Linoleic Acid
now browsing by category
Chronic Pain Due to Mitochondrial Dysfunction, Niacinamide Can Treat It
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/14/chronic-pain-mitochondrial-dysfunction.aspx
Analysis by Dr. Joseph Mercola May 14, 2024

STORY AT-A-GLANCE
- Chronic pain may not be a disorder of its own but a symptom of underlying mitochondrial dysfunction
- Nicotinamide riboside (NR) — a form of vitamin B3 and precursor to nicotinamide adenine dinucleotide (NAD+) — helps relieve chronic pain in mice by improving mitochondrial function
- Niacinamide, another form of vitamin B3 involved in similar cellular processes as NR, may also be useful for relieving chronic pain
- Linoleic acid (LA) in vegetable and seed oils causes mitochondrial dysfunction
- Lowering your intake of LA, which is common in ultraprocessed foods, is one of the most straightforward ways to improve mitochondrial health and, thus, potentially relieve chronic pain
About 21% of U.S. adults suffer from chronic pain, with new cases occurring more often than new cases of other common conditions like diabetes, depression and high blood pressure.1 Pain is considered chronic if it occurs every day or most days over a period of three months or more.
For about 8%, the chronic pain is considered high-impact,2 meaning it limits life or work activities, demonstrating the heavy burden this condition places on those affected. Many reach for dangerous opioid drugs for relief, which suppress mitochondria3 — the last thing you want if you’re struggling with chronic pain.
Chronic Pain Is a Symptom of Mitochondrial Dysfunction
Researchers with Utrecht University in the Netherlands revealed that nicotinamide riboside (NR) — a form of vitamin B3 and precursor to nicotinamide adenine dinucleotide (NAD+), a molecule involved in DNA repair and healthy aging — helps relieve chronic pain in mice4 by improving mitochondrial function.
“Previous research has linked chronic pain to dysfunctional mitochondria, particularly those in specialized nerve cells, called sensory neurons, which detect changes in the environment,” New Scientist reported.5
For the study, an inflammatory substance was injected into the paws of 15 mice, which led to changes in mitochondrial function, even a week later after the inflammation had resolved. The mitochondrial changes were associated with greater pain in the mice, which also had lower levels of NR in the mitochondria of their sensory neurons compared to mice that didn’t experience inflammation.6
NR plays an important role in mitochondrial function, so researchers gave the mice a high dose, which alleviated pain.
“Together these findings indicate two things: first, that inflammation can impair mitochondrial function in sensory neurons and that these impairments increase the risk of chronic pain, even after inflammation has resolved. Second, that taking nicotinamide riboside supplements may help treat this chronic pain by restoring mitochondrial function,” according to New Scientist.7
The study may help shed some light on why some people continue to experience pain even after inflammation has healed, which remains a largely unanswered question. The researchers noticed that even after the initial pain from inflammation goes away, the nerve cells involved in sensing pain still show changes in their mitochondria that disrupt the balance of certain chemicals in the cells.
However, adding the NAD+ precursor NR helped mice recover from pain, even when it was chronic. This suggests that managing mitochondria function in these nerve cells is crucial for overcoming persistent pain after inflammation.
Vitamin B3 for Chronic Pain
As noted in the blog To Extract Knowledge From Matter, which is inspired by the work of the late Ray Peat, niacinamide, another form of vitamin B3 involved in similar cellular processes as NR, may be useful for relieving chronic pain:8
“The study … is one of the first to demonstrate that chronic pain is not an organic disorder of its own, but a symptom of an underlying mitochondrial dysfunction. This not only explain why the intervention with niacinamide worked in alleviating the pain (by improving mitochondrial function), but also why treating chronic pain with opioids is about the worst intervention one could choose.
Why? Because opioids are among the most potent suppressors of mitochondria, which means that as soon as one stops taking them the chronic pain will be much worse, leading to more opioid use and so on — a vicious cycle with usually lethal outcome (overdose).”
In fact, one study found that people who use opioids tend to have fewer mitochondria in their blood. Further, being exposed to the synthetic opioid fentanyl before birth was found to change the number of mitochondria in the blood and the activity of genes related to mitochondria in the nucleus accumbens, a brain area important for feeling pleasure, in young offspring.9
To Extract Knowledge From Matter continued explaining why the featured study’s use of vitamin B3 is superior to opioids for chronic pain:10
“The niacinamide dose used in this study was on the high-side (HED [human equivalent dose] ~35mg/kg daily), but considering it was administrated only once and the pain was completely resolved, it is a low-risk intervention in such doses for humans, especially compared to opioids.
Also, there are prior animal studies showing that lower doses (HED 3mg/kg daily) taken for a few weeks can also relieve chronic pain, which lowers the risk of such intervention even more.”

Save This Article for Later – Get the PDF Now
Your Mitochondria Need Niacinamide
Niacinamide, also known as nicotinamide, is a form of niacin (vitamin B3) that plays a vital role in energy metabolism. It’s essential for the mitochondrial electron transport chain to function. Without it, your mitochondria cannot make energy.
Niacinamide is so important because it is a precursor for NAD+, which is involved in the conversion of food to energy, maintaining DNA integrity and ensuring proper cell function. NAD+ is also a primary fuel for sirtuins, longevity proteins that become depleted with age.
Niacinamide at a dose of 50 milligrams (mg) three times per day will provide the fuel for the rate limiting enzyme for NAD+, NAMPT. Niacinamide also has potent antiobesity effects, can help prevent neurodegeneration and heart failure, and reverse leaky gut.
Niacinamide may also help prevent neurodegeneration by allowing for higher energy levels through energy metabolism in the mitochondria. “There are many studies, going back decades, demonstrating that a drop in NAD+ levels, and thus of NAD/NADH, is a common feature of virtually all neurodegenerative diseases,” writes Peat’s student Georgi Dinkov, a bioenergetic researcher.11
I recommend getting niacinamide in powder form because the lowest available dose in most supplements is 500 mg, and that will decrease NAD+ due to negative feedback on NAMPT, which is the opposite of what you’re looking for. Niacinamide will only cost you about 25 cents a month if you get it as a powder. Typically, 1/64 of a teaspoon of niacinamide powder is about 50 mg.
I also recommend taking one aspirin tablet daily. Aspirin plays a role in mitochondria function12 and also has other health benefits. Importantly, it helps increase the oxidation of glucose as fuel for your body while inhibiting the oxidation of fatty acids, specifically linoleic acid (LA). Dinkov adds:13
“Since aspirin is known to modulate autophagy (raise it when it is abnormally low and lower it when it is abnormally high) and niacinamide is a very effective NAD precursor, it is reasonable to try them in combination that should be synergistic when it comes to protecting the brain (and the entire organism) from diseases and even aging.”
Why Avoiding LA in Ultraprocessed Foods Is Important for Pain Relief
Lowering your LA is the single most important strategy you can take to not only lower reductive stress in your mitochondria but improve your overall health, including relief of chronic pain. LA is an omega-6 fat found in the vegetable oils and seed oils common in most ultraprocessed foods.
The main reason why excess LA causes disease is that it prevents your mitochondria from working well. Mitochondria produce most of your cellular energy in the form of ATP, and without ATP, your cells cannot function and repair themselves normally.
Polyunsaturated fats (PUFAs) such as LA are easily damaged by oxygen in a process called oxidation,14 which triggers the creation of damaging free radicals.15 These, in turn, give rise to advanced lipoxidation end products (ALEs)16 and in the case of omega-6 fats, oxidized LA metabolites (OXLAMs).17,18
These ALEs and OXLAMs then go on to cause mitochondrial dysfunction, which is a hallmark of most chronic disease. In addition to oxidation, inflammation and mitochondrial dysfunction, processed seed oils can also inhibit cardiolipin, an important fat in the inner membrane of your mitochondria.
Cardiolipin is important because it influences the structure of the cristae inside your mitochondria, which is the area where energy production occurs. If cardiolipin is damaged, then the complexes will not be close enough together to form supercomplexes, and thus the mitochondrial energy production will be impaired.
Cardiolipin also works like a cellular alarm system that triggers apoptosis (cell death) by signaling caspase-3 when something goes wrong with the cell. If the cardiolipin is damaged from oxidative stress due to having too much LA, it cannot signal caspase-3, which means apoptosis does not occur.
As a result, dysfunctional cells are allowed to continue to grow, which can turn into a cancerous cell. The type of dietary fat that promotes healthy cardiolipin is omega-3 fat, and the type that destroys it is omega-6, especially LA.
The good news is that dietary changes can improve the composition of fats in your cardiolipin in a matter of weeks, or even days. So, even though it will take years to lower your total body burden of LA, you will likely notice improvements well before then.
How to Optimize Your Mitochondrial Function
To optimize your mitochondrial function, you want to avoid LA as much as possible and increase your intake of omega-3s. Primary sources of LA include seed oils used in cooking, ultraprocessed foods and restaurant foods made with seed oils, condiments, seeds and nuts, most olive oils and avocado oils (due to the high prevalence of adulteration with cheaper seed oils).
Animal foods raised on grains, such as conventional chicken and pork, are also high in LA. Another major culprit that destroys mitochondrial function is excess iron — and almost everyone has too much iron. You can learn more about the health risks of excess iron in my interview with Christy Sutton, D.C. The most effective way to lower your iron is to donate blood two to four times a year.
As mentioned, I also recommend taking 50 mg of niacinamide three times per day. It’s also helpful to make sure you’re getting all the other B vitamins, as they too are crucial for mitochondrial function, especially regular niacin, riboflavin and folate.
Oftentimes, decreased mitochondrial function is due to a deficiency in B vitamins, and that’s easy to fix with a low-dose, high-quality B complex. Usually, when this is the case, improvement can be seen — and felt — within two to three weeks.
- 1, 2 National Institutes of Health May 16, 2023
- 3, 9 Front Psychiatry. 2021 Nov 18:12:737389. doi: 10.3389/fpsyt.2021.737389. eCollection 2021
- 4 Cell Reports Medicine November 8, 2023
- 5, 6, 7 New Scientist November 8, 2023
- 8, 10 Haidut.me February 23, 2024, Chronic pain due to mitochondrial dysfunction, niacinamide can treat it (Archived)
- 11, 13 Haidut.me May 11, 2023, Niacinamide may prevent neurodegeneration (Archived)
- 12 Biochem Biophys Res Commun. 2017 Jan 8; 482(2): 346–351
- 14 Oxid Med Cell Longev. 2014;2014: 360438. doi: 10.1155/2014/360438
- 15 Pharmacognosy Review. 2010;4(8):118-126
- 16 Biochemical Journal. 1982;208(1):129-140
- 17 Nephrol Dialysis Transplant. 2001;16(8):1598-1606
- 18 Free Radical Biol Med. 1992;13:341-390
Symptoms of Diverticulitis and How to Treat It
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/10/diverticulitis-symptoms.aspx
Analysis by Dr. Joseph Mercola May 10, 2024

STORY AT-A-GLANCE
- Diverticulitis is an inflammation or infection of small pouches called diverticula that can develop along the walls of your intestines
- Diverticulitis can cause abdominal pain, constipation, diarrhea, nausea, vomiting, fever and rectal bleeding
- More severe cases can lead to serious complications, including abscesses, fistulas and intestinal blockage
- Restoring your gut microflora and cellular energy production are key to resolving diverticulitis
- Eating foods that support Akkermansia, such as polyphenol-rich fruit, and other beneficial bacteria, and avoiding linoleic acid, are important for diverticulitis; rectal CO2 insufflation may also help
Diverticulitis is an inflammation or infection of small pouches called diverticula that can develop along the walls of your intestines. The formation of these pouches is known as diverticulosis, a common condition that typically causes few or no symptoms. However, when these pouches become inflamed or infected, it leads to diverticulitis, which can be painful and may lead to serious complications.
Diverticulosis is common in the U.S. and other parts of the world where heavily processed diets are the norm. It’s estimated that 30% of Americans over 50 have diverticulosis, which rises to 50% of those over 60% and 75% in people over 80.1
Most often, the condition affects the sigmoid colon, a section of the large intestine near the end of the digestive tract. Among those with diverticulosis, about 4% develop diverticulitis.2
What Are the Symptoms of Diverticulitis?
You can have diverticulosis and not know it, since it often causes no symptoms. But in the case of diverticulitis, it’s typically a different story. Common symptoms include:3
• Abdominal pain — When diverticula become inflamed, they cause the surrounding tissues in the intestinal wall to also become inflamed. This inflammation can lead to pain that’s typically felt in the lower left side of the abdomen and may be severe.
The pain may also spread to your pelvis and back. In people of Asian descent, diverticulosis may occur more often in the first part of the colon, so diverticulitis in that region may cause pain in the upper right abdomen.4
• Bowel changes — The inflammation associated with diverticulitis can affect the movement of the bowel, leading to disruptions in the normal rhythm of digestion. This can result in constipation or diarrhea, along with bloating and gas. Feelings of fullness can also occur.
• Nausea and vomiting — Gastrointestinal irritation may lead to nausea while increased movement of the intestines in an attempt to expel irritants and bacteria may lead to vomiting. In more severe cases, the inflammation can lead to a partial or complete blockage of the intestine, which can trigger vomiting.
• Fever — When diverticula become inflamed, they can also become infected, usually by bacteria. The fever is a sign that your body is actively fighting an infection.
• Rectal bleeding — As diverticulitis progresses, the inflamed diverticula can cause small blood vessels to stretch and rupture, leading to bleeding. This can result in blood appearing in the stool.
Diverticulitis can be classified as acute, which occurs suddenly and often causes intense abdominal pain, fever and nausea, or chronic, with persistent symptoms due to the ongoing inflammation.
More severe cases can lead to serious complications, which are sometimes the first sign of the disease. Each year, about 200,000 people are hospitalized due to diverticulitis, while 71,000 are hospitalized with diverticular bleeding.5 Complications may include:6
- Abscesses
- Perforation, or a hole, in your colon
- Fistulas, an abnormal tunnel between your colon and another area of the body, such as your bladder
- Intestinal blockages
- Peritonitis, an infection of the abdominal cavity
What Causes Diverticulitis?
Certain genes may increase your risk of diverticulitis, but lifestyle factors also play a role, including:7
- Eating ultraprocessed foods
- Inactivity
- Using certain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids
- Obesity
- Smoking
While a number of factors contribute to diverticulitis, a disrupted microbiome and eating a highly processed, low-fiber diet are chief among them. Dietary fiber is crucial for maintaining a healthy digestive system. It helps to bulk up your stool and softens it, making it easier to pass through the colon. This reduces the strain and pressure in your colon during bowel movements.
When your diet lacks sufficient fiber, your stools become harder and smaller, requiring your colon to exert more pressure to move them along. This increased pressure can cause your colon’s muscular wall to develop weak spots.
Over time, the continuous pressure may force the inner lining of your colon through these weak spots in the muscle layer, forming diverticula. Further, a diet low in fiber keeps the intra-colonic pressure elevated because of the harder, smaller stools and the greater effort needed to expel them.
This sustained high pressure is believed to not only contribute to the formation of diverticula but also increase the risk of these diverticula becoming inflamed or infected, leading to diverticulitis. As noted in Cureus:8
“Many theories have been suggested for the different etiologies of diverticular disease, and the most common cause is believed to be a low-fiber diet. It is believed that diets low in fibers are associated with increased intra-colonic pressure, which leads to diverticula formation.”

