Linoleic Acid
now browsing by category
The American Academy of Pediatrics — Mining Children for Profit
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/09/30/aap-mining-children-for-profit.aspx
Analysis by Dr. Joseph Mercola September 30, 2025

Story at-a-glance
- The American Academy of Pediatrics (AAP) is heavily funded by pharmaceutical companies, influencing policies that promote more medical interventions for children while reducing parental control
- The AAP’s top priority is to eliminate parental authority over childhood vaccination decisions, replacing it with state or provider control
- Major child health issues like rising obesity, increasing autism rates, and chronic illness prevention are absent from the AAP’s top 10 priorities
- The AAP uses rare measles outbreaks to justify removing personal and religious vaccine exemptions, despite measles mortality already being near zero before mass vaccination began
- Ignoring preventive strategies, the AAP’s approach sets children up for lifelong dependence on pharmaceutical products rather than building lasting health
In North America, the American Academy of Pediatrics (AAP) holds enormous influence over how children’s medical care is shaped. Its public positions and policy priorities steer the direction of pediatric practice, often setting the tone for what’s considered standard care. What’s less visible is how those priorities are formed, and how the balance between child health, industry interests, and parental authority is struck.
Over the past several decades, the health landscape for children has shifted dramatically, with chronic illness becoming far more common. Yet the way the AAP addresses these changes reveals as much about its focus as it does about what it leaves out. By examining what the organization elevates — and what it avoids — it becomes clear how policy direction affects the day-to-day decisions parents face.
This isn’t just about medical recommendations; it’s about the framework that decides whether prevention, treatment, or industry-driven measures take center stage. The details of the AAP’s own published priorities show where the balance tips, and why the very first item on their list directly impacts your ability to make informed choices for your child.
AAP’s Priorities Reveal a Profound Shift Away from Parental Rights
The AAP is structured to prioritize its members’ income over children’s well-being, according to David Bell, senior scholar at Brownstone Institute and a former medical officer and scientist at the World Health Organization (WHO).1 The published article by the Brownstone Institute outlines how the AAP’s top priority is to remove parents from decision-making about whether their children receive certain medical procedures, especially vaccinations.
With 67,000 members in the U.S., Canada, and Mexico, the AAP’s influence is enormous. Its funding from pharmaceutical companies like Moderna, Merck, Sanofi, and GlaxoSmithKline creates a direct financial link between the organization’s policy positions and industry profit.
• The organization’s published priorities reveal striking omissions that directly affect children’s health outcomes — Among its top 10 goals, the AAP does not address three of the most urgent and widely discussed issues affecting children today: increasing obesity, the autism epidemic, and the overall rise in chronic illness.
While these problems are acknowledged elsewhere by the AAP, the focus is on managing — not preventing — them. This means that as a parent, you’re unlikely to see the organization push for real, root-cause solutions that would improve your child’s long-term health.
• Its strategy aligns with creating lifelong pharmaceutical customers rather than fostering lifelong health — The article points out that promoting chronic illness in children nearly guarantees those conditions will persist into adulthood, ensuring ongoing revenue for drug manufacturers. This isn’t simply a byproduct of flawed policy — it’s an outcome that benefits the same corporations funding the AAP.
• The AAP’s stance on bodily autonomy erodes long-standing human rights norms — The group operates on the view that personal medical decisions should be subordinate to state requirements or a doctor’s orders, even when those orders involve products the doctor is financially incentivized to promote.
This approach mirrors early 20th-century technocracy and medical authoritarianism, where “experts” made health care decisions without patient consent. For you, this translates into diminished control over your child’s body and health choices.
• Their vaccine policies ignore the reality of already low measles mortality before mass vaccination began — In the U.S. and other wealthy nations, nearly all measles-related deaths had already ended before the introduction of mass vaccination programs. Improved nutrition, especially in micronutrients, was likely the key factor. This is important context, because it challenges the AAP’s justification for overriding parental choice based on rare outbreaks.
Financial Influence Drives Pediatric Policy Choices
When an organization receives funding from companies whose business model depends on high product use, the policies it produces will often reflect those companies’ commercial priorities. In this case, it means promoting more pharmaceutical interventions for children, removing parental veto power, and ignoring preventive health strategies that would reduce dependency on medical products.
• AAP uses selective statistics to justify eliminating exemptions — Dr. Jesse Hackell, chair of the AAP’s Committee on Pediatric Workforce, cited the deaths of two children in recent years from measles to argue for removing personal choice.