Save This Article for Later – Get the PDF Now
Diverticulitis Linked to Gut Microbiome Composition
Researchers with Massachusetts General Hospital and Harvard Medical School in collected stool samples from 121 women with severe diverticulitis and compared them to stool samples from 121 women without the condition.9 They conducted a detailed analysis of the overall microbial community structures and metabolomic profiles in the collected samples, revealing significant differences between the groups.
Women with diverticulitis had more pro-inflammatory agents such as the microbe Ruminococcus gnavus, 1,7-dimethyluric acid and various histidine-related metabolites. There was also a notable depletion of butyrate-producing bacteria, which are known for their anti-inflammatory properties, as well as a reduction in anti-inflammatory ceramides.
The study highlighted how microbial composition may influence the protective association between a fiber-rich diet and diverticulitis, suggesting that dietary fiber’s protective effects can be significantly altered by a person’s existing gut microbiota composition. A review published in the Journal of Personalized Medicine further described gut microbiota’s potential role in diverticulitis, noting:10
“Changes in microbiota composition have been observed in patients who were developing acute diverticulitis, with a reduction of taxa with anti-inflammatory activity, such as Clostridium cluster IV, Lactobacilli and Bacteroides.
Recent observations supported that a dysbiosis characterized by decreased presence of anti-inflammatory bacterial species might be linked to mucosal inflammation, and a vicious cycle results from a mucosal inflammation driving dysbiosis at the same time.
An alteration in gut microbiota can lead to an altered activation of nerve fibers, and subsequent neuronal and muscular dysfunction, thus favoring abdominal symptoms’ development.”
Restoring Your Gut Microflora and Cellular Energy Production Are Key
Dysbiosis, or an imbalance of microbial communities, in your gut plays a central role in the development of diverticulitis.11 A balanced gut microbiota helps reduce inflammation in the colon. Certain beneficial bacteria produce short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties. These SCFAs help maintain the health of the colon lining and prevent inflammation that can lead to diverticulitis.
A robust intestinal barrier can also prevent bacterial fragments from entering your bloodstream, whereas a compromised barrier allows these harmful fragments through while blocking SCFAs. However, most people have dysfunctional mitochondria, and if you don’t have enough mitochondria, you can’t create cellular energy efficiently enough to ensure a healthy gastrointestinal tract.
Your gut contains primarily two types of gram-negative bacteria: beneficial and pathogenic. The beneficial ones include obligate anaerobes, which cannot survive in the presence of oxygen and are essential for health. They do not produce harmful endotoxins and contribute positively by producing SCFAs like butyrate, propionate and glucagon-like peptide-1 (GLP-1).
Proper gut function requires energy to maintain an oxygen-free environment in the large intestine, where 99% of gut microbes reside. Insufficient energy leads to oxygen leakage, which harms obligate anaerobes while not impacting the facultative anaerobes, thereby disrupting the balance of the microbiome.
Pathogenic bacteria, or facultative anaerobes, can survive in oxygen and are harmful, as they possess endotoxins in their cell walls. In short, enhancing mitochondrial energy production is crucial for maintaining a healthy gut environment. When you do that, it helps suppress the growth of pathogenic bacteria and support beneficial microbial populations, which in turns reduces your risk of diverticulitis.
Widespread use of antibiotics can also disrupt the microbiome by killing both beneficial and harmful bacteria, leading to a dominance of pathogenic bacteria which produce harmful endotoxins. Optimizing your mitochondrial function is, however, one of the most important strategies you can do to optimize your cellular energy, so it’s at the core of almost everything that you do to improve your health.
How to Restructure Your Microbiome
Akkermansia, highly beneficial bacteria in your large intestine, plays a crucial role in maintaining gut health and should constitute about 10% of the gut microbiome. However, it is absent in many individuals, likely due to inadequate mitochondrial function and resultant oxygen leakage in the gut.
Eating foods that support Akkermansia, such as polyphenol-rich fruit, and other beneficial bacteria, and avoiding foods like linoleic acid — found in vegetable and seed oils in most processed foods — that destroy these bacteria, will help to restructure your microbiome in a positive way. You can also use an Akkermansia probiotic supplement.
One of the reasons Akkermansia is so important is because it produces mucin, a thick, protective gel-like substance that lines various parts of the body, including the gastrointestinal tract. Mucin forms a protective barrier on the gut lining, shielding the epithelial cells of the intestinal wall from mechanical damage, chemical irritation from stomach acids and digestive enzymes, and pathogenic organisms like bacteria and viruses.
Mucin also supports the immune system by trapping potential pathogens and other foreign particles, which are then expelled from the body through the digestive process. It also contains antibodies and antimicrobial peptides that help fight off infections.
Lastly, mucin serves as a food source for other beneficial gut bacteria. This relationship is essential for digestive health, as the bacteria fed by Akkermansia aid in digestion, produce essential nutrients and help maintain an overall balance of gut flora.
Increasing CO2 Likely Beneficial
Carbon dioxide (CO2) is a driver of energy production, as it improves the delivery of oxygen into your cells. While CO2 is typically thought of as nothing more than a harmful waste product of respiration, and a “pollutant” that endangers the planet, the reality is that it’s essential for most life on Earth. In fact, CO2 appears to be a more fundamental component of living matter than oxygen.12
“Really, every condition you can think of, both physiological and mental, can be remediated, and in many cases cured, by increasing endogenous CO2 production and decreasing degradation,” Georgi Dinkov says.
Importantly, CO2 allows for more efficient energy production in your mitochondria, which is why people who live or spend time at higher altitudes tend to be healthier and have fewer chronic health problems such as asthma. The reason for this is because the pressure of CO2 relative to oxygen is greater at higher altitudes.
In order to have sufficient CO2 production, you need healthy mitochondria, because CO2 is produced exclusively in the Krebs cycle in the mitochondria. If you have mitochondrial dysfunction, if you’re hypothyroid or have high levels of inflammation, as is the case in diverticulitis, then you will not be producing enough CO2.
While it’s important to optimize your endogenous (internal) production of CO2, exogenous delivery or supplementation will produce the greatest benefits, as you can deliver far greater amounts than your body can produce. Such strategies include:
- Breathing into a paper bag
- Drinking carbonated water and other carbonated beverages
- CO2 baths
- A special suit into which CO2 is pumped
- Taking small amounts of baking soda in your drinking water
A book written in 1905 by Achilles Rose, M.D. discusses delivery by rectal insufflation. During rectal CO2 insufflation, a small tube or catheter is inserted into the rectum, and a controlled amount of CO2 is gently infused. This is a highly effective way to deliver CO2.
I am currently in the process of setting up an IRB (Institutional Review Board) approved study that will be exploring the therapeutic value of administering CO2 gas rectally to reverse the damage caused by decades of excess LA consumption that caused a radical decrease in mitochondrial function and cellular energy production resulting in a compromised oxygen gradient differential in the large intestine that allows pathogenic bacteria to become squatters and occupy the spaces of the obligate anaerobic species like Akkermansia that provide benefits and do not produce toxic endotoxin.
- 1, 3, 4 Cleveland Clinic, Diverticulosis
- 2 Cleveland Clinic, Diverticulitis
- 5, 6 National Institute of Diabetes and Digestive and Kidney Diseases, Definition & Facts for Diverticular Disease
- 7 National Institute of Diabetes and Digestive and Kidney Diseases, Symptoms & Causes of Diverticular Disease
- 8 Cureus. 2023 Aug; 15(8): e43158
- 9 Nat Commun. 2024 Apr 29;15(1):3612. doi: 10.1038/s41467-024-47859-4
- 10 J Pers Med. 2021 Apr; 11(4): 298
- 11 Neurogastroenterology & Motility May 27, 2023
- 12 Conscious Breathing Carbon Dioxide, Physiology
The Effects of Ozempic and Other Weight Loss Injections
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/08/ozempic-weight-loss-injections-health-effects.aspx
Analysis by Dr. Joseph Mercola May 08, 2024
STORY AT-A-GLANCE
- Semaglutide — the active ingredient in not only Ozempic and Wegovy but also Saxenda and Victoza — is touted as a wonder drug for weight loss but comes with serious side effects
- Research from the University of British Columbia revealed the drugs are associated with an increased risk of stomach paralysis, pancreatitis and bowel obstruction
- The Therapeutic Goods Administration, Australia’s regulatory authority for drugs, is investigating at least three deaths linked to Ozempic and other weight loss injections
- New understandings of how Ozempic works suggest its mechanisms may have more to do with your brain than your gut
- Drugs like Ozempic closely mimic the effects of Akkermansia, a key bacteria strain in your microbiome; naturally increasing Akkermansia may have weight loss effects
They’re described as wonder drugs for weight loss, but semaglutide — sold under the name Ozempic as a diabetes drug and, in a higher dose, under the name Wegovy as a weight loss drug — and other weight loss injections have a dark side.
Semaglutide — the active ingredient in not only Ozempic and Wegovy but also Saxenda and Victoza — touts weight loss rates of 14.9% among adults with obesity,1 and social media is filled with success stories of dramatic weight loss from the drugs.
Dr. Katherine Samaras, professor of medicine and endocrinologist at St. Vincent’s Hospital in Darlinghurst, Australia, told 60 Minutes that Ozempic is game-changing and transformative, going so far as to compare it to the introduction of penicillin.2
But around the world, families are mourning the loss of loved ones who took the drugs and paid the ultimate price. Others are dealing with debilitating side effects, some of them permanent.
Ozempic Slows the Passage of Food Through Your Stomach
Semaglutide is a glucagon-like peptide 1 receptor agonists (GLP-1RAs). As a peptide hormone, GLP-1 is, among other things, part of a group of incretin hormones, which are released when you eat to regulate insulin, along with many other functions.3
Along with affecting insulin, GLP-1 may influence the nervous system, leading to an appetite-reducing response. However, one of their mechanisms is delayed gastric emptying, meaning they radically slow the passage of food through your stomach. This makes you feel fuller longer, but if food moves too slowly, serious consequences result.
Delayed gastric emptying is the hallmark of gastroparesis, or stomach paralysis — a known side effect of the drugs. Nausea and vomiting are common symptoms of gastroparesis that occur so frequently among Ozempic users that social media influencers are now advising people on how to manage these and other side effects.4
Due to the delayed stomach emptying that occurs with semaglutide, the American Society of Anesthesiologists (ASA) released a warning for those taking the drugs before elective surgery.5
They suggest stopping this and other GLP-1 receptor agonists before the procedure, as they could increase the risk of complications associated with anesthesia — namely that you could regurgitate food that’s still sitting in your stomach, even if you’ve fasted appropriately.
Weight Loss Injections Linked to Serious Gastrointestinal Conditions
Research from the University of British Columbia revealed that GLP-1 agonists are associated with an increased risk of several serious health conditions, including stomach paralysis, pancreatitis and bowel obstruction.6 Compared to those using the weight loss drugs bupropion-naltrexone, those taking GLP-1 agonists like Ozempic had a:7
- 9.09 times higher risk of pancreatitis
- 4.22 times higher risk of bowel obstruction
- 3.67 times higher risk of gastroparesis
“These drugs are becoming increasingly accessible, and it is concerning that, in some cases, people can simply go online and order these kinds of medications when they may not have a full understanding of what could potentially happen. This goes directly against the mantra of informed consent,” said study author Mohit Sodhi.8

Save This Article for Later – Get the PDF Now
Ozempic Linked to Fatal Intestinal Blockages
These trendy weight loss medications cause other significant risks as well and may even cause a potentially fatal intestinal obstruction. Diabetic patients who use the drugs have a 4.5 times higher risk of intestinal obstruction than those using other medications. A study of 25,617 people also found use of GLP-1 agonists increases the rate of intestinal obstruction by 3.5-fold.9
The drugs were also found to increase the length and weight of the small intestine in animal studies, while in humans they may increase intestinal length and villus height; villi are the hairlike projections inside the small intestine that help absorb nutrients. Writing in Acta Pharmaceutica Sinica B, researchers explained how this could seriously affect intestinal function, increasing obstruction risk:10
“Because GLP-1RAs [GLP-1 receptor agonists] could cause continuous increases in the intestinal length and villus height, the small intestine may become as inelastic and fibrotic as a loose spring, leading to long-term upper intestinal obstruction …”
60 Minutes covered the story of Trish Webster, a woman from Australia who died from an intestinal blockage after using Ozempic and Saxenda for five months. She experienced diarrhea, constant nausea and vomiting while taking the drugs before eventually collapsing. Her cause of death is listed as “acute gastrointestinal illness.”11
The Therapeutic Goods Administration, Australia’s regulatory authority for therapeutic goods, including drugs and medical devices, is investigating at least three deaths linked to Ozempic and other weight loss injections. Tim Ramsay died just 19 days after using Saxenda, while a 39-year-old woman also died after taking Ozempic injections to lose weight.12
In other cases, those who have taken the injections experience life-changing side effects making them wish they never touched the drugs. Joanne Knight had been taking Ozempic for about two years when she became unable to swallow food. The reason? Her stomach was full of food. Violent vomiting and constant nausea followed, along with a diagnosis of severe gastroparesis.13
“I wish I never touched it. I wish I’d never heard of it in my life,” Knight told CNN. “This medicine made my life hell. So much hell. It has cost me money. It cost me a lot of stress; it cost me days and nights and trips with my family. It’s cost me a lot, and it’s not worth it. The price is too high.”14
Ozempic May Work via Your Brain
New understandings of how Ozempic works suggest its mechanisms may have more to do with your brain than your gut. The Atlantic reported:15
“In recent years, studies have shown that GLP-1 from the gut breaks down quickly and has little effect on our appetites. But the hormone and its receptors are naturally present in many parts of the brain too. These brain receptors are likely the reason the GLP-1 drugs can curb the desire to eat — but also, anecdotally, curb other desires as well. The weight-loss drugs are ultimately drugs for the brain.
Obesity medications differ in a key way from the natural molecule they’re meant to mimic: They last a lot longer. GLP-1 released in the gut has a half-life of just minutes in the bloodstream, whereas semaglutide and tirzepatide [Eli Lilly’s obesity drug] have half-lives measured in days. This is by design. Both drugs were specifically engineered to resist degradation, so that they need to be injected only once a week.
… The medications are also given at levels much higher than natural GLP-1 ever reaches in the bloodstream … By indiscriminately flooding the body with long-lasting molecules, the injections likely allow engineered GLP-1 drugs to penetrate parts of the body that the natural gut hormone cannot — namely, deep in the brain.”
Semaglutide’s brain effects may explain why many people taking the drugs also lose the desire to engage in behaviors like drinking alcohol, shopping and smoking. Research published in The Journal of Clinical Investigation Insight found semaglutide reduces alcohol drinking in rodents and modulates central gamma-aminobutyric acid (GABA) neurotransmission.16
“Growing evidence indicates that the glucagon-like peptide-1 (GLP-1) system is involved in the neurobiology of addictive behaviors,” the researchers explained.17 While the drugs are now being looked at for treatment of alcohol use disorder and other conditions, the consequences of allowing such drugs to tinker with the brain are unknown.
Ozempic Mimics Akkermansia
Akkermansia muciniphila is a bacterium that’s a keystone strain in your microbiome. Having higher levels of Akkermansia is associated with lower weight, while lower levels of Akkermansia are linked to obesity. Interestingly enough, drugs like Ozempic closely mimic the effects of Akkermansia. In my interview with Dr. Colleen Cutcliffe, a microbiome scientist and the CEO and cofounder of Pendulum, a company that creates microbiome products, she explains:
“What happens in your body naturally, if you’ve got all the right microbes, is that you eat a meal, your microbiome metabolizes that food and generates postbiotics [excretions from beneficial bacteria] like butyrate [and] a protein called P9. Some of these postbiotics then signal your body to produce GLP-1.
All that signaling is happening from the microbiome directly to the L cells. And so you eat a meal, your microbiome digests them, these postbiotics get created and tell your L cells, ‘Hey, go produce GLP-1,’ and then you get a spike in GLP-1 in your body.
GLP-1 stimulates your body too. It says, ‘We’ve got to metabolize the sugar in the bloodstream, release insulin.’ It also signals to your brain, ‘We just ate, we’re full, we don’t need to eat again.’ After a period of time, GLP-1 goes down — until the next time you eat a meal. Then it spikes again.
So that’s the natural way of things. There are only two strains that have been published, to date, that have been shown to be able to stimulate L cells to produce GLP-1, and one of them is Akkermansia. It actually secretes three different [postbiotics] that stimulate L cells to produce GLP-1.
So, what’s been found is that if you are low or missing Akkermansia, your body is not naturally producing as much GLP-1 as it’s supposed to be. By giving people back Akkermansia, you can now have these physiological benefits of reducing A1C and lowering blood glucose spikes.
To be clear, the natural GLP-1 you produce is different from the drug. The drug is a mimic. It’s an analog. It looks like GLP-1. It gets injected into the bloodstream directly, which means that rather than the natural spike after you eat [followed by a decline], the [drug] is keeping those levels really high all the time.
So, this signaling of ‘we got to metabolize sugar in the blood and we’re full, we just ate’ is going on constantly. That’s why people experience these incredible, amazing overnight effects because that’s how those drugs are working. But if you actually have the right microbes, you can generate your body’s natural GLP-1 and get back into this natural cycle.”
A Natural Ozempic?
Certain foods will naturally feed beneficial microbes that may help with weight loss naturally. Polyphenol-containing fruits, vegetables and berries, for example, have been shown to increase Akkermansia levels. I suspect a high-quality Akkermansia probiotic supplement may significantly accelerate the process, but the good news is the abundance of Akkermansia in your gut can easily be enhanced through dietary interventions, such as:18
- Supplementing with probiotics and prebiotics that promote Akkermansia growth in the gut — Specific examples include Lactobacillus rhamnosus, Bifidobacterium animalis, Lactococcus lactis (probiotics) and oral fructo-oligosaccharides (oligofructose or FOS, a common prebiotic).
- Eating more fiber — The short-chain fatty acids that form from fiber as it ferments in your intestines feed beneficial bacteria, including Akkermansia.
- Increasing FODMAP’s in your diet — FODMAP refers to “fermentable oligo-, di- and mono-saccharides and polyols,” which include fructose (found in fresh fruit) and lactose (found in milk and other dairy products).
- Boosting intake of dietary polyphenols — Black tea, red wine grape extract, cranberry extract and Concord grape, specifically, have all been shown to significantly promote growth of Akkermansia.
- Avoiding alcohol and high-fat diets — Several studies have shown a correlation between high-fat diets (60% fat or higher) and significantly reduced Akkermansia colonization. Ditto for alcohol consumption.
Berberine is another compound that’s described as “nature’s Ozempic.” It’s a chemical found in plants such as goldenseal and European barberry.19 Research shows it helps regulate blood sugar and may help with weight loss.
A 2022 systematic review of the literature demonstrated that supplementing with berberine had a positive effect on lipid profile, fasting blood glucose, obesity parameters and systolic blood pressure.20
In a 2022 paper in Frontiers in Cellular and Infection Microbiology, the researchers wrote, “Studies have shown that BBR [berberine] can alleviate the pathological conditions of metabolic disorders, and the mechanism is related to the regulation of gut microbiota … meanwhile, the structure and function of gut microbiota also changed after intervention by berberine.”21
Berberine may also delay the amount of time it takes for food to pass through your small intestine,22 and preferentially nourish microbes that produce beneficial short-chain fatty acids known to have many health benefits.23 A comprehensive approach is necessary to lose weight and maintain it naturally, however, and this involves dietary changes.
Collectively, consuming too much linoleic acid (LA) is the primary factor driving the overweight and obesity epidemics. LA is the most common omega-6 fat found in seed oils like soybean, cottonseed, sunflower, rapeseed (canola), corn and safflower. Reducing your intake of seed oils and all processed foods is a powerful way to support a healthy weight. Ideally, consider cutting LA down to below 5 grams per day.
- 1 N Engl J Med 2021; 384:989-1002
- 2 YouTube, 60 Minutes Australia February 11, 2024, 4:22
- 3 SubStack, Modern Discontent March 28, 2023
- 4 TIME March 7, 2024 (Archived)
- 5 American Society of Anesthesiologists June 29, 2023
- 6 JAMA. 2023;330(18):1795-1797. doi: 10.1001/jama.2023.19574
- 7, 8 The University of British Columbia October 5, 2023
- 9, 10 Acta Pharmaceutica Sinica B May 2023, Volume 13, Issue 5, Pages 2291-2293
- 11 Diabetes.co.uk November 18, 2023
- 12 60 Minutes Australia February 2024
- 13, 14 CNN Health July 25, 2023
- 15 The Atlantic March 5, 2024
- 16, 17 The Journal of Clinical Investigation Insight May 16, 2023
- 18 Nature Microbiology April 5, 2021; 6: 563-573
- 19 MedlinePlus, Berberine
- 20 Frontiers in Nutrition, 2022; 9
- 21 Frontiers in Cellular and Infection Microbiology, 2022;12(854885)
- 22 Zhongguo Zhong Xi Yi Jie He Za Zhi. 1994;14(12)
- 23 Scientific Reports 2015;5
Natural Therapies for Cystic Fibrosis
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/02/natural-therapies-for-cystic-fibrosis.aspx
Analysis by Dr. Joseph Mercola May 02, 2024