The article stresses that claiming vaccines are “safe” without acknowledging that they carry risks and cause adverse effects is “a stupid claim in medicine and biology.” For you as a parent, this means policy decisions are being made using emotionally charged but statistically rare events, rather than a balanced risk-benefit analysis.
• Religious and cultural objections to certain vaccines are dismissed outright — Many parents have concerns about vaccines developed using cells from induced abortions, yet the AAP officially supports overriding these objections. This disregard for moral or cultural beliefs signals that your deeply held values could be deemed irrelevant in decisions about your child’s care.
• The broader impact is a public health model that treats children as a market, not individuals — The AAP’s actions align less with science-based health care and more with marketing strategies for an expanding pediatric pharmaceutical market. If these priorities succeed, future generations of children will grow up in an environment where medical compliance is enforced, personal choice is diminished, and preventive care is sidelined.
• AAP’s published priorities are a direct signal of where pediatric care is headed — Unless challenged, these policies could mean fewer rights for parents, greater exposure of children to medical interventions without your consent, and an ongoing neglect of prevention-focused health care. Understanding this shift is the first step in protecting your ability to make informed decisions for your child’s long-term well-being.

Save This Article for Later – Get the PDF Now
Practical Steps to Protect Your Child’s Health and Your Right to Decide
When an influential organization pushes policies that remove your voice from your child’s health care, the most effective way to respond is by addressing the root of the problem — both the health risks to your child and the erosion of your authority as a parent. Your goal is twofold: keep your child healthy so they’re less likely to need chronic medical interventions, and take deliberate steps to protect your ability to make informed decisions about their care.
1. Build your child’s health from the inside out — Focus on a diet and lifestyle that supports strong immunity and balanced development. Limit ultraprocessed foods, eliminate vegetable oils, and replace them with nutrient-rich fats like tallow, ghee, or grass fed butter.
Prioritize whole fruits, root vegetables, and quality proteins such as grass fed beef and pastured eggs. A strong nutritional foundation, along with regular daily movement, sound sleep, and stress management, reduces the likelihood your child will need long-term pharmaceutical treatments.
2. Stay informed about medical products and policies — Read the actual policy statements from organizations like the AAP rather than relying on summaries in the media. If you’re a parent who wants full knowledge of what’s being recommended for your child, you need to know exactly what is on the priority list — and what’s missing. Understanding the gaps, such as ignoring obesity or autism prevention, helps you spot when an agenda is driven by profit instead of health.
3. Document your decisions and communicate them clearly — Keep written records of your preferences regarding your child’s care, including your stance on specific medical interventions. If you’re enrolling your child in school or a new activity, provide those documents in advance. This ensures there is no confusion about your expectations and puts your position on record before issues arise.
4. Address chronic illness risks early and naturally — If your child is showing signs of early health problems — such as excess weight gain, fatigue, or developmental concerns — intervene now with lifestyle changes. Increase daily activity, ensure regular outdoor time for sun exposure, and create a consistent sleep routine. By preventing or reversing early issues without medicalizing them, you reduce the likelihood of your child becoming dependent on ongoing drug-based treatments.
5. Engage in local and state-level advocacy — Join parent groups or community organizations that support medical freedom and parental rights. If you’re concerned about policies being pushed at the legislative level, showing up at school board meetings or contacting lawmakers directly is one of the most effective ways to make your voice heard. Organized, informed parents are far more difficult for institutions to ignore.
FAQs About the AAP
Q: What is the main concern with the AAP?
A: The AAP has shifted its focus away from prevention and root-cause solutions for children’s health, prioritizing policies that remove parental authority over medical decisions — especially vaccinations — while receiving funding from major pharmaceutical companies.
Q: Why does the AAP’s funding matter for parents?
A: When an organization is funded by companies that profit from more medical interventions, its policy positions often align with increasing the use of those products. This means parents are more likely to face pressure to comply with recommendations that benefit industry rather than focusing on long-term health outcomes for their children.
Q: What important child health issues are missing from the AAP’s top priorities?
A: The AAP’s published priority list leaves out major public health concerns like rising childhood obesity, increasing autism rates, and the broader epidemic of chronic illness. These omissions suggest a lack of interest in prevention-focused health care strategies.
Q: How does the AAP justify removing parental choice on vaccines?
A: The AAP cites rare measles outbreaks and isolated cases of death to argue for eliminating personal, cultural, or religious exemptions, despite the fact that measles mortality in the U.S. had already dropped to near zero before mass vaccination programs began.