STORY AT-A-GLANCE
- Cystic fibrosis (CF) is a severe genetic disorder marked by excessive, thick mucus in the lungs and other organs, leading to chronic inflammation and reduced lung function, necessitating daily breathing treatments
- Nutritional support, including vitamins A, C, E, zinc, omega-3 (DHA), garlic, ginseng and curcumin, is commonly recommended for CF patients
- Vitamin D deficiency is notably prevalent among CF patients, affecting their lung function and overall disease progression; maintaining a vitamin D level of at least 60 ng/mL is recommended for mitigating these effects
- N-acetylcysteine (NAC) has emerged as a significant antioxidant in CF management, helping to reduce inflammation, break down mucus, enhance antibiotic effectiveness, and support immune response
- Reducing dietary intake of linoleic acid (LA) is advised for CF patients due to its potential to exacerbate disease symptoms through mitochondrial dysfunction
Cystic fibrosis (CF) is a progressive and terminal genetic disease that causes an overproduction and buildup of thick, sticky mucus in the lungs and other organs that lead to chronic inflammation and, eventually, a deterioration of lung function.
The disease requires daily breathing treatment for up to five hours a day, and many CF patients end up spending a lot of time in the hospital due to respiratory distress and chronic infections. Pancreatic and gastrointestinal complications, including malabsorption of proteins and fats, and chronic liver disease are also common. The median survival age is about 35 years.1
A 2012 paper2 in the Journal of Pharmacy Practice reviewed several of the most commonly recommended nutritional supports for those with CF, including vitamins A, C and E, zinc, omega-3 docosahexaenoic (DHA), garlic, ginseng and curcumin.
According to this paper, 75% of CF patients routinely use complementary and alternative medicine (CAM) in addition to their regular treatment, so it’s important for health professionals to be familiar with these options.
More recently, a scientific review3 published in 2022 highlighted the role of N-acetylcysteine (NAC) in the clinical management of CF. Removing all linoleic acid (LA) from your diet and optimizing your vitamin D level are two additional foundational recommendations that I will go over here.
Vitamins A, C and E and Zinc
Many CF patients have poor absorption of fat-soluble vitamins such as A and E, due to malabsorption of fats. For this reason, supplementation with these vitamins is often recommended. As a rule, patients are advised to consume between 120% and 150% of the recommended daily allowance (RDA) of nutrients to prevent premature death from malnutrition.4
The Journal of Pharmacy Practice paper5 cites research from 2001, which found that CF patients who received 1 milligram of beta-carotene per kilo of bodyweight per day (up to 50 mg per day) for three months, followed by a daily dose of 10 mg for another three months, experienced “a statistically significant decrease in the number of days of treatment with systemic antibiotics.”
Zinc supplementation at a dose of 30 mg per day has also been shown to reduce the average days of antibiotic use, and a pediatric study using an antioxidant-rich multivitamin supplement containing vitamins A, C, E and zinc and other micronutrients found “modest improvement” in lung function.
How to Select a Good Vitamin Supplement
Vitamin A (retinol) should not be confused with beta-carotene, which is pre-vitamin A that gets converted into vitamin A in your liver. To use beta-carotene, you need to have a well-functioning digestive tract and sufficient bile produced by your gallbladder. Specific enzymes are also needed to break down the carotene for the conversion into retinol to occur.
Most people have poor gut health, and this is particularly true for CF patients, which makes beta-carotene a poor alternative as a primary source of vitamin A. Retinol — preformed vitamin A — is found in animal products such as grass fed meat and poultry, liver, fish and raw organic dairy products like butter. This is the form of vitamin A your body can use, so make sure the vitamin A you buy specifies “retinol” or “retinoic acid,” and not just “vitamin A” or “beta-carotene.”
When it comes to vitamin C, you want to make sure it’s liposomal, as it will allow you to take higher dosages without causing loose stools. It’s also absorbed better.
While healthy people can typically get enough vitamin C from food such as red pepper, broccoli, kiwi, strawberries, citrus fruits, camu camu, rose hips or acerola cherries, if you’re ill, you need far more than what can be obtained from food (possibly except for acerola cherry, which contains 80 mg of vitamin C per cherry).
Selecting a natural supplement is particularly important when it comes to vitamin E. Studies have demonstrated that synthetic vitamin E has the opposite effect of natural vitamin E, such as increasing the risk of certain cancers rather than lowering it,6,7,8 for example. So, it’s important to make sure you’re getting a natural version.
What you’re looking for is “d alpha tocopherol.” Avoid all synthetic forms such as succinate, acetate and the racemic DL isomer. You want the pure D isomer, which is what your body can use. There are also other vitamin E isomers, and you want the complete spectrum of tocotrienols, specifically the beta, gamma, and delta types of vitamin E, in the effective D isomer.

Save This Article for Later – Get the PDF Now
Vitamin D
Vitamin D also plays a crucial role in the health and management of CF, offering several benefits backed by scientific research. A systematic review and meta-analysis9 published in January 2024 revealed that CF patients typically have significantly lower levels of vitamin D compared to healthy controls, both in childhood/adolescence and adulthood.
The prevalence of vitamin D levels considered insufficient (20–30 ng/mL) in CF patients was found to be 36% among pediatrics and adolescents and 63% among adults. Twenty-seven percent of pediatric/adolescent CF patients and 35% of adults had vitamin D levels of below 20 ng/mL, which is a severe deficiency state.
Ideally, you’d want a vitamin D level of at least 60 ng/mL year-round. To reach that level, I recommend daily walks with minimal clothing for 30 minutes before and after solar noon, for a total of one hour. During summertime, that would be right around 1 pm.
While oral vitamin D3 supplementation is an option if you cannot get enough sun exposure, you’ll miss out on many of the other health benefits that sun exposure provides. You also need to make sure you’re taking vitamin K2 and magnesium when using oral supplementation.
How Vitamin D Deficiency Impacts CF
Another study10 focused on the relationship between vitamin D levels and lung function in CF patients, specifically through the lung clearance index (LCI), a measure of lung function. The study found a strong negative correlation between vitamin D levels and LCI, indicating that lower vitamin D levels are associated with worse lung function.
It also noted that vitamin D deficiency could be particularly detrimental in patients with comorbidities such as cystic fibrosis-related diabetes (CFRD) and cystic fibrosis liver disease (CFLD).
Additionally, a pilot study11 published in 2019 investigated the immunomodulatory effects of vitamin D on pro-inflammatory cytokines in the airways of CF patients infected by Pseudomonas aeruginosa.
They found that supplementation with vitamin D led to a decrease in the levels of interleukins IL-17A and IL-23 in the exhaled breath condensate (EBC), indicating a reduction in inflammation.
These cytokines are known to play roles in the body’s inflammatory response, suggesting that vitamin D supplementation can help modulate the immune response in CF patients, potentially mitigating lung damage caused by chronic infections.
These findings collectively underscore the importance of monitoring and managing vitamin D levels in CF patients, not only for bone health but also for its potential benefits in improving lung function, reducing inflammation, and enhancing the body’s response to infections.
N-acetylcysteine (NAC)
NAC is a precursor to your body’s production of glutathione (GSH), also has an important role in the management of CF.12 As noted in the journal Pharmaceuticals:13
“[NAC] has been known for a long time as a powerful antioxidant and as an antidote for paracetamol overdose. However, other activities related to this molecule have been discovered over the years, making it a promising drug for diseases such as cystic fibrosis (CF).
Its antioxidant activity plays a key role in CF airway inflammation and redox imbalance. Furthermore, this molecule appears to play an important role in the prevention and eradication of biofilms resulting from CF airway infections, in particular that of Pseudomonas aeruginosa …
To do this, NAC can act alone, but it can also be used as an adjuvant molecule to known drugs (antibiotics/anti-inflammatories) to increase their activity.”
Here’s a quick overview of how NAC can be beneficial for CF patients, drawing on its various mechanisms:14
| Fighting oxidative stress — There’s a battle between damaging oxidative substances (ROS) and the body’s antioxidants. NAC steps in as a reinforcement, helping to boost the body’s antioxidant levels, especially glutathione (GSH). This helps to mitigate the damage caused by oxidative stress, which can worsen CF conditions. |
| Reducing inflammation — CF lungs are often inflamed, partly due to overactive immune responses that attract too many neutrophils (a type of white blood cell) to the site. These neutrophils release substances that can damage lung tissue. NAC helps calm this overreaction, reducing inflammation by modulating the production of molecules like cytokines that drive the inflammatory process. |
| Breaking down mucus — The thick mucus in CF can trap bacteria, creating biofilms that are hard to treat. NAC can break the sulfur bonds in the mucus, making it less sticky and easier to clear from the lungs. This action helps disrupt the biofilm structure, allowing antibiotics to reach and kill bacteria more effectively. |
| Enhancing antibiotic effectiveness — The presence of biofilms and thick mucus in CF lungs can make bacteria resistant to antibiotics. NAC can make these bacteria more susceptible to antibiotics by breaking down the biofilms. It can also work synergistically with certain antibiotics, improving their ability to kill bacteria. |
| Acting against bacteria directly — Even though NAC is not an antibiotic, it has properties that can directly inhibit the growth of bacteria and their ability to form biofilms. This adds an extra layer of defense against lung infections. |
| Supporting healthy immune responses — By reducing the oxidative stress and helping to manage the inflammatory response, NAC can indirectly support the body’s immune system, making it more effective at fighting off infections without causing additional damage to lung tissues. |
| Improving cell function — On a cellular level, NAC might help correct some of the dysfunction caused by the CF mutation. It has been suggested that NAC can help with the maturation and function of CFTR proteins, which are faulty in CF, thereby helping to alleviate some of the symptoms. |
Omega-3
Omega-3 is also thought to be important for CF patients because deficiency has been linked to worsened pulmonary and GI symptoms, as well as CF progression. DHA, in particular, is important, as it has a beneficial impact on lung function. Previous research has concluded that doses up to 50 mg of DHA per kilo of bodyweight is safe for CF patients.15
When it comes to omega-3, I recommend trying to get most of it from omega-3-rich seafood, such as wild-caught Alaskan salmon, herring, sardines, mackerel and anchovies. If using a supplement, avoid synthetic fish oils and opt for krill oil instead.
Herbal Remedies
Herbal remedies recommended for CF include:16
- Garlic, which has antibacterial effects.
- Ginseng, which has antioxidant, antimicrobial and immune modulating effects. Aqueous extract of ginseng has been shown to be effective in inhibiting P aeruginosa, a bacteria often involved in chronic pulmonary infections, including antibiotic-resistant strains.
- Curcumin, which has antioxidant properties. Limited data also suggests it may increase CFTR-regulated channel activity in CF patients. CFTR is a protein that, when dysfunctional, results in the development of CF symptoms.
Eliminate Linoleic Acid From Your Diet
As important as supplementing certain nutrients might be, CF patients must also be vigilant about avoiding certain things. As explained in my in-depth review, “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” linoleic acid (LA) — an omega-6 polyunsaturated fat (PUFA) — acts as a mitochondrial poison and the primary contributor to all chronic disease.
If you have CF, I strongly advise you to eliminate as much LA from your diet as humanly possible. While LA is found in most foods, by eliminating processed foods, condiments, seed oils for cooking, fast food and restaurant food, and conventionally raised pork, chicken and eggs, you can get your LA intake below 5% of daily calories, which is about what our ancestors used to get.
While there are no studies detailing direct harm caused by LA in CF, dysfunctional lipid metabolism, including LA metabolism, is a characteristic of CF. So, there appears to be a complex interaction with LA that could influence disease outcomes.
Excess LA is a primary driver of mitochondrial dysfunction, and well-functioning mitochondria are a prerequisite for health and disease prevention.
That said, considering excess LA is a primary driver of mitochondrial dysfunction, there’s every reason to believe that it will have a detrimental impact on CF. After all, health and disease prevention require you to have well-functioning mitochondria. It’s as foundational as you can get.
If you’re not sure how much you’re eating, enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake. Cronometer will tell you how much omega-6 you’re getting from your food down to the 10th of a gram, and you can assume 90% of that is LA. Anything over 10 grams of LA is likely to cause problems.
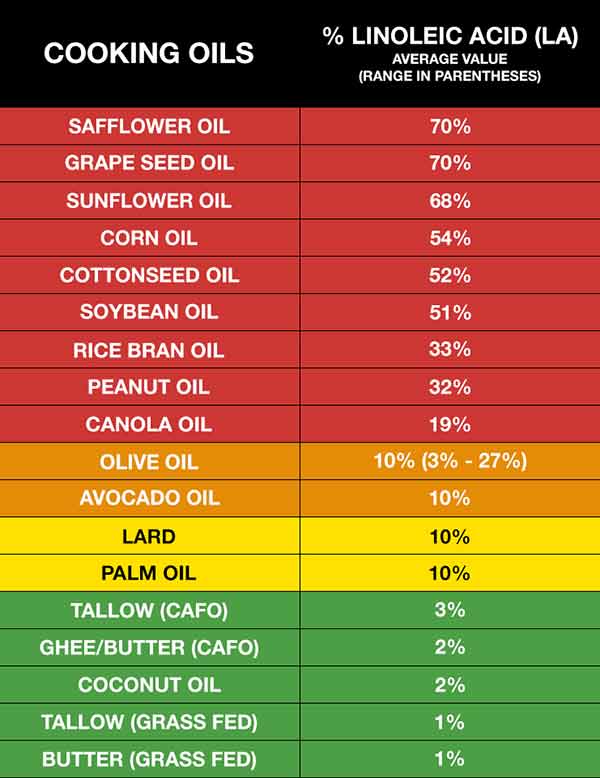
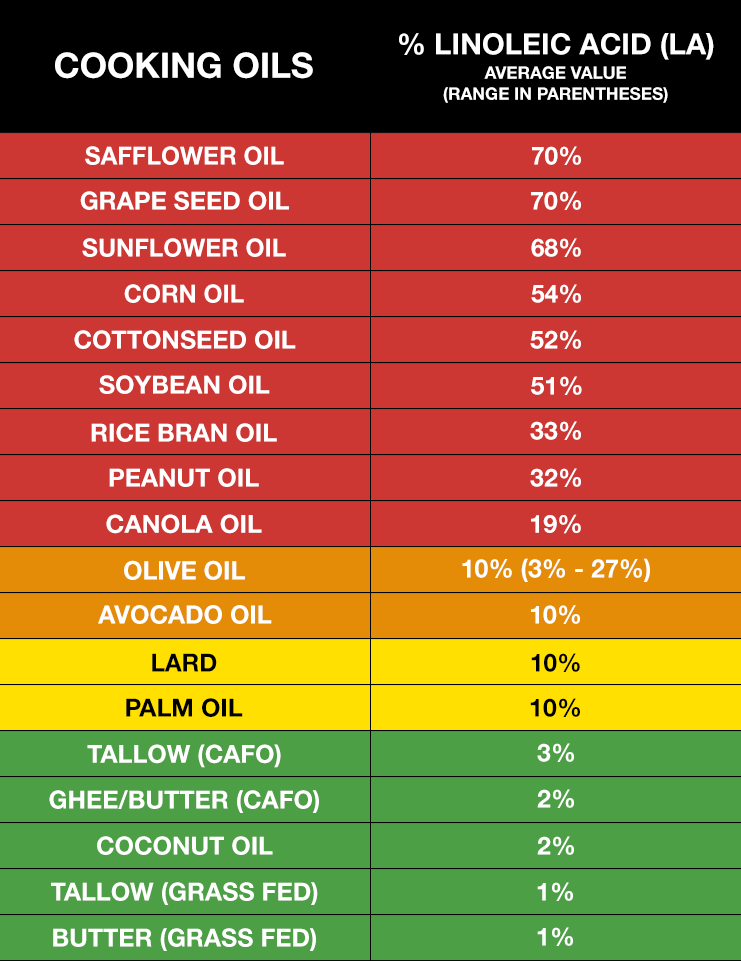
Healthy fat replacements include tallow, butter or ghee, all of which are excellent for cooking. The table below provides a fairly comprehensive list of the most commonly consumed oils and their approximate LA content.
In general, the lowest LA-containing fats — butter and beef tallow — would be the fats of choice. These excellent cooking fats would not only be the lowest in LA, but will also provide the fat-soluble vitamins, A, D, and K2. Coconut oil is also very low in LA but doesn’t provide the important fat-soluble vitamins that tallow and butter contain.
Vitamin E Prevents Oxidation of LA
If you’ve been eating a high-PUFA diet for a long time, consider taking vitamin E regularly until you get your LA down to healthy levels. As noted earlier, CF patients need extra vitamin E anyway, and this is yet another reason to make sure you’re getting enough.
High LA levels increase a potentially dangerous process in your body called lipolysis — the liberation of fatty acids from your fat cells into your bloodstream where they are mobilized. This then increases the oxidation of LA, which is precisely what you want to avoid. Ideally, you want to keep LA in your fat cells until they metabolize it with peroxisomes. Vitamin E can help neutralize this damaging effect of LA.
Due to the high LA burden, few people can get enough vitamin E from their diet to suppress the oxidative destruction caused by LA unless they’re supplementing with vitamin E.
The good news is that since the supplementation is short term, you’re not going to need it the rest of your life. If you can keep your LA intake to below 5 grams a day for three years, it’s likely you may not even need it at all, or at most, only a few times a month.
The Story of Claire Wineland
Claire Wineland, an inspirational speaker and YouTube sensation, was diagnosed with CF at birth. At age 13, she founded the Claire’s Place Foundation17 to help families with children who have CF. She died September 2, 2018, from a massive stroke following an otherwise successful lung transplant.
In 2016, Wineland appeared in an episode of “My Last Days,” a limited CW docuseries hosted by Justin Baldoni, featuring people living with terminal illness. September 2, 2019, YouTube Originals released the documentary “CLAIRE,” directed by Nicholas Reed (above).
While filled with chronic illness, Wineland’s life was a testament to how to live life well, with purpose and gratitude. It’s a potent reminder of how we need to live life to the fullest, even though we might die tomorrow. “I’ve always loved the idea of bringing life into places where people think life doesn’t really exist,” Wineland said.
Wineland’s mother said she was convinced her daughter came into the world with a mission to share the message of “what it’s like to be blessed with life.” I couldn’t agree more.
- 1, 2, 4, 5, 15, 16 Journal of Pharmacy Practice 2012; 26(1): 14-17
- 3, 12, 13, 14 Pharmaceuticals February 2022; 15(2): 217
- 6 Cancer Prevention Research May 2012, DOI: 10.1158/1940-6207.CAPR-12-0045
- 7 Science Daily April 23, 2012
- 8 Sci Transl Med 29 January 2014: Vol. 6, Issue 221, p. 221ra15
- 9 Journal of Health, Population and Nutrition January 17, 2024; 43, Article number 11
- 10 Children 2022; 9(3): 329
- 11 Italian Journal of Pediatrics 2019; 45, Article number 41
- 17 Claire’s Place Foundation, Inc
Migraine Triggers and Helpful Treatments
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/22/migraine-triggers-treatments.aspx
Analysis by Dr. Joseph Mercola April 22, 2024
STORY AT-A-GLANCE
- Migraine is the third most prevalent illness in the world, yet researchers still struggle to understand exactly how and why migraines occur. Adding to the complexity, there are several different types of migraine
- Migraine is thought to be a disorder of your nervous system, most likely originating in your brain stem. Evidence also suggests migraines are strongly related to mitochondrial dysfunction
- One of the primary causes of mitochondrial dysfunction is excess linoleic acid (LA) consumption, so radically reducing your intake should be at the top of your list if you struggle with migraines
- Nutrient deficiencies also appear to play a role. Of particular importance for prevention and treatment of migraine are vitamin D, magnesium, Coenzyme Q10 (CoQ10) and riboflavin (vitamin B2)
Migraines affect an estimated 12% of the American population and is the second leading cause of disability worldwide.1 They can strike both young and old, but a majority of sufferers are women. According to research,2 “Its prevalence increases in puberty but continues to increase until 35 to 39 years of age, decreasing later in life, especially after menopause.”
Worldwide, as many as 1 billion people are affected,3 making migraine the third most prevalent illness in the world. Yet, despite its prevalence, researchers still struggle to understand exactly how and why migraines occur. Adding to the complexity, there are several different types of migraines, including:4,5
| Cluster | Chronic | Episodic |
| Basilar | Hemiplegic | Retinal |
| Abdominal | Optical | With aura |
| Without aura | Status migrainous | Transformed |
| Menstrual | Vestibular |
What Does a Migraine Feel Like?
Migraine attacks are typically recurring, of moderate to severe intensity, many times occurring only on one side of your head. Along with throbbing, piercing or “burning” pain, other common symptoms include nausea, visual disturbances, dizziness, numbness in your extremities or face, and extreme sensitivity to light, sound, smell and touch.6
An attack may last from a couple of hours to as long as three days, often requiring bed rest in complete darkness and silence. In a 2017 Greatist article, migraine sufferers were asked to describe their pain. Here are some of their answers:7
• “My head feels like it’s in a vise” — Triggers often include stress,8 weather changes, physical exertion, lack of sleep and/or eating the wrong foods. Artificial sweeteners9 such as aspartame are also known to commonly trigger migraine.Doctors suggest keeping a food diary to track the emergence of symptoms to pin down certain food triggers. You could do the same for weather and stress if you believe such factors may play a role.
• It’s “like when a light fixture starts to go out” — This patient is describing the effects of ocular migraine, the onset of which often starts with flickering or flashing light phenomena, or zigzagging lines in the peripheral vision, which can eventually take over the entire field of vision.
These visual disturbances are referred to as an “aura.” Other common auras include blind spots, blurry, wavy or kaleidoscope vision. Auras can also involve other senses.
For example, you may experience paresthesia (tingling or numbness), aphasia (trouble speaking), auditory hallucinations or smelling something that isn’t there. Approximately one-quarter of all migraines are accompanied by aura, which is thought to be caused by a chemical or electrical wave in the brain region that processes sensory signals.10
• “It’s like I’ve been staring at the sun” — Oftentimes, the entire head, from the neck up, can feel overworked, “battered and bruised,” or like your brain has been pounded with a hammer. Post-symptoms can also include a stiff neck for up to a day after the headache ends.
• “Like I’m on a ship during a storm” — Nausea and a feeling of being in motion is also common.
Estrogen Is a Major Player in Migraines
Generally speaking, migraine is thought to be a disorder of your central nervous system, most likely originating in your brain stem.11 While most brain regions do not register or transmit pain signals, the trigeminal nerve network does.
Pain is relayed through the trigeminal network to an area in your brain stem called the trigeminal nucleus. From there, it is conveyed to the sensory cortex in your brain that is involved in awareness of pain and other senses. Interestingly, estrogen appears to be a major factor in this chain of events.
The late Ray Peat, a pioneer in bioenergetic medicine, argued that estrogen is a major cause of migraines, and in 2018, research was published that offered fresh support for that view. Researchers found that estrogen sensitizes cells around the trigeminal nerve and connected blood vessels in the head, thereby augmenting pain signals.
Estrogen, of course, is at its highest during women’s’ reproductive years, which also helps explain not only the gender difference in prevalence but also the age range at which migraines are most common. As noted by bioenergetic researcher Georgi Dinkov, a student of Peat, in 2018:12
“After more than 80 years of claiming estrogen protected women from migraines and mood disorders (and prescribing HRT as prevention/treatment) modern medicine seems to be finally recognizing the causative role of estrogen in migraines. Peat has been saying this for years …
The fact that stress also causes and/or exacerbates migraines is another ‘obvious’ sign for the role of estrogen (and serotonin/cortisol) in migraines.
In addition to implicating estrogen as a facilitator and cause of migraines, [a] study13,14 [in Frontiers of Molecular Biosciences] … also states that progesterone and testosterone are protective.
I have personally noticed that all men who complained of migraines have quite obvious signs of hypogonadism and hyperestrogenism — low muscle mass, gyno, irritability, depression, etc.”

Save This Article for Later – Get the PDF Now
Migraines and Mitochondrial Dysfunction
An even more foundational cause of migraines is mitochondrial dysfunction. As such, any strategy that helps improve your mitochondrial function is likely to be helpful. The most important of these strategies is to limit your intake of linoleic acid (LA), as this omega-3 fat acts as a mitochondrial toxin when consumed in excess. I published a paper together with Christopher D’Adamo on the detrimental health effects of LA in July 2023, which you can read for free.15
Ideally, you’d want to keep your intake below 2% of your daily calories, but even 5% would be a significant improvement since most people consume far more than that. Seed oils, and hence most processed foods and restaurant foods, are the primary sources of LA and need to be radically limited. I’ll expound on this further below.
The main reason why excess LA causes so many health problems — from migraines to heart disease and cancer — is that it prevents your mitochondria from working properly. Mitochondria are subcellular organelles responsible for producing most of your cellular energy in the form of ATP, and without ATP, your cells cannot function and repair themselves normally.
PUFAs such as LA are easily damaged by oxygen in a process called oxidation,16 which triggers the creation damaging free radicals.17 These, in turn, give rise to advanced lipoxidation end-products (ALEs)18 and oxidized linoleic acid metabolites (OXLAMs).19,20
LA-Induced Metabolites Cause Major Damage
These ALEs and OXLAMs then go on to cause mitochondrial dysfunction, which is a hallmark of most all chronic disease, including migraines. In addition to oxidation, inflammation and mitochondrial dysfunction, processed seed oils can also:
| Damage the cells lining your blood vessels |
| Cause memory impairment and increase your risk of Alzheimer’s disease (canola oil, in particular, has been linked to Alzheimer’s) |
| Strip your liver of glutathione thereby lowering your antioxidant defenses |
| Inhibit delta-6 desaturase (delta-6), an enzyme involved in the conversion of short-chained omega-3s to longer chained omega-3s in your liver |
| Impair your immune function and increase mortality |
| Make your fat cells more insulin sensitive, thereby causing insulin resistance |
| Inhibit cardiolipin, an important fat in the inner membrane of your mitochondria |
How LA Impairs Your Mitochondria
The inhibition of cardiolipin in the inner membrane of your mitochondria explains much of the damage caused by LA. You have about 40 quadrillion to 100 quadrillion mitochondria throughout the cells of your body. The cristae of the inner membrane of the mitochondria contains a fat called cardiolipin,21 and its function is dependent on the type of fat you get from your diet.
Cardiolipin is important, because it influences the structure of the cristae inside your mitochondria, which is the area where energy production occurs. If cardiolipin is damaged, then the complexes will not be close enough together to form supercomplexes and thus the mitochondrial energy production will be impaired.
Cardiolipin also works like a cellular alarm system that triggers apoptosis (cell death) by signaling caspase-3 when something goes wrong with the cell. If the cardiolipin is damaged from oxidative stress due to having too much LA, it cannot signal caspase-3, and hence apoptosis does not occur.
As a result, dysfunctional cells are allowed to continue to grow, which can turn into a cancerous cell. The type of dietary fat that promotes healthy cardiolipin is omega-3 fat, and the type that destroys it is omega-6, especially LA.
The good news is that dietary changes can improve the composition of fats in your cardiolipin in a matter of weeks, or even days. So, even though it will take years to lower your total body burden of LA, you will likely notice improvements well before then.
What Foods to Avoid, and How
Primary sources of LA include seed oils used in cooking, processed foods and restaurant foods made with seed oils, condiments, seeds and nuts, most olive oils and avocado oils (due to the high prevalence of adulteration with cheaper seed oils), and animal foods raised on grains such as conventional chicken and pork.
Ideally, consider cutting LA down to below 5 grams per day. If you’re not sure how much you’re eating, enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake.
Cronometer will tell you how much omega-6 you’re getting from your food down to the 10th of a gram, and you can assume 90% of that is LA. Anything over 10 grams of LA is likely to cause problems. Healthy fat replacements include tallow, butter or ghee, all of which are excellent for cooking.
The table below provides a relatively comprehensive list of the most commonly consumed oils and their approximate LA content.22,23,24 In general, the lowest LA-containing fats — butter and beef tallow — would be the fats of choice.
These excellent cooking fats would not only be the lowest in LA but will also provide the fat-soluble vitamins, A, D, and K2. Coconut oil is also very low in LA but doesn’t provide the important fat-soluble vitamins that tallow and butter contain.
Some Migraines May Indicate a More Serious Blood Vessel Problem
One long-held theory was that a migraine is caused by vascular changes in your brain, from initial blood vessel constriction and a drop in blood flow, followed by dilation and stretching of blood vessels, which activates pain-signaling neurons.
Newer studies have negated this theory, however, as researchers determined migraines are not actually preceded by constriction and decrease in blood flow, but rather by a blood flow increase of nearly 300 percent. Despite that, circulation appears normal, or even slightly reduced, once the attack is in full swing. The question remains: Why?
One small observational study25 found that migraineurs tend to have a different blood vessel structure in their brains compared to those who do not get migraines. Using magnetic resonance angiography, the researchers examined the structure of blood vessels and the changes in cerebral blood flow, focusing on a system of arteries that deliver blood to the brain called “circle of Willis.”
They found that an incomplete circle of Willis was significantly more common in those who get migraines, with or without aura, compared to the control group (73% and 67% versus 51%, respectively). As a result, compared to those with a complete circle of Willis, those with an incomplete circle had greater asymmetry in hemispheric cerebral blood flow.
According to one of the authors of the study, Dr. John Detre, a professor of neurology and radiology:26
“Abnormalities in both the circle of Willis and blood flow were most prominent in the back of the brain, where the visual cortex is located. This may help explain why the most common migraine auras consist of visual symptoms such as seeing distortions, spots or wavy lines.”
Other research27 suggests some migraines — primarily migraines without aura — may be caused by a tear in your neck artery (arterial dissection), which raises your risk of stroke.
Compared to people who had migraine with aura, those without aura were 1.7 times more likely to have an arterial tear. Arterial dissection and stroke was also more likely in men and those under the age of 39. Overall, your probability of having this problem is very low, but it may be worth getting it checked out if you fall into a high-risk category.
Nutrient Deficiencies Linked to Migraine
Nutritional deficiencies can also contribute to or cause a number of different health problems, including migraines. In the video above, “America’s pharmacist” Suzy Cohen discusses drug-free solutions for migraine and headache relief, including nutritional supplements. Nutrients of particular importance here are vitamin D,28 magnesium, coenzyme Q10 (CoQ10) and riboflavin (vitamin B2), and deficiencies in one or more of these is quite common.
In a migraine study29 involving more than 7,400 children, teens and young adults, 16% to 51% of participants had below average levels of vitamins depending on the vitamin tested.30 Those suffering from chronic migraines were overall more likely to have CoQ10 and riboflavin deficiency compared to those with episodic migraines.
Unfortunately, many of the patients in this study were prescribed preventive therapy and too few were given supplements alone for the researchers to determine if supplementation was enough to actually prevent migraines.31 However, other research suggests they can.
For example, research using vitamin D supplementation demonstrated a reduction in C-reactive protein (CRP) and a statistically significant reduction in headache frequency.32 Another more study by Finnish researchers found that men with the lowest vitamin D levels were twice more likely to suffer frequent headaches than those with the highest levels.
Overall, the lower the men’s blood level of vitamin D, the more frequent their headaches. Those with a vitamin D blood level of 15.3 nanograms per milliliter (ng/mL) or lower typically had one or more headaches per week, while those with a level of 11.6 ng/mL or lower reported up to seven headaches per week. Ideally, your vitamin D level should be in the 60 to 80 ng/mL range, so both groups were severely deficient. As reported by Deming Headlight:33
“The researchers theorized that vitamin D has anti-inflammatory properties that prevent swelling in the sensory neurons and the microglial cells in the brain and is essential for proper brain function. In the study information, they also note that previous studies show vitamin D prevents musculoskeletal pain, a major cause of tension headaches.”
According to research presented at the 50th Annual Meeting of the American Headache Society34 in 2010, nearly 42% of patients with chronic migraine were deficient in vitamin D. The study also showed that the longer you suffered from chronic migraines, the more likely you are to be vitamin D deficient.
Magnesium Is Empirically Recommended for All Migraine Sufferers
Magnesium — which can affect both serotonin receptor function and the production and use of neurotransmitters — has also been shown to play an important role in the prevention and treatment of migraines, and migraine sufferers are more likely to suffer from magnesium deficiency than non-migraineurs.35
Researchers theorize that migraine sufferers may develop magnesium deficiency from a variety of reasons, including poor absorption, renal wasting, increased excretion due to stress or low nutritional intake. Since magnesium administration is both easy and safe, researchers have noted that empiric treatment with a magnesium supplement is justified for all migraine sufferers.36
As a prophylactic, be prepared to boost your magnesium intake for at least three months to experience results, ideally in combination with CoQ10.
In many cases, receiving a high dose of magnesium can also abort an attack in progress. The most effective way to administer magnesium for migraine would be to get an intravenous (IV) infusion. I used to regularly administer magnesium IVs for those with acute migraines and it seemed to work for most patients to abort the headache.
Barring that option, magnesium threonate may be your best option for an oral supplement. It has superior absorbability compared to other forms of magnesium, and since its ability to cross the blood-brain barrier makes it more likely to have a beneficial effect on your brain.
B Vitamins Are Also Important
Besides CoQ10, magnesium and vitamin D, other vitamin deficiencies linked to migraines include riboflavin (B2), B6, B12 and folic acid. One 2009 study37 evaluated the effect of 2 mg of folic acid, 25 mg vitamin B6 and 400 micrograms (mcg) of vitamin B12 in 52 patients diagnosed with migraine with aura.
Compared to the placebo group, those receiving these supplements experienced a 50% reduction in migraine disability over a six-month period. Previous studies38 have also reported that high doses of riboflavin can help prevent migraine attacks. For example, in one study patients who received 400 mg of riboflavin per day experienced a 50% reduction in migraine frequency after three months.
Are You Eating Plenty of These Foods?
Although supplements are convenient, it’s important you get as many nutrients from your diet as possible, as your body can metabolize and absorb vitamins and minerals from your diet more effectively and efficiently than from most supplements.
In addition to adding foods rich in magnesium, riboflavin and CoQ10 to your daily diet, look for organic, grass fed products to reduce your exposure to toxins and additional stressors. As for vitamin D, sensible sun exposure is your best bet. If you opt for a vitamin D3 supplement, be sure to increase your vitamin K2 and magnesium as well.
|
Foods Rich in Magnesium39 |
|
| Dark leafy greens | |
| Wild Alaskan salmon | |
| Yogurt made from organic and/or grass fed milk with no added sugars | |
|
Foods Rich in Riboflavin40 |
|
| Beet greens | Tempeh |
| Crimini Mushrooms | Organic low-PUFA eggs |
| Asparagus | Broccoli |
| Cauliflower | |
Migraines Are a Mitochondrial Problem
The fact that nutritional deficiencies worsen migraine and supplementation can ease it lends additional support to the theory that migraines are a mitochondrial disorder.41 Ubiquinol — the reduced form of CoQ10 — plays a vital role in ATP production, which is the basic fuel for your mitochondria.
Your body does produce ubiquinol naturally; in fact, it is the predominant form in most healthy cells, tissues and organs. However, with rampant pollution and poor diet, mitochondrial dysfunction has become increasingly common, warranting supplementation with either ubiquinol or CoQ10.
One study published in the journal Neurology42 found that CoQ10 was superior to a placebo in preventing migraines and reducing severity. Of the patients who received 100 mg of CoQ10 three times a day, 50% reported significantly reduced frequency of headaches compared to only 14% of those who took the placebo.
That said, while ubiquinol may be beneficial, for long-term migraine relief you really need to address your diet in a more comprehensive manner, as detailed above.
Migraine Prevention 101: Avoid Triggers
Last but not least, it’s also useful to keep a diary of your migraines to identify potentially triggers. That way, you can avoid them. While there are many (and what triggers a migraine for one might not trigger it in another), the following are some of the most common.
| Food and drink, especially wheat and gluten, dairy, cane sugar, yeast, corn, citrus, eggs, artificial preservatives or chemical additives, cured or processed meats, alcohol (especially red wine and beer), aspartame, caffeine and MSG.43,44 |
| Allergies, including food allergies45 and food sensitivities and chemical sensitivities. Research published in the journal Lancet in 197946 showed migraineurs with food antigen immunoreactivity experienced profound relief when put on an elimination diet.
Another randomized, double-blind, cross-over study published in 201047 found that a six-week-long diet restriction produced a statistically significant reduction in migraines in those diagnosed with migraine without aura. If you suspect you might have a food allergy, I suggest doing a diet elimination challenge to see if your symptoms improve. Keep in mind that depending on your typical migraine frequency, you may need to avoid the suspected food for a few weeks in order to evaluate whether it had an effect or not. To confirm the results, reintroduce the food or drink on an empty stomach. If the suspected food is the culprit, you will generally be able to feel the symptoms return within an hour, although migraines can sometimes have a longer lag time than, say, bloating or drowsiness. |
| Hormones — Some women experience migraines before or during their periods, during pregnancy or during menopause. Others may get migraines from hormonal medications like birth control pills or hormone replacement therapy. |
| External stimuli — Bright lights, fluorescent lights, loud noises and strong smells (even pleasant ones) can trigger and/or exacerbate a migraine.
Blue light in particular can be problematic. Many digital devices and LED light sources emit mostly blue light. Research has found that this light increases your migraine pain and activates your trigeminal nerve, associated with the pain of migraines.48 Meanwhile, green light may help ease migraine pain and photosensitivity.49 |
| Changes in sleeping cycle, either missing sleep and oversleeping. |
| Stress/post-stress — Any kind of emotional trauma can trigger a migraine, even after the stress has passed. |
| Dehydration and/or hunger — Skipping meals or fasting are also common triggers. |
| Physical exertion — Extremely intense exercise, or even sex, has been known to bring on migraines. |
| Weather changes, and/or changes in altitude. |
Acupuncture and Chiropractic May Be Helpful Adjuncts to Migraine Treatment
Acupuncture may also be a helpful adjunct therapy. Research has found that getting regular acupuncture treatments can help reduce the frequency and severity of migraine attacks in those suffering from migraine without aura.50,51,52
In all, 249 adult migraineurs who reported two to eight migraine attacks per month were included in the study. They were randomly assigned to receive either 20 real acupuncture treatments or 20 sham treatments over four months. Among those receiving the real treatment, migraine frequency declined by about three episodes per month, while the sham group had two attacks less per month. According to the authors:
“Acupuncture should be considered as one option for migraine prophylaxis in light of our findings.”
It’s interesting to note that even sham treatment had a significant response. Indeed, previous research has shown the placebo effect can be a potent tool in the prevention and treatment of migraines and other types of pain. As noted by neurologist Dr. Amy Gelfand, while the placebo response is troublesome for researchers, it can be a very beneficial effect for patients, especially when the treatment is otherwise safe, be it acupuncture or sugar pills.53
Chiropractic adjustments have also helped many patients, but not all chiropractors are skilled with the techniques to address migraine, so before you schedule an appointment it is important to confirm that your chiropractor has significant experience in helping people treat their migraines.
- 1, 2 Stat Pearls, Migraine Headache
- 3, 6 Migraine Research Foundation, Migraine Facts
- 4 Healthcentral.com, Migraines
- 5 Prevention April 28, 2015
- 7 Greatist March 13, 2017
- 8 Curr Pain Headache Rep. 2016 Jul;20(7):45
- 9 Chris Kresser May 30, 2014
- 10 WebMD, Migraines
- 11 Scientific American July 21, 2013
- 12 Ray Peat Forum August 29, 2018
- 13 Frontiers in Molecular Biosciences August 14, 2018
- 14 EurekAlert! August 14, 2018
- 15 Nutrients July 2023; 15(14): 3129
- 16 Oxid Med Cell Longev. 2014;2014: 360438. DOI: 10.1155/2014/360438
- 17 Pharmacognosy Review. 2010;4(8):118-126
- 18 Biochemical Journal. 1982;208(1):129-140
- 19 Nephrol Dialysis Transplant. 2001;16(8):1598-1606
- 20 Free Radical Biol Med. 1992;13:341-390
- 21 YouTube, Omega-6 Apocalypse 2, Chris Knobbe August 25, 2021
- 22 Renewable Energy. 2018; 126: 403-419
- 23 Int J Mol Sci. 2015;16(6):12871-12890
- 24 The Plan Journal. 2008;54:640-655
- 25 PLoS One July 26, 2016; 8(7): e71007
- 26 Huffington Post July 26, 2013
- 27 WebMD March 6, 2017
- 28 Biomed Research International, 2014; 2014: 827635
- 29 EurekAlert! June 10, 2016
- 30 MD Magazine June 17, 2016
- 31 WebMD June 10, 2016
- 32 Journal of Research in Medical Sciences 2015 May; 20(5): 477–482
- 33 Deming Headlight February 4, 2017 (Archived)
- 34 50th Annual Meeting of the American Headache Society (Archived)
- 35, 36 J Neural Transm (Vienna). 2012 May;119(5):575-9
- 37 Pharmacogenetics and Genomics 2009 Jun;19(6):422-8
- 38 European Journal of Neurology 2004 Jul;11(7):475-7
- 39 EverydayHealth.com, 9 Food Sources of Magnesium
- 40 Whfoods.com, Vitamin B2 Rich Foods (Archived)
- 41 Headache 2012 Oct;52 Suppl 2:81
- 42 Neurology 2005 Feb 22;64(4):713-5
- 43, 46 Lancet 1979 May 5;1(8123):966-9
- 44 Sun Sentinel June 18, 2013 (Archived)
- 45 PubMed.gov, “Food allergies and migraine” search results
- 47 Cephalalgia 2010 Jul;30(7):829-37
- 48 Nature Neuroscience 2010 Feb; 13(2): 239-245
- 49 Science Daily May 17, 2016
- 50 JAMA February 20, 2017 DOI: 10.1001/jamainternmed.2016.9378
- 51, 53 Reuters February 23, 2017
- 52 CNN February 21, 2017
Why Choline Is NOT Associated With Prostate Cancer
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/12/choline-prostate-cancer.aspx
Analysis by Dr. Joseph Mercola April 12, 2024