Q: What can parents do to protect their rights and their children’s health?
A: Parents can strengthen their child’s health through nutrition and lifestyle choices, stay informed on medical policies, document care preferences, address health risks early with natural approaches, and participate in local or state advocacy to protect medical decision-making authority.
Unique Protein Provides Clues on How to Extend Lifespan Through Diet
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/09/klotho-protein-longevity.aspx
Analysis by Dr. Joseph Mercola July 09, 2025

Story at-a-glance
- A single protein called klotho extended healthy mice lifespan by 20%, while improving muscle strength, bone density, and cognitive function across multiple body systems
- Klotho functions as a “longevity switch” that naturally declines with age; it’s influenced by lifestyle choices rather than just chronological aging
- Regular moderate exercise, whole-food diets rich in antioxidants and adequate vitamin D significantly boost klotho levels, while overtraining reverses these benefits
- Poor sleep, chronic stress, loneliness, and habits like smoking all decrease klotho production, accelerating the aging process and increasing disease risk
- Scientists are exploring klotho as a biomarker for healthy aging, as low levels correlate with greater risk of cognitive decline, frailty, and early mortality
A single protein, klotho, extended the lifespan of healthy mice by 20% in a study from Molecular Therapy.1 In addition to longer life, these mice also moved better, thought faster and resisted age-related breakdown in muscles, bones, and brain function. Aging brings more than wrinkles. It weakens bones, shrinks muscle, blunts cognition and raises your risk of disease. Klotho works differently than any single drug or supplement.
It doesn’t just address one symptom; it improves how your body handles stress, repairs damage, and maintains organ function across multiple systems. As your klotho levels drop with age, your ability to regenerate tissues declines, your inflammation rises and your risk for conditions like osteoporosis, Alzheimer’s disease, and frailty climbs.
Klotho is a protein your kidneys and brain naturally produce, but only if you’re living in a way that supports that internal machinery. The good news? Your habits — what you eat, how you move, how well you sleep and even how connected you feel to others — all influence your body’s klotho production.
Researchers are calling klotho a “longevity switch,” and one of the most promising ways to measure how well your lifestyle is working. To understand why this matters so much for your long-term health, and what it looks like in practice, let’s break down the latest findings from the gene therapy experiment that helped klotho-deficient animals move, think and live like younger ones.
A Single Injection Extended Lifespan and Rewired Aging from the Inside Out
The Molecular Therapy study tested whether long-term exposure to a specific form of the klotho protein, known as secreted klotho, or s-Klotho, could slow down the aging process in healthy mice.2 Scientists used a specialized virus to deliver the gene that makes s-Klotho directly into the animals’ bloodstream and brain. Unlike many antiaging strategies that target one system, this method aimed to affect multiple organs at once.
• Mice with boosted klotho lived longer and aged better — Treated animals lived longer than untreated mice, but longevity wasn’t the only improvement.3 They also showed fewer signs of age-related decline. Their muscles stayed stronger, their bones remained denser and their brains showed more activity related to regeneration and memory. This suggests klotho extends quality of life, which is what matters most.
• Muscle strength and bone health improved — In strength tests like grip performance and bar hanging, klotho-treated mice performed better, especially when treated during adulthood rather than earlier life. Muscle tissue under the microscope revealed larger fibers and far less scar tissue. After simulated injury, their muscles rebuilt more like those of younger mice.
Bone health improved too. Males who received treatment at middle age had thicker, denser bone structure and smaller gaps in their spongy bone. Females, on the other hand, benefited more when treated earlier, before bone degeneration was advanced. Gene expression testing confirmed more activity in the genes that form strong, mineral-rich bone.
• Brain resilience increased through stem cell activity and immune cleanup — Klotho helped regenerate brain tissue by increasing the number of maturing neurons and maintaining supportive cells called astrocytes. The treated mice also showed more brain immune cells responsible for removing damaged proteins and debris. These were not inflamed cells but highly functional ones, associated with better memory and less age-related inflammation.
• Muscle and brain benefits were linked to reduced inflammation and better cell signaling — Klotho blocked specific age-related pathways known to cause tissue scarring and interfere with stem cell repair. In muscles, it preserved mitochondrial function and kept stem cells capable of rebuilding tissue. In the brain, it promoted neurogenesis — your brain’s ability to grow new neurons — and kept immune cells working efficiently.