STORY AT-A-GLANCE
- Choline, essential for numerous physiological processes such as brain development, DNA synthesis and fat metabolism, was officially recognized as a vital nutrient in 1998, with deficiencies linked to severe health issues
- High choline intake is associated with significant health benefits, including reduced risks of heart disease, breast cancer and nonalcoholic fatty liver disease, underscoring its importance in your diet
- Studies suggesting a link between choline intake and an increased risk of prostate cancer fail to account for various dietary and environmental factors, leading to misleading conclusions about eggs
- Choline deficiency poses a greater health risk than high intake. An estimated 90% of Americans already do not meet the adequate daily intake values set by the Institute of Medicine
- Eggs from chickens fed a low-linoleic acid diet are a powerhouse of nutrition. They provide high-quality protein, essential fats, vitamins like D, E and K, and minerals such as selenium and zinc. Eggs also contain B vitamins essential for energy production
Some studies,1 including analyses from NHANES data, have stirred up fears about choline and its alleged link to an increased risk of prostate cancer. This fear causes people to avoid one of the most important nutrients to their health.
As your guide to deciphering the complexities of health and nutrition, I feel it’s imperative to address these concerns and explain why the fear surrounding choline intake, particularly from eggs, is not only misplaced but may also deter you from enjoying one of nature’s most nutrient-dense foods.
First, let’s understand what choline is. Choline, initially discovered in 1862,2 was officially recognized as an essential nutrient for human health by the Institute of Medicine in 1998.3 It plays a critical role in many physiological processes, including:4
| Healthy fetal development5 — Choline is required for proper neural tube closure,6 brain development and healthy vision.7 Research shows mothers who get sufficient choline impart lifelong memory enhancement to their child due to changes in the development of the hippocampus (memory center) of the child’s brain.8 Choline deficiency also raises your risk of premature birth, low birth weight and preeclampsia. |
| The synthesis of phospholipids, the most common of which is phosphatidylcholine, better known as lecithin, which constitutes between 40% and 50% of your cellular membranes and 70% to 95% of the phospholipids in lipoproteins and bile.9 |
| Nervous system health — Choline is necessary for making acetylcholine, a neurotransmitter involved in healthy muscle, heart and memory performance.10 |
| Cell messaging, by producing cell-messaging compounds.11 |
| Fat transport and metabolism — Choline is needed to carry cholesterol from your liver, and a choline deficiency could result in excess fat and cholesterol buildup.12 |
| DNA synthesis, aiding in the process along with other vitamins, such as folate and B12. |
| Methylation reactions.13 |
| Healthy mitochondrial function.14 |
Health Benefits of Choline
Studies have linked higher choline intake to a range of benefits, including a decreased risk for heart disease,15 a 24% decreased risk for breast cancer,16 and the prevention of nonalcoholic fatty liver disease (NAFLD).
In fact, choline appears to be a key controlling factor in preventing the development of fatty liver by enhancing secretion of very low-density lipoprotein (VLDL) particles, which are required to safely transport fat out of your liver.17 Research has also discovered evidence of epigenetic mechanisms of choline,18 which also helps explain how choline helps maintain healthy liver function.
Research19 published in 2020 also concluded that choline has anti-inflammatory activity and can be particularly useful in those with insulin resistance and/or metabolic syndrome. And, while a choline supplement was good in this regard, eggs were far better. Choline has also been shown to prevent neurodegenerative diseases such as Alzheimer’s by:20,21
- Reducing your homocysteine level, an amino acid that has been shown to cause neurodegeneration and is involved in the formation of amyloid plaques, two hallmarks of Alzheimer’s. Choline converts homocysteine into methionine, which has several beneficial effects.
- Inhibiting microglia activation — Microglia cells clear debris from your brain, and while this is a crucial function, in Alzheimer’s the microglia tend to become overactivated, causing inflammation in the brain that can result in the death of neurons. By reducing activation of microglia, choline can help protect Alzheimer’s patients from further brain damage.
Study Linking Choline to Prostate Cancer Has Many Weaknesses
The primary study22 that has many people second-guessing their egg consumption analyzed meat, milk and egg intake and their potential associations with prostate cancer. All of these are sources of choline, although eggs contain the highest amounts.
It suggested there might be a link between high dietary choline intake and an increased risk of advanced, lethal prostate cancer. According to the authors, “Men in the highest quintile of choline intake had a 70% increased risk of lethal prostate cancer.” However, this conclusion overlooks several crucial aspects.
For starters, the study was observational, meaning it can indicate associations but cannot prove causation. Considering the many dietary and environmental factors that can influence health outcomes, it’s extremely difficult to isolate the effect of a single nutrient.
What’s more, they only collected dietary information six times during 22 years of follow-up, which raises questions about accuracy. Many can’t even recall what they ate a few days ago, let alone the type of food and weekly quantity they consumed over the past year. Other shortcomings of this study include the following:
- It does not account for other components of the diet that could influence prostate cancer risk, such as phytonutrients, fiber, and other vitamins and minerals.
- No dose-response relationship across quintiles of choline intake was established. Understanding whether the risk of prostate cancer increases linearly with choline intake or if there’s a threshold effect would be crucial for dietary recommendations.
- The study also looked at postdiagnostic intake of choline and its relationship with lethal prostate cancer among men who were initially diagnosed with nonmetastatic disease and here, no statistically significant link could be found.

Save This Article for Later – Get the PDF Now
The Source of Choline Matters
The source of the choline also matters. Not all choline sources are created equal. Eggs, especially those from chickens fed low-linoleic acid (LA) diets, are incredibly nutrient-dense, offering not just choline but also vitamins, minerals and antioxidants in a natural package that your body can efficiently use.
Conversely, conventionally-raised eggs tend to be high in LA, and as I detailed in my extensive report on LA, this dietary component is a major driver of all chronic disease, including cancer, as it impairs your mitochondrial function and inhibits energy production.
An estimated 90% of the U.S. population is deficient in choline.23 At the same time, most people consume several times more LA than is safe based on historical intakes. So, what’s more likely to contribute to cancer? LA or choline?
There’s also the issue of generalizing. The study population, comprised of 47,896 male health professionals from the United States, may not represent the broader public due to its homogeneity in terms of profession, education, and potentially, socioeconomic status.
These factors can influence dietary habits, health awareness, access to healthcare, and the ability to engage in preventative health behaviors, which in turn could affect the study’s findings and their applicability to the general population.
For example, while health professionals are commonly expected to have greater knowledge about nutrition and disease prevention, this is rarely the case. Rather, they tend to follow standard dietary recommendations issued by government, which have repeatedly been proven to be disastrous for health.
Case in point, for decades, the recommendation has been to avoid saturated fat and cholesterol (both of which are high in eggs) and to opt for polyunsaturated (PUFA) seed oils instead, which, as it turns out, is a perfect recipe for cancer. So, was high choline consumption really the issue, or did they also have higher LA intake because of following misguided dietary recommendations?
Low-PUFA Eggs Are a Powerhouse of Nutrition
Focusing on a single nutrient also fails to consider the synergistic effects of foods. Whole foods like eggs contain a complex mix of nutrients that work together to support health.
Indeed, egg yolks from chickens fed low-LA diets are a powerhouse of nutrition. They provide high-quality protein, essential fats, vitamins E and K, and minerals such as selenium and zinc. Moreover, eggs are one of the few dietary sources of vitamin D, which is crucial for bone health and immune function.
A single hard-boiled egg can contain anywhere from 113 milligrams24 (mg) to 147 mg25 of choline, or about 25% of your daily requirement, making it one of the best choline sources in the American diet.26 Only grass fed beef liver beats it, with 430 mg of choline per 100-gram serving.27
Egg yolk also contains a large amount of B vitamins, all of which are necessary cofactors in the steps to produce energy in your body.
If you’re micronutrient deficient, your metabolism will be low because you don’t have the necessary cofactors to generate ATP, and in carbohydrate metabolism, choline is one of those necessary cofactors. When you add the high rate of choline deficiency in the general population into the mix, it’s highly unlikely that choline would be the cause behind lethal cancer.
How Much Choline Do You Need?
While a dietary reference intake value has not yet been established for choline, the Institute of Medicine set an “adequate daily intake” value of 425 mg per day for women, 550 mg for men and 250 mg for children28,29 to help prevent a deficiency and potential organ and muscle damage.
Curiously, those in the highest quintile of choline intake in this study30 were only getting a median of 509 mg per day, which doesn’t even meet the IOM’s ADI.
Keep in mind, however, that requirements can vary widely, depending on your overall diet, age, ethnicity31 and genetic makeup. As noted in one paper,32 “People with one of several very common genetic polymorphisms in the genes of choline metabolism are more likely to develop hepatic dysfunction when deprived of choline.”
Another study33 found that in some men, 550 mg of choline per day was insufficient as they still developed organ dysfunction. Postmenopausal women were also more prone to develop signs of organ dysfunction than premenopausal women when deprived of adequate amounts of choline for just under six weeks.
Eating a diet high in (otherwise healthy) saturated fats may also increase your choline requirement by as much as 30%.34 Pregnant and breastfeeding women, athletes and postmenopausal women also need higher amounts.
The tolerable upper intake level for choline is 3.5 grams per day. Side effects of excessive choline include low blood pressure, sweating, diarrhea and a fishy body odor.35 Unfortunately, none of these signs and symptoms of choline excess were investigated in the featured study.
The Bigger Picture
It’s essential to look beyond headlines and understand the broader context of nutrition science. The fearmongering around eggs and choline is a perfect example of how isolating nutrients from their dietary context can lead to misleading conclusions.
A balanced diet focusing on whole, unprocessed foods is key to optimal health, and sadly, many simply don’t get enough essential nutrients because their diets are so loaded with processed food.
Food testing by Moms Across America (MAA) highlights the seriousness of the situation, as they found school lunches contain more toxins than nutrients.36 All school lunches tested contained heavy metals — some at levels up to 6,293 times higher than the maximum levels allowed in drinking water — and 95% had detectable levels of glyphosate.
Meanwhile, most of the meals were “abysmally low” in essential nutrients. Similarly, fast food meals provide nowhere near your daily nutrient requirements for vitamins and minerals.37
So, in conclusion, don’t let fearmongering dictate your dietary choices. Eggs, particularly from chickens on a healthy diet, remain one of the most nutrient-rich foods you can eat. As always, it’s about the quality and the source. Incorporating eggs into a balanced, nutrient-dense diet supports health far more than it harms.
Assuming you’re not getting choline from other sources, you need to eat at least two, probably three and more, egg yolks per day. I eat six yolks a day (but only one egg white) because I work out and walk at least five to six miles a day. The more active you are, the more choline you need to support a higher metabolic rate.
- 1, 22 American Journal of Clinical Nutrition 2012 Oct; 96(4): 855–863
- 2 Ann Nutr Metab. 2012;61(3):254-258
- 3 Nutr Rev. 2009 Nov; 67(11): 615–623
- 4 Natural Products Insider, The Choline Need (PDF)
- 5 Nutr Today. 2007; 42(4): 181–186
- 6 Am J Epidemiol. 2004 July 15;160(2):102-9
- 7 Am J Epidemiol. 2013 June 15;177(12):1338-47
- 8 J Am Coll Nutr 2004 Dec.;23(6Suppl):621S-626S
- 9, 10, 13, 14, 18, 32 Curr Opin Clin Nutr Metab Care. 2013 May; 16(3): 339–345
- 11 J Inherit Metab Dis. 2011 Feb.:34(1):3-15
- 12 J Biol Chem. 2002 Nov. 1;277(44):42358-65
- 15 ARYA Atheroscler. 2011 Summer;7(2):78-86
- 16 FASEB J. 2008 June;22(6):2045-2052
- 17 Veterinary Journal 2008 Apr;176(1):10-20
- 19 Nutrients 2020; 12(10): 3120
- 20 Molecular Psychiatry January 8, 2019
- 21 Science Daily January 8, 2019
- 23 Clean Eating Magazine November 23, 2021
- 24 Nutrition Data, Hardboiled egg (Archived)
- 25 USDA Nutrient Database Hardboiled egg
- 26 Nutr Rev. 2009 Nov; 67(11):615-623
- 27 USDA Database for Choline January 2008
- 28 Fatty Liver Diet Guide 2012-2015 (Archived)
- 29 NIH Choline Fact Sheet
- 30 American Journal of Clinical Nutrition 2012 Oct; 96(4): 855–863, Table 1
- 31 FASEB J. 2014 July;28(7):2970-8
- 33 American Journal of Clinical Nutrition 2007 May;85(5):1275-85
- 34 Chrismasterjohnphd.com November 23, 2010
- 35 Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline
- 36 Moms Across America September 28, 2022
- 37 Moms Across America October 18, 2023
Five ‘Simple yet Effective’ Tips to Boost Your Longevity
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/10/tips-to-boost-your-longevity.aspx
Analysis by Dr. Joseph Mercola April 10, 2024

STORY AT-A-GLANCE
- Simple changes can significantly influence overall health and longevity. Nearly 70% of people across five generations said they would like to live 100 years, but not if they had terrible health, were a burden on their family, or if they had serious cognitive loss
- Training specialist David Wiener found five effective choices to help achieve that goal, beginning with keeping your brain active using games, concentration skills, keeping a gratitude journal, going for daily walks and reaching out to loved ones
- Fresh air and sunshine can help lift your mood and optimize your vitamin D levels, which decreases your risk of metabolic syndrome, Type 2 diabetes and heart disease. Sleep reduces your risk of heart disease and stroke
- Chronic stress can lead to medical conditions that shorten your lifespan. Exercise is generally acknowledged as leading to a healthier life, but exercising in the late morning hours can support greater benefits than exercising at other times of the day
- Each of these five simple strategies can make a significant difference in your overall health and longevity. Perhaps the most important factor, however, is reducing your linoleic acid (LA) intake, as LA is a potent metabolic poison when consumed in excess
Longevity and the Fountain of Youth have been a focus of human thought and experiment for centuries. Researchers are fascinated by the topic. A quick search on PubMed reveals over 62,000 results for research studies that include the term “longevity”1 and over 150 studies listed on ClinicalTrials.gov.2
The financial company Edward Jones3 published a 2022 study in which they asked five generations of Americans whether they wanted to live to age 100. Nearly 70% of them said “yes,” but included that they would not want the added longevity if they had terrible health, were a burden on their family or had serious cognitive loss. The researchers wrote, “The real answer to our question seems to be, ‘Yes, but it depends on staying healthy, engaged and purposeful.'”4
The Edward Jones report noted that the number of people who are 65 and older has nearly tripled in the last 50 years and it is projected to reach 86 million by 2050. They note that together with living longer and more people retiring, this stage in life appears to be far more important than in previous decades, and with far more social and marketplace implications.
A reporter from the online magazine Express5 spoke with David Wiener, training specialist at AI-based fitness and lifestyle coaching app Freeletics. He shared tweaks you could include in your lifestyle choices that would be simple, but effective in helping you to meet this goal — living a longer, healthier and more engaged life.
One thing he did not address, however, was diet. As detailed in “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” linoleic acid, an omega-6 fat, acts as a metabolic poison when consumed in excess.
So, if you want to live a long, healthy life, this really ought to be your starting point. LA intake above 10% is highly likely to cause problems. Ideally, you want to keep it well below 5%. If your LA intake has been high, make sure you’re getting enough vitamin E, as it protects polyunsaturated fats like LA from lipid peroxidation. That said, let’s take a look at Wiener’s suggestions, all of which are good.
Keep Your Brain Active and Sharp
Wiener describes keeping your brain active as being one of the “best ways”6 of increasing life expectancy and maintaining your cognitive ability. “By challenging your brain with mental exercises, it is believed you could maintain individual brain cells and stimulate communication between them to help them work more effectively,” Wiener told Express. He went on,7
“While most people’s jobs keep them mentally active and alert, learning a new hobby or skill, volunteering or mentoring are additional ways to keep your mind sharp, more specifically learning a language has shown to be greatly beneficial too.”
Your brain is one of the most important organs in your body. Exercising your brain, in the same way that you would exercise your body, plays a significant role in longevity and independence. Taking care of your brain includes engaging in stimulating activities that not only make your brain work but also bring you joy.
Some of the activities that Dr. Laurie Archbald-Pannone, a geriatric medicine physician and associate professor of medicine at the University of Virginia, recommends include keeping a gratitude journal, going for a daily walk and reaching out to friends and family.
Denise Park, Ph.D., professor and director of research at the Center for Vital Longevity in the School of Behavioral Sciences at the University of Texas in Dallas, spoke with Forbes Magazine8 about a study in which she and her team engaged a group of older individuals to learn two new activities — digital photography and quilting.
The researchers found the adults improved their memories over three months. Park talked about finding the optimal amount of challenge to maintain a healthy mind, noting that too much is stressful but too little does not encourage gain. “Adding novel behaviors that you never performed before helps build new neural circuits that will be built to handle that challenge,” she said.9
Finding games that stimulate different functions can also support your social life. Engaging in stimulating brain activity with others helps to reduce isolation and the brain exercise helps give you a sense of control as well as helps support the creation of new brain connections.
Dr. Zaldy Tan is an expert in senior care and the director of the Cedars-Sinai Memory and Aging Program. Tan identified types of brain activities that help challenge and exercise your mind. Tan suggests games that challenge:10
- Verbal memory such as a crossword puzzle
- Concentration skills such as online brain games
- Visual-spatial working memory skills such as a jigsaw puzzle
- Tactile skills that use procedural memory such as knitting or model building
- Tactile, visual, motor and auditory skills such as dancing
Get Outside to Enjoy the Fresh Air and Sunshine
It’s no secret that being outside in the fresh air is healthy. Wiener recommends gardening and taking walks to help boost your time outside and optimize your vitamin D levels.11 One meta-analysis of 28 studies demonstrated a substantial decrease in heart disease, metabolic syndrome and Type 2 diabetes in middle age to elderly people with high levels of vitamin D.12
Optimal levels of vitamin D also support healthy function of your muscles and immune system, as well as bone health by helping your body to absorb calcium.13 However, depending on where you live and the time of the year, it’s not always possible to get outside for a little sunshine.
It is important to note that vitamin D supplements may help to raise your vitamin D serum measurements, but they don’t give you everything you need. As Wiener points out, sunshine also influences your sleep, which I discuss just below. “This is because sunlight also regulates another hormone in the body called melatonin that controls your sleep cycle,” Wiener said.