• Klotho’s effects showed up in gene expression tied to longevity — Animals that received treatment showed higher expression of genes that build collagen in bone and drive bone formation. They also had lower levels of a gene that typically rises with aging and contributes to poor bone mineralization. In the brain, there was an upregulation of repair pathways and immune functions that target malfunctioning cells.
Your Daily Habits Control Your Body’s Antiaging Switch
A comprehensive review published in Metabolites explored how everyday choices, like how you eat, sleep, move, and manage stress, directly influence your body’s production of klotho.4 The paper proposed using klotho levels as a real-time biomarker to track whether your lifestyle is truly improving your long-term healthspan.
• Klotho tracks with overall well-being, not just disease — Most medical markers only flag disease after it’s already taken hold. But klotho is different; rather than being a disease marker, it’s a health marker. Your levels rise with good habits and fall with harmful ones, making it one of the few tools that could give you feedback on whether your habits are actually helping you age well.
• Moderate, consistent exercise is one of the best ways to raise klotho — Even light daily movement significantly boosted klotho levels, while extreme workouts or stressful conditions — like military training in high heat — lowered them. A 12-trial meta-analysis confirmed that aerobic and resistance training both worked, but overtraining reversed the benefits.
• A healthy diet is directly tied to higher klotho expression — Diets rich in fruits, vegetables, fermented foods, and antioxidants — like vitamin A, C, E, zinc, and selenium — were consistently linked to higher klotho levels.
The Mediterranean-style diet, with a focus on minimally processed foods, stood out in large-scale data, while low-carb diets didn’t help and sometimes made things worse. Vitamin D and curcumin (from turmeric) also triggered klotho production in lab studies.
• Poor sleep, loneliness, and chronic stress all push klotho down — Klotho responds to psychological load. Short sleep (under 5.5 hours) and excessive sleep (over 7.5 hours) both lowered levels. Chronic stress reduced klotho in women caring for sick children and in soldiers under high pressure. Social connection, especially emotional closeness, was correlated with better klotho status, even in middle age.
• Risky habits blunt klotho’s protective effects — Smoking, alcohol, and cannabis all showed negative or inconsistent relationships with klotho. In some cases, the body responded to inflammation by temporarily increasing levels, but this wasn’t protective, it was compensatory. Over time, the cumulative damage from these habits appeared to wear down klotho’s regenerative capacity.

Save This Article for Later – Get the PDF Now
Klotho Is Your Brain and Body’s Aging Thermostat
Published in the Clinical Kidney Journal, a comprehensive review examined how klotho influences aging, cognition, inflammation, and longevity through its effects on phosphate metabolism, vitamin D regulation and multiple molecular signaling pathways.5 The authors pulled together decades of preclinical and clinical evidence to outline how declining klotho levels are tightly linked to both chronic diseases and neurodegeneration.
• Lower klotho levels are consistently tied to shorter lifespan, poor memory, and cognitive decline — Mice that lack the klotho gene show signs of accelerated aging, including cognitive impairment, vascular disease, infertility, and early death. Humans with low klotho levels face higher risks for kidney disease, heart problems, and frailty.
One large national cohort study of 10,069 people found that adults with the lowest serum klotho levels had a 31% higher risk of dying from any cause compared to those with higher levels.
• Your klotho levels drop with age, but not just because you’re getting older — Inflammation, poor diet, and chronic illness all contribute to a decline in klotho expression. For instance, diabetic kidney disease, high blood pressure, and even low oxygen levels reduce klotho.
• Klotho helps your brain clear toxins and protect memory — Soluble klotho is produced in brain regions involved in memory and learning. Studies show it reduces oxidative stress, supports nerve cell repair and protects against damage from Alzheimer’s-related proteins.
Even when administered outside the brain, klotho fragments have been shown to boost synaptic plasticity and learning in mice, suggesting it activates neural repair pathways without needing to cross the blood-brain barrier.
• Klotho blocks the destructive pathways that fuel aging at the cellular level — This includes suppressing a pathway that promotes fibrosis and scarring, damping down signaling that raises inflammation and regulating intracellular calcium to maintain healthy cell function. Klotho also helps manage energy metabolism, antioxidant defense, and tissue regeneration, making it a master regulator of healthy aging.
Klotho Decline Reflects Aging and Disease Severity
Research published in Ageing Research Reviews analyzed klotho levels across 65 studies and confirmed that this antiaging protein consistently decreases with age, even in otherwise healthy people. The decline is more severe in those with kidney, metabolic, or endocrine disorders. Researchers tracked klotho in blood, cerebrospinal fluid (CSF), urine and tissue samples, reinforcing its usefulness as a biomarker for both aging and chronic disease progression.
• Klotho loss accelerates disease — Low klotho levels in the brain have been linked to reduced white matter integrity and greater oxidative stress, according to studies on aged rhesus monkeys.
In both animal and cell models, klotho deficiency led to increased susceptibility to inflammation and neurodegeneration. Restoring klotho, on the other hand, improved cell maturation and reduced inflammation in models of Alzheimer’s, multiple sclerosis, and amyotrophic lateral sclerosis (ALS).
• Baseline klotho levels are essential for future therapies — Because levels of klotho vary so widely by age and disease status, researchers emphasize the importance of establishing personal klotho baselines. Understanding what’s normal at different life stages helps doctors better assess risk and tailor future interventions.
• What this means for you — Monitoring your klotho levels could one day be as routine as checking blood pressure. If this protein turns out to be as central to healthy aging as the evidence suggests, it could help detect early signs of degenerative conditions and open the door to customized, preventative therapies. In short, klotho appears to be key to measuring, and maintaining, your body’s biological resilience over time.
Simple Ways to Activate Your Longevity Switch
If you want to increase your klotho levels and keep them high as you age, you need to focus on the lifestyle habits that trigger its natural production in your body. This isn’t about expensive treatments or supplements — it’s about addressing the root causes of accelerated aging: low cellular energy, chronic stress, poor diet, inactivity, and inflammation.
Klotho doesn’t show up when your system is overloaded. It rises when your body feels safe, nourished, and supported. Here’s what I recommend if you want to tap into the same antiaging system that helped mice live 20% longer and thrive in old age:
1. Move your body, but don’t overdo it — Klotho increases with daily movement, especially moderate aerobic activity like walking, cycling, or light resistance training. But if you push too hard, it reverses the benefit. If you’re sedentary or struggling with energy, start with 20 to 30 minutes of brisk walking each day and build up to an hour daily from there. The goal is consistency, not exhaustion.
2. Eat like your life depends on it, because it does — Choose foods that nourish your cells. If you’re still eating low-carb, you’re working against klotho. Build your meals around whole foods like fresh fruit, root vegetables, fermented foods like raw grass fed yogurt or kefir, and minerals like copper and magnesium. I recommend whole-food carbs first, along with collagen-rich protein and tallow, ghee, or grass fed butter as your fats of choice.
3. Give your gut a reason to heal — Fermented foods like sauerkraut, kimchi, and kefir support gut integrity and encourage healthy klotho levels. If you’re dealing with digestive issues, don’t jump straight to fiber-heavy foods. Start with healing carbs like whole fruit and white rice, and slowly build up. Your gut flora is part of the communication loop that regulates your aging proteins.
4. Soak in sunshine and get your vitamin D naturally — Vitamin D directly triggers the klotho gene, so if you’re inside all day, you’re missing a key switch. Aim for regular daily sunlight with no sunscreen, but avoid exposure during peak hours (10 a.m. to 4 p.m.) until you’ve eliminated vegetable oils from your diet for at least six months.
The linoleic acid in vegetable oils makes your skin more susceptible to damage from the sun. If you’re vitamin D deficient or are unable to get regular sun exposure, use a vitamin D3 supplement, but always check that it’s balanced with magnesium and K2.
5. Stop doing things that age you faster — Smoking, loneliness, and chronic stress send klotho in the wrong direction. Start by building real social connections, creating a wind-down routine for sleep and learning to recognize the signals that your body needs rest, not stimulation.
FAQs About Klotho and Aging
Q: What is klotho, and why is it so important for aging?
A: Klotho is a protein your body makes naturally, mostly in your kidneys and brain. It helps protect against the effects of aging by reducing inflammation, supporting brain function, and preserving muscle and bone health.
Low klotho levels have been linked to shorter lifespans, memory loss and age-related disease. Research now shows it may act as a “longevity switch” that reflects how well your body is aging — more accurately than conventional disease markers.6
Q: Does boosting klotho actually extend your lifespan?
A: Yes, at least in animal studies so far. A 2025 study published in Molecular Therapy found that raising klotho levels in healthy mice extended their lifespan by 20%.7 But it didn’t just help them live longer. They stayed stronger, sharper, and showed fewer signs of age-related decline in muscle, bone, and brain function.