Save This Article for Later – Get the PDF Now
Red and Near-Infrared Light Therapy
If sunshine is not an option, then red and near-infrared light, which are subsets of natural sunlight, may help you get some of the same benefits. During an interview with Ari Whitten, author of “The Ultimate Guide to Red Light Therapy,” we reviewed the mechanics and benefits of red light and infrared light. Whitten has a degree in kinesiology, exercise science and movement science, and has studied natural health and nutrition for over 20 years.
Over the last few decades, there have been more than 5,000 studies published about red and near-infrared light therapy, also called photobiomodulation. Researchers have noted an impact on a wide range of conditions, including combating wrinkles and cellulite, improving hair regrowth and sports performance, increasing strength and benefits for individuals with Alzheimer’s and Parkinson’s disease.
Red and near-infrared light operates through several mechanisms of action in the body to produce positive effects. As Whitten and I discussed in the interview, it helps support mitochondrial health and stimulate mitochondrial biogenesis, modulates gene expression and helps structure water that surrounds your cells. Each of these mechanisms offers significant benefits to your overall health.
Sleep: Prioritize Quality and Quantity
Wiener notes that research has consistently demonstrated sleeping less than six hours each night presents a significant risk for heart attack and stroke. Taking care to get at least seven to eight hours of quality sleep each night can help support longevity.
Nearly every facet of your biology is affected when you don’t get enough sleep, which is demonstrated by the long list of health effects linked to sleep deprivation. You’ll find a list and studies in the article linked below. Some of the effects include reduced athletic performance, increased risk of neurological issues, increased risk of Type 2 diabetes, weakened immune function and an increased risk of high blood pressure, heart attacks and cardiovascular disease.
Unfortunately, many people still see a lack of sleep as a badge of honor. To them, it signifies a sign of drive, ambition and achievement. Worse, good sleep may be characterized as a sign of sloth. In 2018, Joe Rogan interviewed professor Matthew Walker, Ph.D., founder and director of the University of California Berkeley’s Center for Human Sleep Science.
As explained by Walker,14 your brain doesn’t shut down while you’re asleep. Instead, some parts become far more active than when you’re awake. During REM sleep, the visual, motor kinesthetic, emotional and memory centers increase activity, while the area that rules rationality and logical thinking, decreases. There are several common factors that Walker calls the “enemy of sleep.” These include:
- Alcohol and caffeine — These and other substances, such as sleeping pills, interfere with sleep quality and sleep time
- Artificial lighting — We have effectively electrified the night, and light at night damages your health by degrading your sleep
- Loneliness, anxiety and depression — The longing for connection and the effects of mental illness can often interfere with or cause people to forego sleep
- Long work hours — The international business environment, increased global competition and longer commuter times are just a few of the factors contributing to the increase in work hours and stress-related burnout
- Overcommitment — Schedules are filled from morning to night, and many people are unwilling to trade entertainment or socializing with family and friends for sleep
Wiener and Walker make several recommendations to achieve quality sleep each night. You’ll find those and more in “Sleep — Why You Need It and 50 Ways to Improve It.”
Use Stress Reducing Strategies to Lower Cortisol Secretion
As Wiener stated, stress can trigger the release of high cortisol levels.15 A fight or flight response can raise your blood pressure and give you the resources you need in the moment. But chronic activation of the system causes the consistent release of hormones that produce harmful physiological changes.16 This leads to the storage of abdominal fat, insomnia, low energy and changes in appetite.
Additionally, it can lead to high blood pressure, heart disease, metabolic syndrome, arthritis, Type 2 diabetes and obesity. Each of these chronic diseases can lead to premature death. The fight or flight response is modulated by the sympathetic and parasympathetic nervous systems, which are part of the autonomic nervous system. This system controls functions in the body that happen automatically, such as heart rate and blood pressure.
The sympathetic nervous system signals the fight or flight response to begin, and once the danger has passed the parasympathetic nervous system helps apply the brakes to the hormone release. In chronic stress, your sympathetic nervous system is revved up, which has a detrimental effect on your health. But, by using controlled breathing techniques, you can create physiological change that lowers your heart rate and blood pressure and improves immune function.
Breathing techniques can help modulate the autonomic nervous system, several of which you can read about in “Have You Tried Box Breathing?” Box breathing is a basic tactical breathing technique used by Navy SEALS to remain calm under duress.17
Other Ways to Normalize Cortisol
Two other factors that will have a significant impact on your cortisol level is low-carb diets and fasting. Both are sure-fire ways to increase cortisol and should be avoided if you’re trying to optimize your mitochondrial function.
If you don’t get enough glucose from your diet, your body must produce glucose by activating stress hormones like glucagon, adrenaline, and cortisol, which make glucose by sacrificing the protein stored in your muscle, bones and brain.
To avoid this, you’ll want to make sure you’re getting at least 150 grams of glucose a day, ideally from ripe fruit. My carb intake is currently between 400 to 450 grams a day, and I feel great.
If you have a healthy gut, you’ll be able to incorporate more fruit fiber without a problem. If your gut is impaired, however, the extra fiber can feed endotoxin-producing bacteria in your gut, which will suppress your mitochondrial function even further. In this case, start by introducing things like pulp-free orange juice.
You Get Greater Benefits When You Exercise in the Morning
Exercise is generally acknowledged as leading to a healthier life, but did you know that there are certain times of the day when you experience greater benefits? Wiener18 recommends exercising in the morning to take advantage of fat oxidation that naturally occurs during the morning hours before having your first meal.
A 2022 paper19 found an association between the time of day you exercise and the risk of coronary heart disease and stroke. The 86,657 men and women who participated were free of cardiovascular disease at the beginning of the study.
The researchers compared the peak time of activity across a 24-hour period and found those who were most active during the late morning had a significantly lower risk of stroke and coronary artery disease compared to people who had a pattern of midday activity.
You can use each of these five simple strategies to make a significant difference in your overall health and longevity. While they may seem simple and easy — almost too easy — they are highly effective and help you take control of your health.
- 1 PubMed, “Longevity”
- 2 Clinical Trials, “Longevity”
- 3, 4 Edward Jones, Longevity and the New Journey of Retirement page 4 & 5
- 5 Express, March 3, 2024
- 6, 7 Express, March 3, 2024, #1
- 8, 9, 10 Forbes Health, May 23, 2023
- 11 Express, March 3, 2024, #2
- 12 Maturitas 2010; 65(3)
- 13 NIAMS, Calcium and Vitamin D: Important for Bone Health, What Does Vitamin D Do for Our Bones? 60% down the page (DTP)
- 14 YouTube, Joe Rogan Experience #1109, Min 13:11
- 15, 18 Express, March 3, 2024, #4
- 16 Yale Medicine, Chronic Stress Subhead 3, 4
- 17 YouTube, Box Breathing and Meditation Technique w/ Mark Divine of SealFit – TechniqueWOD
- 19 European Journal of Preventive Cardiology, 2022; 30(3)
Alzheimer’s Is Now a Leading Cause of Death
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/06/alzheimers-death-rate.aspx
Analysis by Dr. Joseph Mercola April 06, 2024
Story at-a-glance
- Alzheimer’s disease, a severe form of dementia, affected an estimated 6.7 million Americans in 2023, and deaths from Alzheimer’s more than doubled between 2000 and 2019
- Previous U.S. data placed the number dying from Alzheimer’s disease around 83,000 in 2010. By 2014, research suggested the true number was well over half a million per year — more than six times higher than previously thought. Today, 1 in 3 seniors dies with Alzheimer’s or some other dementia, and the death toll exceeds that of breast- and prostate cancer combined
- Since there’s no conventional cure, prevention is crucial if you want to avoid becoming a statistic. Two key strategies are lowering your linoleic acid (LA) intake and avoiding estrogen and estrogenic compounds
- Advances in diagnosis are being made. For example, researchers have created a blood test that predicts Alzheimer’s with great accuracy. There’s also a peanut butter smell test, and a free 15-minute at-home test called Self-Administered Gerocognitive Examination (SAGE) that can facilitate early diagnosis
Alzheimer’s disease, a severe form of dementia, affected an estimated 6.7 million Americans in 2023.1 It is not pretty to lose your mind, as many of you know from firsthand experience with relatives or friends. This devastating degenerative brain disease develops slowly over time and tends to be lethal in its final stages.
As a general guideline, tell-tale symptoms of Alzheimer’s include a decline in memory along with a decline in at least one of the following cognitive abilities:
- Speaking coherently or understanding spoken or written language
- Recognizing or identifying objects
- Ability to perform motor activities
- Abstract thinking and ability to make sound judgments
- Planning and carrying out complex tasks
Alzheimer’s Deaths Outpace Breast- and Prostate Cancer
Deaths from Alzheimer’s more than doubled between 2000 and 2019.2 In 2014, research suggested the actual death toll may be well over half a million per year,3 which would put Alzheimer’s in the top three killer diseases in the U.S., right behind heart disease and cancer.
Officially, it’s the sixth-leading cause of death in the United States as of 2019,4 and with a total of 121,499 recorded deaths that year, Alzheimer’s claimed more lives than breast- and prostate cancer combined.5
However, it seems the 2014 study was onto something, because while Alzheimer’s was listed on 121,499 death certificates in 2019, underlying causes like AD are typically left off. As explained by Bryan James, an epidemiologist at the Rush Alzheimer’s Disease Center in Chicago and lead author of the 2014 study:6
“Death certificates are well known to underreport deaths from Alzheimer’s and other types of dementia. The more immediate causes of death, such as pneumonia or heart attack, are usually listed, and the underlying causes of death are usually left off.”
Alzheimer Death Toll May Be Six Times Higher Than Previously Thought
The 2014 study, published in the journal Neurology,7 followed 2,566 seniors aged 65 and over for eight years. In that time, close to one-quarter of them developed Alzheimer’s. Four hundred of them died from the disease.
Using statistic extrapolation, the researchers came up with an estimated annual Alzheimer’s death toll in excess of 503,000 — more than six times higher than previous estimates. According to Dallas Anderson,8 an overseer of population studies relating to Alzheimer’s and dementia at the National Institute on Aging (NIA):
“People who I think are knowledgeable about the death registration system in the U.S. would not be surprised that the official number is low, but it is somewhat of a surprise to see that kind of a difference … It’s just another reminder that Alzheimer’s is really an important public health problem, and we need to work on it.”
Indeed, and since there’s no conventional cure, the issue of prevention is crucial if you want to avoid becoming a statistic here. There are also few if any successful medical treatments available once Alzheimer’s sets in.
For example, memantine (sold under the brand name Namenda) is approved for moderate to severe cases of Alzheimer’s, but doctors also prescribe it off-label for mild cases. Unfortunately, the drug has been found to be useless for mild to moderate Alzheimer’s.
A 2011 analysis of data9 from three clinical trials showed that patients with mild Alzheimer’s who took Namenda had no improvement in mental function or their ability to perform everyday tasks when compared to placebo. Even among moderate to severe Alzheimer’s patients, for which the drug is approved to treat, the researchers found only “meager” improvements.
Other go-to drugs for the treatment of Alzheimer’s include cholinesterase inhibitor drugs such as Aricept, Exelon and Reminyl. These too may do more harm than good as they provoke slower heart rates, significantly increasing your chances of getting a permanent pacemaker. They also raise your risk of hip fracture.
So, what can you do? The good news is that two key prevention strategies (which virtually no one is talking about) are relatively easy to implement, namely minimizing your linoleic acid (LA) consumption and estrogen exposure.