Q: How do I increase my klotho levels naturally?
A: Daily habits play a powerful role. Research in Metabolites shows moderate exercise, a whole-food diet rich in antioxidants, restful sleep, sunlight exposure for vitamin D, and emotional connection all raise klotho levels.8 On the flip side, stress, poor diet, smoking, and sleep issues cause levels to drop.
Q: Is klotho something to take as a supplement or drug?
A: No, klotho isn’t available as a pill or over-the-counter treatment. Current experiments use gene therapy to increase klotho production inside the body, but these methods are still in early stages and not approved for humans. For now, your best bet is creating the right conditions for your body to make more of it on its own.
Q: Could klotho be used as a routine health test someday?
A: Yes, since klotho levels drop with age and illness, scientists believe it could become a future biomarker, like blood pressure, to assess how well your body is aging. One review of 65 studies confirmed that klotho declines with chronic disease, especially in the brain, kidney, and metabolic systems. Tracking it could help predict disease risk and guide early intervention.9
Erythritol and Xylitol Raise Blood Clot and Stroke Risk
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/08/13/erythritol-xylitol-blood-clot-stroke-risk.aspx
Analysis by Dr. Joseph Mercola August 13, 2025

Story at-a-glance
- Research shows erythritol, a sugar substitute, weakens protective brain cell functions, increases oxidative stress, and compromises the blood-brain barrier integrity
- Erythritol consumption causes rapid platelet clumping and accelerated blood clot formation, dramatically increasing stroke and heart attack risks
- Like erythritol, xylitol increases platelet reactivity and clotting risks, with effects persisting for hours after consumption
- People diagnosed with diabetes, obesity, hypertension, or existing cardiovascular disease experience the most pronounced increases in clotting dangers
- Replace artificial sweeteners with whole fruits, root vegetables, and real carbs while avoiding omega-6 oils for better overall health
You’ve likely heard that sugar substitutes like erythritol are “healthy” sweetening alternatives, but research clearly shows otherwise. Emerging evidence shows that these ingredients compromise your cerebral vascular system, increasing your vulnerability to blood clots, stroke, and neurological damage.
Unfortunately, erythritol isn’t the only sugar alcohol implicated in serious health risks. Another similar sugar substitute, xylitol, has also been linked to increased cardiovascular events, including heart attacks and strokes.
Erythritol Damages Your Brain’s Blood Vessels Directly
In a study published in the Journal of Applied Physiology, researchers investigated what happens to your cardiovascular health when exposed to erythritol. Specifically, they used human brain microvascular endothelial cells, which line and protect your smallest brain blood vessels, to see if erythritol affected their ability to maintain a healthy blood-brain barrier.1
To perform the tests, the team exposed cultured endothelial cells to various concentrations of erythritol to mimic conditions similar to consuming erythritol-containing products. They found clear and consistent evidence of damage to these critical cells, even at low concentrations that match typical human consumption.
• Erythritol affects your brain blood vessels right away — After just a few hours of exposure, erythritol significantly weakened the cells’ protective functions and increased markers of oxidative stress, meaning the cells started becoming damaged.
• There was a substantial rise in reactive oxygen species (ROS) — These refer to unstable molecules that aggressively interact with and damage healthy cells and tissues. Normally, your body carefully manages ROS to prevent harm, but erythritol exposure has significantly disrupted this balance. Higher ROS levels directly translated to increased cell injury and inflammation, ultimately affecting your blood-brain barrier:2
“Uncontrolled increase in oxidative stress in cerebral endothelial cells can lead to disruption in the blood-brain barrier integrity, resulting in increased vascular permeability promoting tissue damage and death.”
• Erythritol affects endothelial cells’ nitric oxide (NO) balance — NO helps maintain vascular health by relaxing blood vessels and supporting proper blood flow. Yet, after erythritol treatment, the endothelial cells showed reduced production, coupled with increased markers indicating endothelial dysfunction — a condition that often precedes serious cardiovascular issues like strokes.
• Vascular blood flow is affected — According to the researchers, your endothelial cells release tissue-type plasminogen activator (t-PA) to maintain vascular flow, and erythritol affects this important function:3
“In the present study, erythritol impaired t-PA release in response to thrombin, indicative of reduced endothelial fibrinolytic capacity. Moreover, impaired capacity of brain microvascular endothelial cells to release t-PA is also associated with weakened blood-brain barrier integrity. Thus, erythritol-induced impairment in t-PA release may extend beyond compromised thrombolytic potential and contribute to greater cerebrovascular dysfunction.”