Save This Article for Later – Get the PDF Now
High Serotonin Levels Linked to Dementia
In September 2023, research10,11 linked high serotonin to dementia. Disturbingly, media outlets completely misrepresented the findings by confusing serotonin with serotonin transporter (SERT). What the researchers found was that having low levels of SERT is linked to problems with memory and thinking skills, which can eventually lead to dementia or Alzheimer’s disease.
Media, however, reported that “low serotonin” was linked to dementia, which is the converse of what they actually found. SERT is like a “clean-up crew” in the brain. It helps remove excess serotonin, which is a chemical messenger in the brain. When there’s not enough SERT around to do its job, serotonin levels outside of brain cells can rise too high. This excess serotonin floating around can cause trouble and contribute to problems with memory and thinking.
So, when the study talks about “low SERT” being associated with cognitive problems, it really means that having less of this clean-up crew leads to higher levels of serotonin outside brain cells. And higher levels of serotonin outside brain cells are linked to dementia. As noted by bioenergetic researcher Georgi Dinkov:12
“STUDY: high serotonin linked to dementia; MEDIA: low serotonin linked to dementia.13,14 Once again, a level of misreporting that I am much more included to ascribe to malice than incompetence simply because most of the popular press outlets covering a specific scientific study get the study authors to proof-read the press article before publishing.
So, for patently false press articles like that to appear is most likely due to an attempt to preserve the status of serotonin as the ‘happy hormone,’ as well as to delay/prevent the avalanche of lawsuit for iatrogenic dementia from all people taking SSRI and other serotonergic drugs.
In summary, the actual study found that low levels of the serotonin transporter (SERT) — the sodium-dependent protein responsible for uptake and deactivation of serotonin — were associated with cognitive impairment (which usually develops into full-blown dementia/Alzheimer with age).
In other words, higher extracellular serotonin levels were associated with dementia. The press articles state the exact opposite — that lower levels of the ‘happiness’ hormone serotonin were associated with dementia …
[The] study also suggests the prevention of dementia/Alzheimer may be as simple as eating some extra salt (providing the required sodium co-factor of SERT), or using a serotonin antagonist.
Air ionizers, which also tend to decrease extracellular serotonin may be helpful too and can provide benefit 24×7 without any conscious effort on behalf of the person/people using them.”
How to Address Elevated Serotonin
Considering that high extracellular serotonin can contribute to dementia, you’d be wise to keep your serotonin level as low as possible. One way to do that is by increasing GABA, which is available as a supplement. GABA increases the degradation rate of serotonin, so you cannot have high levels of both.
People with high GABA/low serotonin are typically calm and gregarious, whereas GABA deficiency and elevated serotonin is associated with anxiety, fear, depression, short temper, phobias, impulsiveness and disorganization.
People who have high GABA levels usually have low serotonin, and vice-versa. People with high GABA/low serotonin are typically calm and gregarious, whereas GABA deficiency and elevated serotonin is associated with anxiety, fear, depression, short temper, phobias, impulsiveness and disorganization.
Another important strategy is to address your gut health. When complex carbs that aren’t digested in your stomach travel down to your intestine, they end up feeding gram-negative bacteria that produce endotoxin, also known as LPS (lipopolysaccharide).
Endotoxin catalyzes a series of metabolic reactions that converts tryptophan in your gut to serotonin. So, to inhibit serotonin production in your gut (which is where most of the serotonin in your body is produced), you want to prevent endotoxin production, which means you need to balance your gut microbiome. Here are a few strategies to do that:
| Pre- and probiotics — Eat prebiotic foods such as onions, garlic, leeks, asparagus and bananas, and probiotic fermented foods like yogurt, kefir, kimchi and sauerkraut. Alternatively, take a probiotic supplement. Beneficial bacteria such as Bifidobacteria and Lactobacillus, and beneficial yeast like Saccharomyces boulardii, can all help rein in the endotoxin production through competitive inhibition. |
| Limit sugar and refined carbohydrates — High intake of sugar and refined carbohydrates can feed harmful bacteria in the gut and promote inflammation, potentially increasing endotoxin production. |
| Avoid resistant starches — Other carbs to avoid would be resistant starches from legumes, beans, lentils, most grains, green bananas, sushi rice and pasta. Oatmeal can also cause trouble for many. You’ll know it’s incompatible with you if you get gas and/or constipation, or if it slows your digestion. Oatmeal is also high in linoleic acid (LA), which is why I avoid it.
If you have small intestinal bacterial overgrowth (SIBO), you may also need to avoid starches like rice and cooked potatoes, as you have inhibited ability to break down the starch into glucose. As a result, these kinds of starches may impede your recovery. |
| Eat plenty of antioxidant-rich whole foods — Foods rich in antioxidants, such as berries, leafy greens, and other colorful fruits and vegetables, can help reduce oxidative stress and inflammation in the gut, thereby supporting gut health and reducing endotoxin production. |
| Choose healthy fats such as those found in avocados, coconut oil, organic grass fed butter and ghee to help reduce gut inflammation. |
| Optimize your omega-3 level — Consuming omega-3 fats from sources like fatty fish (salmon, mackerel, sardines) may help reduce gut inflammation and promote a healthy gut microbiome. |
Prolonged Estrogen Exposure Linked to Alzheimer’s Severity
Other research,15 published in October 2021, linked prolonged estrogen exposure to Alzheimer’s severity in women. This is particularly notable considering nearly two-thirds of Alzheimer’s patients are women.16 Estrogen is also a known carcinogen.17 As reported by Dinkov:18
“The study is pretty straightforward in its claim that longer exposure to endogenous estrogen was associated with exacerbated/higher biomarkers of Alzheimer disease (AD), as well as lower glucose metabolism and smaller brain volume in women.
Another interesting link the study mentions, which is relevant for both sexes, is that lower testosterone levels are also associated with exacerbated/higher biomarkers of AD. The earlier puberty and earlier menopause associations also mean shorter exposure to progesterone. As such, the study can be summarized with the simple statement that estrogen is detrimental while progesterone and testosterone are protective against AD.”
There are two key ways to lower your estrogen:
1. Avoiding estrogen replacement therapy and minimizing exposure to estrogenic compounds found in hundreds of consumer products.19 Opt for natural and organic personal care products, including makeup, skin care, and hair care items, to reduce exposure to synthetic chemicals like parabens and phthalates, which have estrogenic properties.
Ditto for household cleaning products, laundry detergents and air fresheners, many of which contain chemicals with estrogenic properties. Swap them out for natural, nontoxic alternatives or make your own cleaning solutions using vinegar, baking soda and essential oils instead.
Also minimize your use of plastic containers and food packaging, which can leach estrogenic compounds into food and beverages. Instead, opt for glass or stainless steel containers for food storage and water bottles.
2. Taking natural progesterone. Most formulations are not effective as they are oral or transdermal. Ideally, pure progesterone powder should be dissolved in a high-quality vitamin E with MCT oil and rubbed on your gums. Typical doses are 25 to 50 mg once or twice a day.
In my view, what mature women really need are progesterone and pregnenolone, not estrogen. In practical terms, you’ll want to make sure your levels of progesterone and pregnenolone are within healthy limits (the levels you’d have in your 20s), which is around 30 mg a day.
Mitochondrial Dysfunction Is at the Heart of Alzheimer’s
Nearly a quarter century ago, the late Ray Peat, a biologist and “father” of bioenergetic medicine, argued that Alzheimer’s and aging are two examples of what happens when you have poor mitochondrial function, resulting in declining energy production. He presented this hypothesis in two extensive articles.20,21
In the second article, he specifically addressed the role of estrogen and polyunsaturated fats (PUFAs) like LA, as well as the protective influence of progesterone. He wrote, in part:22
“Estrogen stimulates cell division, but can also increase the rate of cell death. Unsaturated fatty acids can also stimulate or kill … Besides increasing the free fatty acid concentration, estrogen possibly depresses the level of cholesterol, both of which are changes seen in the senile brain.
Estrogen causes massive alterations of extracellular matrix, and seems to promote dissolution of microtubules (Nemetschek-Gannsler), as calcium does. Unsaturated fats increase calcium uptake by at least some brain cells (H. Katsuki and S. Okuda, 1995.)
Unsaturated fats, like estrogen, increase the permeability of blood vessels. The unsaturated fat causes edema of the brain, inhibits choline uptake, blocking acetylcholine production.
Progesterone is a nerve growth factor, produced by glial cells (oligodendrocytes). It promotes the production of myelin, protects against seizures, and protects cells against free radicals. It protects before conception, during gestation, during growth and puberty, and during aging. It promotes regeneration. Its production is blocked by stress, lipid peroxidation, and an excess of estrogen and iron …
A ‘deficiency’ of polyunsaturated fatty acids leads to altered rates of cellular regeneration and differentiation, a larger brain at birth, improved function of the immune system, decreased inflammation, decreased mortality from endotoxin poisoning, lower susceptibility to lipid peroxidation, increased basal metabolic rate and respiration, increased thyroid function, later puberty and decreases other signs of estrogen dominance.
When dietary PUFA are not available, the body produces a small amount of unsaturated fatty acid (Mead acids), but these do not activate cell systems in the same way that plant-derived PUFAs do, and they are the precursors for an entirely different group of prostaglandins.”
Interestingly, a near-identical argument was laid out in an October 2020 article by Vijay Pande, Ph.D., and Kristen Fortney, titled “The Cure for Aging Might be the Cure for Alzheimer’s:”23
“What we are only now beginning to understand is that the diseases that ultimately kill us are inseparable from the aging process itself. Aging is the root cause. This means that studying these diseases without taking aging into account could be dangerously misleading … and worst of all, impede real progress …
The biggest risk factor for Alzheimer’s isn’t your APOE status; it’s your age. People in their twenties don’t get Alzheimer’s. But after you hit the age of 65, your risk of Alzheimer’s doubles every five years, with your risk reaching nearly one out of three by the time you’re 85.
What if going after this one biggest risk factor is the best vector of attack? Maybe even the only way to truly address it? This isn’t about the vanity of staying younger, about holding on to your good looks or your ability to run an 8 minute mile. It’s about the only concrete possibility we have to cure these diseases.”
How to Optimize Your Mitochondrial Function Through Diet
To optimize your mitochondrial function, you need to address your diet, as the foods you eat are the substrate from which cellular energy is produced. LA wreaks havoc with your cellular machinery and needs to be limited to 5 grams or less per day.
To reach that goal, you need to ditch all processed foods, fast foods and most restaurant foods, as they’re all loaded with or cooked in LA-rich seed oils. Focus on whole and minimally processed foods.
Your macronutrient ratios also matter. As explained in previous articles, including “A Surprising Reason Why You May Need More Carbs in Your Diet,” ideally, you want to burn glucose in the electron transport chain of your mitochondria, and to ensure that, you need to eat enough healthy carbs, and get no more than 35% or so of your daily calories from fat.
If your fat intake is too high, you’ll prevent glucose from being burned in the mitochondria and force it into glycolysis instead, which is a highly inefficient way to produce energy.
Advances Made in Alzheimer’s Diagnosis
While there are few options available once Alzheimer’s sets in, advances in diagnosis are being made. Early diagnosis may at least give you a chance to implement strategies that might slow down its progression, or in an ideal scenario perhaps even reverse it to some degree. Diagnostic tools include:
• A blood test that measures the patterns of 10 specific lipids associated with the plaques found in the brains of people with Alzheimer’s disease. These 10 lipids are highly predictive of whether or not you will suffer cognitive impairment.24
• A blood test that measures “a molecular precursor in the blood that can cause proteins to irregularly fold and clump in the brain, ultimately forming amyloid beta plaques.”25
• A peanut butter smell test — In tests, patients diagnosed with early stage Alzheimer’s experienced a significant difference in their ability to detect the smell of peanut butter between their right and left nostrils.
The left nostril tends to be impaired in those with Alzheimer’s, whereas those with other kinds of dementia experience either no differences in odor detection between the two nostrils, or the right nostril is worse for detecting the smell compared to the left one.
• A 15-minute at-home test called SAGE, which stands for Self-Administered Gerocognitive Examination, can help you assess your risk of Alzheimer’s and dementia.26 If taken at intervals over time, it can also serve as an early warning, if your scores begin to decline. The test can also be used to monitor the condition in those already diagnosed with Alzheimer’s. You can download the SAGE test from the Ohio State University’s website.27
Additional Alzheimer’s Prevention Guidelines
In addition to optimizing your mitochondrial function and avoiding things that raise your serotonin and estrogen, other helpful prevention strategies include:
| Avoid gluten and casein (primarily wheat and pasteurized dairy, but not dairy fat, such as butter) — Research shows that your blood-brain barrier is negatively affected by gluten. Gluten also makes your gut more permeable, which allows proteins to get into your bloodstream, where they don’t belong. That then sensitizes your immune system and promotes inflammation and autoimmunity, both of which play a role in the development of Alzheimer’s. |
| Optimize your gut flora by regularly eating fermented foods or taking a high potency and high-quality probiotic supplement. |
| Make sure you’re getting enough animal-based omega-3 fats, such as krill oil. High intake of the omega-3 fats EPA and DHA help by preventing cell damage caused by Alzheimer’s disease, thereby slowing down its progression and lowering your risk of developing the disorder. |
| Optimize your vitamin D level with safe sun exposure — Strong links between low levels of vitamin D in Alzheimer’s patients and poor outcomes on cognitive tests have been revealed. In one 2023 study, vitamin D reduced dementia risk by 40%. |
| Keep your fasting insulin levels below 3. |
| Eat a nutritious diet, rich in folate — Vegetables, without question, are your best form of folate, and we should all eat plenty of fresh raw veggies every day. Avoid supplements like folic acid, which is the inferior synthetic version of folate. |
| Avoid and eliminate mercury and aluminum from your body — Dental amalgam fillings, which are 50% mercury by weight, are one of the major sources of heavy metal toxicity. Make sure you use a biological dentist to have your amalgams removed. Sources of aluminum include antiperspirants, non-stick cookware and vaccine adjuvants. |
| Make sure your iron isn’t elevated and donate blood if it is — Studies show that iron accumulations in the brain tend to concentrate in areas most affected by Alzheimer’s, namely the frontal cortex and hippocampus. Magnetic resonance imaging tests have also revealed elevated iron in brains affected by Alzheimer’s. |
| Exercise regularly — It’s been suggested that exercise can trigger a change in the way the amyloid precursor protein is metabolized,28 thus slowing down the onset and progression of Alzheimer’s. In one study, women with the highest cardiovascular fitness had an 88% lower risk of dementia than those with moderate fitness. |
| Eat blueberries and other antioxidant-rich foods — Wild blueberries, which have high anthocyanin and antioxidant content, are known to guard against neurological diseases. |
| Challenge your mind daily — Mental stimulation, especially learning something new, such as learning to play an instrument or a new language, is associated with a decreased risk of Alzheimer’s. |
| Avoid anticholinergics and statin drugs — Drugs that block acetylcholine, a nervous system neurotransmitter, have been shown to increase your risk of dementia. These drugs include certain nighttime pain relievers, antihistamines, sleep aids, certain antidepressants, medications to control incontinence, and certain narcotic pain relievers.
Statin drugs are particularly problematic because they suppress the synthesis of cholesterol, deplete your brain of CoQ10 and neurotransmitter precursors, and prevent adequate delivery of essential fatty acids and fat-soluble antioxidants to your brain by inhibiting the production of the indispensable carrier biomolecule known as low-density lipoprotein. |
– Sources and References
- 1, 2, 5, 16 ALZ.org AD Facts and Figures
- 3 Time Magazine March 5, 2014
- 4 Alzheimer’s Association March 14, 2023; 19(4): 1598-1695
- 6, 8 CNN Health March 5, 2014
- 7 Neurology March 5, 2014 [Epub ahead of print]
- 9 CNN Health April 12, 2011 (Archived)
- 10 Journal of Alzheimer’s Disease September 2023; 96(1): 215-227
- 11 IosPress.com, Journal of Alzheimer’s Disease September 2023; 96(1): 215-227
- 12 Haidut.me February 20, 2024 (Archived)
- 13 UPI.com December 11, 2023
- 14 Neuroscience News December 7, 2023
- 15 Menopause October 2021; 28(10): 1099-1107
- 17 Science Daily December 13, 2002
- 18 Haidut.me March 30, 2022 (Archived)
- 19 Environmental Health News January 10, 2024
- 20 Ray Peat Alzheimer’s Part 1
- 21, 22 Ray Peat Alzheimer’s Part 2
- 23 A16z.com October 7, 2020
- 24 NBC News March 9, 2014
- 25 Science Alert December 22, 2022
- 26 Journal of Neuropsychiatry and Clinical Neurosciences January 13, 2014 [Epub ahead of print]
- 27 Ohio State University, SAGE Test
- 28 Journal of Neuroscience, April 27, 2005: 25(17); 4217-4221
‘Long Vax’ Finally Enters Lexicon
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/05/covid-vaccine-long-vax.aspx
Analysis by Dr. Joseph Mercola April 05, 2024

Story at-a-glance
- Dr. Pierre Kory and Dr. Paul Marik are trying to get the word out that long vax is not only real but has disabled many Americans who were at the peak of health prior to getting a COVID jab
- At Kory’s long COVID clinic, 70% of the patients actually have long vax and reported their symptoms began “minutes, hours, days or several weeks” after receiving a COVID-19 shot
- Long vax symptoms are nearly identical to those of long COVID — the difference being that the long vax patients tend to be sicker, with more frequent small fiber neuropathy and dysautonomia
- A study by Yale scientists detailed long vax, which they called chronic post-vaccination syndrome, in 241 people
- Top reported symptoms include exercise intolerance, excessive fatigue, numbness, brain fog and neuropathy
An estimated 6.4% of U.S. adults have experienced symptoms of long COVID, a term used to describe a complex disorder that persists for three or more months after contracting COVID-19.1 While long COVID has been extensively covered in the media, millions more suffer from long vax — a condition with nearly identical symptoms to long COVID, but often even more severe.
New York pulmonologist Dr. Pierre Kory and Dr. Paul Marik, a critical care doctor formerly with Sentara Norfolk General Hospital in East Virginia, are part of the Front Line COVID-19 Critical Care Working Group (FLCCC). They’re trying to get the word out that long vax is not only real but has disabled many Americans who were at the peak of health prior to getting a COVID jab.2
At Long COVID Clinic, 70% of Patients Have Long Vax
Kory opened a tele-health practice that specializes in treating COVID disease, including long COVID. Kory says:3
“Long COVID, although a new name, is not a new disease. It meets the diagnostic criteria for a decades-old condition called myalgic encephalitis/chronic fatigue syndrome (ME/CFS).
The three symptom ‘pillars’ which lead to the diagnosis are fatigue, post-exertional malaise (PEM), and ‘brain fog’ (i.e. cognitive deficits ranging from word finding difficulties, short term memory loss, inability to focus/comprehend, and more rarely confusion or disorientation).
Although this triad is present in nearly every patient I see (rarely brain fog is missing), the patients also present with a ‘side menu’ of problems which can include sensory neuropathies, dysautonomia/POTS, motor neuropathies, abdominal issues, musculoskeletal complaints, and cranial symptoms (i.e tinnitus, vertigo, headaches, vision, hearing loss, smell loss, taste loss).
Many of my patients are debilitated and meet criteria for disability, despite the majority reporting being in the peak of health and functioning prior to the pandemic.”
Yet, Kory and colleagues quickly noticed that most of their patients reported their symptoms began “minutes, hours, days or several weeks”4 after receiving a COVID-19 shot. While many had also had COVID-19, only a small number tied their symptoms to the viral infection.
While the team initially called the condition post-COVID vaccine injury syndrome, they changed the diagnosis to “long vax” because the symptoms were so close to long COVID — the difference being that the long vax patients tended to be sicker, with more frequent small fiber neuropathy and dysautonomia, Kory said.5
Research Details Neuropathic Symptoms Following COVID-19 Jabs
Scientific studies detailing long vax symptoms continue to emerge. In one study from early in the pandemic, more than two-thirds of those reporting long COVID symptoms had negative antibody tests, suggesting at least some of them didn’t even have COVID-19.6 Meanwhile, many COVID jab recipients report long COVID-like symptoms.
As reported by Science magazine in 2022, “In rare cases, coronavirus vaccines may cause long COVID-like symptoms,”7 which can include (but is not limited to) brain fog, memory problems, headaches, blurred vision, loss of smell, nerve pain, heart rate fluctuations, dramatic blood pressure swings and muscle weakness. The feeling of “internal electric shocks” are also reported.
Also in 2022, a preprint study from the U.S. National Institutes of Health reported new neuropathic symptoms that began in 23 adults within one month of receiving a COVID-19 shot.8 All of the patients felt severe tingling or numbness in their faces or limbs, and 61% also experienced dizziness when standing up, intolerance to heat and heart palpitations.
When 12 of the patients had their nerve function tested, seven had less sweating in their hands and feet than normal, while six had a condition where their heart beats too fast when they stand up.9
The researchers also took skin samples from the lower legs of 16 patients. Among them, 31% showed signs that the small nerves in the skin were not as dense as they should be, which can indicate nerve damage. Another 13% were on the border of being considered damaged, and 19% had swollen nerve fibers. When five of the samples were evaluated more closely, signs of an immune reaction in the blood vessels were detected.10
Further, while electrical tests on the nerves were normal for most participants, 52% showed clear signs of damage to the small nerves that can be felt but not easily seen. The study shows that after getting the COVID-19 shot, a range of symptoms related to nerve damage is possible, which might be caused by an immune system reaction.