Erythritol Makes Your Blood Sticky
In an analysis published in Arteriosclerosis, Thrombosis, and Vascular Biology, researchers linked erythritol consumption to increased stickiness of your blood, drastically elevating your risk of forming harmful clots. Digging deeper into the methodology, the team aimed to measure how erythritol affects platelet function — the process responsible for your blood’s ability to clot — compared to regular sugar (glucose).4
Healthy participants were asked to drink a beverage containing either erythritol or glucose in separate sessions, allowing researchers to observe real-time effects on blood clotting. Immediately following consumption, their platelet activity was tracked through blood tests and specialized laboratory measurements.
• Platelet reactivity surged significantly within minutes — Erythritol made the platelets rapidly prone to clumping together. This accelerates clotting, setting the stage for serious health events such as strokes or heart attacks, especially in individuals already facing cardiovascular risks. In fact, the researchers noted that erythritol caused a “>1000-fold increase in erythritol plasma concentration.”5
In laboratory tests designed to mimic clot formation in your blood vessels, clots not only formed faster but were also structurally more robust, increasing the likelihood of dangerous blockages occurring in crucial arteries supplying your heart or brain.
• Erythritol vs. glucose — Glucose did not trigger similar platelet activation or clotting changes. The stark contrast highlights that erythritol uniquely and acutely endangers your vascular health, whereas glucose remains safer to use in this context.
•Thrombin generation was accelerated — This enzyme essentially acts as a catalyst, rapidly converting fibrinogen — a soluble protein circulating in your blood — into fibrin, the insoluble threads that physically form the clot.
Increased thrombin generation means more rapid and intense clot formation, creating the dangerous possibility of vessel blockage and impaired blood flow to critical organs.
• Erythritol amplified the release of dense granules — These are tiny packets of substances that help platelets stick together and form stable clots. When erythritol exposure triggers platelets, these granules quickly discharge their contents, dramatically boosting platelet aggregation and clot robustness. This intensifies the clot formation process even further, magnifying the threat to your cardiovascular system and raising your risk of stroke or heart attack.

Save This Article for Later – Get the PDF Now
Another Alcohol Sugar Is Linked to Heart Problems
A study published in the European Heart Journal explored the cardiovascular risks associated with consuming xylitol, another popular sugar substitute that is categorized as “Generally Recognized as Safe” (GRAS).6 Researchers tested how regular consumption of xylitol affects blood clotting and cardiovascular health, specifically by assessing the sweetener’s impact on platelet activity and risk of forming blood clots.7
By comparing participants who regularly consumed xylitol-containing foods with those who did not, the researchers identified significant increases in cardiovascular risks among the xylitol users. Specifically, individuals consuming xylitol regularly showed markedly elevated platelet reactivity, meaning their blood became noticeably stickier similar to erythritol.
• There was a measurable rise in cardiovascular incidents — This includes heart attacks and strokes, among individuals with high xylitol consumption. According to the data, these health events correlated strongly with elevated levels of xylitol detected in participants’ blood. In other words, the more xylitol present in your bloodstream, the higher your chances of experiencing an adverse cardiovascular event.
• Even moderate, frequent consumption of xylitol significantly heightened platelet activity — Tests conducted on blood samples demonstrated that xylitol directly triggered an increase in platelet aggregation, ultimately forming clots. Moreover, the researchers emphasized that it happened to all participants:8
“[C]onsumption of a xylitol-sweetened drink markedly raised plasma levels and enhanced multiple functional measures of platelet responsiveness in all subjects.”
• The effects of xylitol linger — The study highlighted a troubling time-related finding — platelet activation occurred quickly after xylitol consumption and persisted for several hours. Participants who consumed even modest amounts of xylitol-containing foods experienced a rapid increase in platelet aggregation within minutes.
• Groups who are vulnerable to xylitol’s harmful effects — The researchers observed that individuals already predisposed to cardiovascular disease — such as those with insulin resistance, diabetes, obesity, or hypertension — experienced the most pronounced increase in clotting risk after consuming xylitol. Simply put, if you’re already managing a heart-related condition, consuming xylitol will significantly raise your risk of a heart attack or stroke.