Save This Article for Later – Get the PDF Now
Yale Scientists Detail Long Vax Symptoms
A study by Yale scientists, including Dr. Harlan Krumholz of Yale School of Medicine in New Haven, Connecticut, also shed light on long vax, which they described as chronic post-vaccination syndrome, or PVS.11 In a study of 241 people who reported PVS after an mRNA COVID-19 shot, the median time from the jab to the onset of symptoms was three days, with symptoms continuing for 595 days. The five most common symptoms included:12
- Exercise intolerance (71%)
- Excessive fatigue (69%)
- Numbness (63%)
- Brain fog (63%)
- Neuropathy (63%)
In the week before the survey was completed, patients reported a range of additional symptoms highlighting the mental toll the condition takes. The symptoms required a median of 20 interventions for treatment and included:13
| Feeling unease (93%) | Fearfulness (82%) |
| Overwhelmed by worries (81%) | Feelings of helplessness (80%) |
| Anxiety (76%) | Depression (76%) |
| Hopelessness (72%) | Worthlessness (49%) |
“In this study,” the researchers explained, “individuals who reported PVS after COVID-19 vaccination had low health status, high symptom burden, and high psychosocial stress despite trying many treatments. There is a need for continued investigation to understand and treat this condition.”14
Even a 2021 study reported a series of patients who experienced new autoimmune conditions — or flare-ups of existing autoimmune disease — following mRNA COVID-19 shots,15 highlighting the importance of careful research into the ongoing health risks.
Will Long Vax Be Censored?
It’s hopeful that scientific on long vax is reaching medical journals and getting some media coverage.16 But Kory and Marik are concerned it could reach a similar fate as other COVID shot coverage during the pandemic.
“The concern is that our findings, Krumholz’s study, and any reports of adverse events from COVID-19 vaccination, will be subject to the same institutional censorship we saw throughout the pandemic. Suppressing this information risks creating an even bigger disaster,” they told The Hill,17 referring to a potential epidemic of autoimmune diseases that could occur as a result.
“America’s health agencies need to snap into action to help study this problem so we can better understand and treat these conditions. Unfortunately, there doesn’t seem to be much hope of this happening,” Kory and Marik wrote. “The National Institutes of Health is fixated on studying the effect of Paxlovid, an antiviral COVID treatment, to treat long COVID and long vax, despite it having no proven effect on autoimmune disease.”18
Further, Kory explains that while major medical centers and hospitals across the U.S. have opened long COVID clinics, the treatments they offer are largely ineffective, and they often gas-lit long vax patients who tried to get help:19
“[F]or most of 2022 into 2023, those centers consistently gas-lit the Long Vax patients who presented to those clinics. Gaslighting of medical injuries is the well-described inability for physicians to recognize or accept when their own treatments (i.e the mRNA vaccines) cause harm …
The stories my patients would tell me of the care they received included what I would describe as abuse or insults from the treating physicians when the patients tried to convince them that the vaccines were the cause. These stories still make my blood boil and have estranged many of my patients from ‘the system.’ I believe the gaslighting responses have lessened somewhat but I don’t really know how much.
What angered me even further is that the health agencies only directed funding at long COVID and the medical literature and media only referred to sufferers as having long COVID. The contribution of the gene therapy vaccines are consistently ignored.”
Is Long Vax Behind the Explosion of Disability Claims?
Kory believes that long vax, and to a lesser extent long COVID, are behind the explosion of disability claims that have occurred since COVID-19 shots rolled out.20
Data compiled by former BlackRock analyst and fund manager Edward Dowd revealed a sobering glimpse into the true carnage that occurred at the hands of the COVID-19 shot campaign,21 and its results are striking. It revealed the following estimated human and economic costs:22
Human cost:
- 26.6 million injuries
- 1.36 million disabilities
- 300,000 excess deaths
Economic cost:
- Total: $147.8 billion
- Injuries: $89.9 billion
- Disabilities: $52.2 billion
- Excess deaths: $5.6 billion
What’s more, this data is from the employed population, aged 16 to 64 — a typically healthy crowd. To put this into perspective, John Leake writes on Courageous Discourse, “Note that this death count in one year is 5.2 times the number of men killed in ten years of combat in Vietnam.”23
Help for Long Vax Symptoms
As long vax and its symptoms become increasingly recognized, it will hopefully lead to increased access to effective treatments. If you’re experiencing symptoms, it’s important to find a holistic health care practitioner who’s familiar with long vax and how to treat it. You can also access FLCCC’s I-RECOVER24 guide,25 which offers step-by-step instructions on how to treat reactions from COVID-19 injections.26
I also summarized strategies to optimize mitochondrial health if you’re suffering from long COVID or long vax, with a focus on boosting mitochondrial health. To allow your body to heal you’ll want to minimize EMF exposure as much as possible. Your diet also matters, as the cristae of the inner membrane of the mitochondria contains a fat called cardiolipin, the function of which is dependent on the type of fat you get from your diet.
The type of dietary fat that promotes healthy cardiolipin is omega-3 fat, and the type that destroys it is omega-6, especially linoleic acid (LA), which is highly susceptible to oxidation. So, to optimize your mitochondrial function, you want to avoid LA as much as possible and increase your intake of omega-3s.
Primary sources of LA include seed oils used in cooking, processed foods and restaurant foods made with seed oils, condiments, seeds and nuts, most olive oils and avocado oils (due to the high prevalence of adulteration with cheaper seed oils). Animal foods raised on grains, such as conventional chicken and pork, are also high in LA.
Another major culprit that destroys mitochondrial function is excess iron — and almost everyone has too much iron. You can learn more about the health risks of excess iron in my interview with Christy Sutton, D.C. The most effective way to lower your iron is to donate blood two to four times a year.
Copper is also important for energy metabolism, detoxification and mitochondrial function, and copper deficiency is common. Other strategies include sun exposure and near-infrared light therapy, NAD+ optimizers and methylene blue, which can be a valuable rescue remedy. By improving your mitochondrial function and restoring the energy supply to your cells, you’ll significantly increase your odds of reversing the problems caused by the jab or the virus.
- 1 U.S. CDC, MMWR February 15, 2024 / 73(6);135–136
- 2, 3, 4, 5, 19, 20 Pierre Kory’s Medical Musings March 8, 2024
- 6 TNR December 8, 2022
- 7 Science January 20, 2022
- 8, 9, 10 medRxiv May 17, 2022
- 11, 12, 13, 14 medRxiv November 10, 2023
- 15 Int Immunopharmacol. 2021 Oct:99:107970. doi: 10.1016/j.intimp.2021.107970. Epub 2021 Jul 10
- 16, 17, 18 The Hill March 6, 2024
- 21 Phinance Technologies, The Vaccine Damage Project March 2023
- 22 Zero Hedge March 28, 2023
- 23 Substack, Courageous Discourse March 29, 2023
- 24, 25 FLCCC Alliance, I-RECOVER
- 26 FLCCC Alliance, I-RECOVER, Post-Vaccine Treatment Guide
The Subtle Early Signals of Dementia in Someone You Love
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/03/26/early-dementia-sign.aspx
Analysis by Dr. Joseph Mercola March 26, 2024
STORY AT-A-GLANCE
- Before memory and thinking problems become obvious, people with dementia may display changes in mood and behavior
- In the early stages of the disease, irritability, anxiety or depression may occur
- Apathy is another common sign, although some people may display more blatant changes like suddenly becoming sexually promiscuous or developing the habit of snatching food off other people’s plates
- Alzheimer’s disease is the result of poor mitochondrial function; to optimize your mitochondrial function, you need to limit your intake linoleic acid (LA) to 5 grams a day or less
- To achieve this, you’ll need to eliminate all processed foods, fast foods and the majority of restaurant meals, which are frequently loaded with or prepared using seed oils high in LA
Worldwide, more than 55 million people are living with dementia, and each year nearly 10 million new cases occur.1 Dementia is not a disease in itself but rather a term used to describe a number of different brain illnesses that may affect your memory, thinking, behavior and ability to perform everyday activities. The most common type of dementia is Alzheimer’s disease, which accounts for up to 70% of cases.2
Many people associate dementia with memory loss — and this is a red flag — however, not all memory problems are due to Alzheimer’s (and some causes of dementia-like symptoms, including memory loss, can be reversed, such as those related to thyroid problems and vitamin deficiencies).3
If you’ve noticed yourself or a loved one becoming increasingly forgetful or experiencing changes in thinking abilities, you should see a health care provider right away. Oftentimes, however, the first symptoms are so subtle they may be easily missed — and they may manifest as changes in behavior and mood long before memory problems become apparent.
Fortunately, there are two crucial prevention strategies that remain largely underdiscussed yet are relatively simple to implement — reducing linoleic acid (LA) intake and limiting exposure to estrogen.
Pay Attention to Personality Changes — An Early Sign of Dementia
Before memory and thinking problems become obvious, people with dementia may display changes in mood and behavior, according to a team of neuropsychiatrists and Alzheimer’s experts, who say the latter symptoms may be among the earliest signs of dementia.
The team released a 34-question checklist they believe could help diagnosis a new condition called mild behavioral impairment (MBI).4 Similar to mild cognitive impairment (MCI), which is defined by a noticeable decline in cognitive abilities that does not yet interfere with most daily functions, MBI describes changes in behavior and mood that may occur prior to MCI and the cognitive changes associated with dementia.
The checklist is intended to identify patients at risk of dementia earlier, as according study author Dr. Zahinoor Ismail, a neuropsychiatrist at the University of Calgary, among people with MCI, those with mood and behavior changes will progress to full-blown dementia faster.5 Some have expressed concern that the checklist may lead to overdiagnosis or false diagnosis, putting some people through increased medical testing and worry unnecessarily.
In the case of MCI, for instance, not everyone diagnosed will go on to develop Alzheimer’s or other types of dementia. In fact, The New York Times reported, up to 20% of those with MCI later turn out to be cognitively normal.6
Still, others say keeping an eye out for unusual behavioral or personality changes can help people get help, at least symptom relief, faster. Sadly, there is currently no cure for Alzheimer’s disease and, as it progresses, the disease is devastating not only for those diagnosed but also their friends and family. Prevention remains the best option, and I detail steps that can help below.
Behavioral and Mood Changes to Watch Out For
Dementia manifests differently in everyone, which is why the most important changes to watch out for are those that are unusual for your loved one. A person may, for instance, stop doing something they’ve always loved to do, be it cooking a certain dish for your birthday or watching the evening news.
Apathy is another common sign, although some people may display more blatant changes like suddenly becoming sexually promiscuous or developing the habit of snatching food off other people’s plates.7 The Alzheimer’s Association noted:8
“Individuals living with Alzheimer’s or other dementia may experience mood and personality changes. They can become confused, suspicious, depressed, fearful or anxious. They may be easily upset at home, with friends or when out of their comfort zone.”
In the early stages of the disease, irritability, anxiety or depression may occur. In fact, a study published in the journal Neurology not only found that people who eventually developed dementia were twice as likely to develop depression earlier on in their lives, but they also tended to display mood changes in a consistent pattern.9 Time reported:10
“The symptoms appeared in consistent phases: first, irritability, depression and nighttime behavior changes; followed by anxiety, appetite changes, agitation and apathy. The final phase was elation, motor disturbances, hallucinations, delusions and disinhibition.”
In order for early mood and/or behavioral changes to be considered MBI, the change in behavior must persist for at least six months.

Save This Article for Later – Get the PDF Now
Signs of Mild Cognitive Impairment
In some people, MCI may follow the earliest changes in mood and behavior. MCI is a slight decline in cognitive abilities that increases your risk of developing more serious dementia, including Alzheimer’s disease, although it is by no means a guarantee. It’s estimated that up to 18% of people aged 60 and older are living with MCI.11
Simply misplacing your keys on occasion is not cause for alarm, however forgetting important information that you would have normally recalled, such as appointments, conversations or recent events, may be a sign. You may also have a harder time making sound decisions, figuring out the sequence of steps needed to complete a task or judging the time needed to do so.
If you’ve been diagnosed with MCI, be aware that some cases do not progress and may even improve. Regular exercise, proper diet — including reducing your intake of LA — and engaging in mentally and socially stimulating activities may help to boost your brainpower.
Dementia: When to Worry?
It can be difficult to gauge if a loved one is declining mentally. If you have suspicions but aren’t sure, try keeping a notebook to jot down instances that concern you. You may be able to identify a pattern of events that makes the picture clearer.
Agnes B. Juhasz, nurse, dementia care specialist and author of ‘The Dementia Whisperer: Scenes From the Frontline of Caring,’ suggested making note of anything out of ordinary for that particular person. She wrote in the [U.K.]’s Mirror news:12
“Naturally, there are a few typical signs and possible changes that are worth watching out for more closely. These include the level of forgetfulness; acute or permanent confusion about certain things; disorientation in time and place; significant changes in behavior and personality; decreased judgment; changes in speech or writing; and withdrawal from social interactions and activities.
But all these suggested signs ultimately lead us back to the essential, magical question we always have to ask before we can arrive at any further conclusions: ‘Is this abnormal for this individual, or is it part of who they have always been?’ When we notice that something is new and odd, that has never occurred in a person’s life before, as far as we have observed, that is the point when further help may be needed.”
Early Warning Signs of Alzheimer’s
While an absent-minded mistake, like putting a mug in the wrong cabinet, is not cause for alarm, feeling confused about day-to-day tasks is.
Losing interest in hobbies, repetitive behaviors (phrases, gestures or questions), mispronouncing words or stuttering can also be signs. And while occasional forgetfulness, like forgetting why you were walking into a room, is not typically reason to worry, more profound confusion, like the room itself feeling unfamiliar, may signal a problem.13
The Alzheimer’s Association also compiled differences between symptoms of dementia, including Alzheimer’s, and typical age-related changes:14
| Signs of Alzheimer’s/dementia | Typical age-related changes |
|---|---|
| Poor judgment and decision-making | Making a bad decision once in a while |
| Inability to manage a budget | Missing a monthly payment |
| Losing track of the date or the season | Forgetting which day it is and remembering it later |
| Difficulty having a conversation | Sometimes forgetting which word to use |
| Misplacing things and being unable to retrace steps to find them | Losing things from time to time |
Why Addressing Mitochondrial Dysfunction by Reducing LA Is Key
Work by the late Ray Peat, a biologist and “father” of bioenergetic medicine, suggests Alzheimer’s disease is the result of poor mitochondrial function, which results in reduced energy production.15,16
To optimize your mitochondrial function, you need to address your diet, as the foods you eat are the substrate from which cellular energy is produced. LA wreaks havoc with your cellular machinery, which is why it should be limited to 5 grams or less per day.
To achieve this, you’ll need to eliminate all processed foods, fast foods and the majority of restaurant meals, which are frequently loaded with or prepared using seed oils high in LA. Instead, prioritize whole and minimally processed foods.
In addition to limiting LA in your diet, carnosine, a dipeptide composed of two amino acids — beta-alanine and histidine — is a crucial aid for LA detoxification, as it binds to advanced lipoxidation endproducts (ALEs) that form from oxidized seed oils in your diet.
While your body will slowly eliminate stored LA over time, provided you reduce your intake, carnosine can help reduce the oxidative damage caused by LA while your body is cleaning itself out. I take liposomal carnosine every day before meals to help detoxify LA.
LA is highly susceptible to oxidation, and as the fat oxidizes it breaks down into harmful sub-components such as ALEs and oxidized LA metabolites (OXLAMs). These ALEs and OXLAMs are what cause most of the damage.
Carnosine binds to ALEs like a magnet and acts as a sacrificial sink. It’s basically a substitute target for these profoundly damaging molecules. In this way, carnosine allows your body to excrete the ALEs from your body before they damage your mitochondria, DNA or proteins.
As an added benefit, carnosine is protective against Alzheimer’s,17 due to its ability to scavenge 4-hydroxynonenal (4HNE), a biomarker of oxidative stress that may increase the harm caused by free radicals.
Elevated Serotonin Linked to Dementia
High serotonin levels are also linked to dementia.18 While often described as the “happy hormone,” serotonin, a chemical messenger in the brain, acts as an antimetabolite, hindering energy production in your mitochondria. A September 2023 study found that having low levels of serotonin transporter (SERT) is linked to problems with memory and thinking skills, which can eventually lead to dementia or Alzheimer’s disease.
SERT is like a “cleanup crew” in the brain, helping to remove excess serotonin. When there’s not enough SERT around to do its job, serotonin levels outside of brain cells can rise too high. This excess serotonin floating around can cause trouble and contribute to problems with memory and thinking.
Considering that high extracellular serotonin can contribute to dementia, you’d be wise to keep your serotonin level as low as possible. One way to do that is by increasing GABA, which is available as a supplement.
The Estrogen Connection
Alzheimer’s disease (AD) is more common in women than men,19 and prolonged estrogen exposure is also linked to Alzheimer’s severity in women.20 As bioenergetic researcher Georgi Dinkov explained, “The study can be summarized with the simple statement that estrogen is detrimental while progesterone and testosterone are protective against AD.”21
Avoiding estrogen replacement therapy and minimizing your exposure to the estrogenic compounds found in hundreds of consumer products is therefore an important step to protecting your brain health.
Taking natural progesterone is also important, but be aware that most formulations are not effective as they are oral or transdermal. Ideally, pure progesterone powder should be dissolved in a high-quality vitamin E with MCT oil and rubbed on your gums. Typical doses are 25 to 50 milligrams once or twice a day.
In my view, what mature women really need are progesterone and pregnenolone, not estrogen. In practical terms, you’ll want to make sure your levels of progesterone and pregnenolone are within healthy limits (the levels you’d have in your 20s), which is around 30 mg a day.
More Tips to Prevent Alzheimer’s Disease
In addition to optimizing your mitochondrial function, lowering your intake of LA and avoiding things that raise your serotonin and estrogen, other helpful Alzheimer’s prevention strategies include:
| Avoid gluten and casein (primarily wheat and pasteurized dairy, but not dairy fat, such as butter) — Research shows that your blood-brain barrier is negatively affected by gluten. Gluten also makes your gut more permeable, which allows proteins to get into your bloodstream, where they don’t belong. That then sensitizes your immune system and promotes inflammation and autoimmunity, both of which play a role in the development of Alzheimer’s. |
| Optimize your gut flora by regularly eating fermented foods or taking a high potency and high-quality probiotic supplement. |
| Make sure you’re getting enough animal-based omega-3 fats, such as krill oil. High intake of the omega-3 fats EPA and DHA help by preventing cell damage caused by Alzheimer’s disease, thereby slowing down its progression and lowering your risk of developing the disorder. |
| Optimize your vitamin D level with safe sun exposure — Strong links between low levels of vitamin D in Alzheimer’s patients and poor outcomes on cognitive tests have been revealed. In one 2023 study, vitamin D reduced dementia risk by 40%. |
| Keep your fasting insulin levels below 3. |
| Eat a nutritious diet, rich in folate — Vegetables, without question, are your best form of folate, and we should all eat plenty of fresh raw veggies every day. Avoid supplements like folic acid, which is the inferior synthetic version of folate. |
| Avoid and eliminate mercury and aluminum from your body — Dental amalgam fillings, which are 50% mercury by weight, are one of the major sources of heavy metal toxicity. Make sure you use a biological dentist to have your amalgams removed. Sources of aluminum include antiperspirants, nonstick cookware and vaccine adjuvants. |
| Make sure your iron isn’t elevated and donate blood if it is — Studies show that iron accumulations in the brain tend to concentrate in areas most affected by Alzheimer’s, namely the frontal cortex and hippocampus. Magnetic resonance imaging tests have also revealed elevated iron in brains affected by Alzheimer’s. |
| Exercise regularly — It’s been suggested that exercise can trigger a change in the way the amyloid precursor protein is metabolized,22 thus slowing down the onset and progression of Alzheimer’s. In one study, women with the highest cardiovascular fitness had an 88% lower risk of dementia than those with moderate fitness. |
| Eat blueberries and other antioxidant-rich foods — Wild blueberries, which have high anthocyanin and antioxidant content, are known to guard against neurological diseases. |
| Challenge your mind daily — Mental stimulation, especially learning something new, such as how to play an instrument or speak a new language, is associated with a decreased risk of Alzheimer’s. |
| Avoid anticholinergics and statin drugs — Drugs that block acetylcholine, a nervous system neurotransmitter, have been shown to increase your risk of dementia. These drugs include certain nighttime pain relievers, antihistamines, sleep aids, certain antidepressants, medications to control incontinence and certain narcotic pain relievers.
Statin drugs are particularly problematic because they suppress the synthesis of cholesterol, deplete your brain of CoQ10 and neurotransmitter precursors, and prevent adequate delivery of essential fatty acids and fat-soluble antioxidants to your brain by inhibiting the production of the indispensable carrier biomolecule known as low-density lipoprotein. |
– Sources and References
- 1, 2 World Health Organization, Dementia March 15, 2023
- 3 Alzheimer’s Association, What Is Dementia?
- 4 J Alzheimers Dis. 2017; 56(3): 929–938
- 5, 6, 7 The New York Times July 26, 2016
- 8, 14 Alzheimer’s Association, 10 Early Signs and Symptoms of Alzheimer’s and Dementia
- 9 Neurology February 10, 2015, 84(6) 617-622
- 10 Time January 14, 2015
- 11 Alzheimer’s Association, Mild Cognitive Impairment
- 12 Mirror November 9, 2016
- 13 Independent December 2015
- 15 Ray Peat Alzheimer’s Part 1
- 16 Ray Peat Alzheimer’s Part 2
- 17 Pharmaceuticals June 2023; 16(6): 778
- 18 Journal of Alzheimer’s Disease September 2023; 96(1): 215-227
- 19 ALZ.org AD Facts and Figures
- 20 Menopause October 2021; 28(10): 1099-1107
- 21 Haidut.me March 30, 2022 (Archived)
- 22 Journal of Neuroscience, April 27, 2005: 25(17); 4217-4221