• Platelet activity also surges — When comparing xylitol’s effects on platelets with other sugar alcohols, the researchers found similar but distinct patterns. Like erythritol, xylitol increased clotting risks and even increased platelet activity to concerning levels:9
“[W]e found xylitol, like erythritol, is readily absorbed following oral ingestion by humans, with plasma levels increasing over 1000-fold in the post-prandial setting.”
• Xylitol causes changes in platelet calcium signaling pathways — Under normal conditions, calcium within platelets is tightly controlled. However, exposure to xylitol disrupted these delicate calcium balances, causing platelets to release chemicals rapidly that stimulate clumping and clot formation. This mechanism closely mirrors what researchers observed with erythritol, underscoring a shared risk profile among sugar alcohols.
Overall, these detailed findings offer strong evidence that xylitol — despite its innocent marketing as a healthier sugar alternative — poses genuine and significant cardiovascular dangers.
Avoid Artificial Sweeteners and Consume Real Carbohydrates
If you’re concerned about protecting yourself from blood clots, strokes, or heart disease, the first step is to address your diet by eliminating harmful sugar substitutes like erythritol and xylitol. As noted by the published research, these sweeteners make your blood dangerously sticky and damage the blood vessels that safeguard your brain and heart. To help you get started, here are my recommendations:
1. Cut artificial sweeteners completely — Stop consuming erythritol, xylitol, and other products that contain sugar alcohols right away. Even if they’re labeled “natural,” these sweeteners increase clotting risks and cause harmful inflammation in your blood vessels. Check labels carefully, especially in products marketed as “sugar-free,” and avoid items that contain these ingredients. In the same way, avoid products that use artificial sweeteners, such as aspartame and sucralose.
2. Consider these other sugar substitutes — If you get cravings for sweet food, consider making them at home using healthy alternatives. I recommend natural stevia (the plant itself), as well as Luo Han Guo. Pure dextrose, if it’s derived from clean cane sugar, is a third alternative I recommend.
3. Choose natural carbohydrates instead — Your body thrives on real carbohydrates for energy. Fruit juices with pulp or whole fruits like oranges, apples, and berries are great choices. Root vegetables such as sweet potatoes also offer safe sources of carbohydrates that support your metabolic health without harmful additives.
Aim for 200 to 250 grams of healthy carbohydrates daily to maintain stable insulin levels and improve overall metabolic health. White rice and ripe bananas are also good dietary sources of carbohydrates.
4. Focus on healing your gut microbiome — Gut health is deeply connected to your overall health, including your cardiovascular system. And, as noted in previous articles, artificial sweeteners greatly affect your gut microbiome diversity.
A healthy gut helps maintain balanced inflammation and reduces your overall risk of clotting and cardiovascular problems. That said, I recommend you eat fermented foods regularly such as homemade yogurt, sauerkraut, and kimchi to reseed your gut with healthy bacteria.
5. Lower your exposure to omega-6 fatty acids — If you’ve been eating foods high in alcohol sugars, you’re likely eating other foods that contain linoleic acid (LA), which I believe is one of the most pernicious toxins in the Western food supply.
High intake of LA from vegetable oils (like sunflower, soybean, and canola oils) severely damages your blood vessels and increases inflammation and clotting risk. Choose traditional, safer fats like raw butter from grass fed cows, tallow, or ghee to cook your food at home.
In addition, LA exists in the many foods you eat — even meat. I recommend you maintain your LA intake below 5 grams per day to protect your health. If you can keep it below 2 grams per day, that’s even better. To help you track how much LA you’re eating, I recommend downloading the Mercola Health Coach app when it launches later this year. It will feature the Seed Oil Sleuth tool, which calculates your LA intake down to a tenth of a gram.
Frequently Asked Questions (FAQs) About Alcohol Sugars
Q: What happens to my brain when I consume erythritol?
A: Erythritol damages the tiny blood vessels in your brain by weakening the blood-brain barrier. This allows harmful substances to leak into your brain tissue, triggering inflammation and increasing your risk of stroke and neurological damage. It also disrupts nitric oxide (NO) production, which is key for proper blood flow.
Q: How fast does erythritol affect my blood?
A: The effects are immediate. Within minutes of drinking something with erythritol, your blood becomes more sticky. This means your platelets — the cells that form clots — become highly reactive, making it easier for dangerous clots to form. These changes persist for hours, elevating your stroke and heart attack risk.
Q: Is glucose safer than erythritol or xylitol?
A: Yes. In the clinical studies, glucose did not trigger the same clotting or vascular damage that erythritol and xylitol did. In fact, researchers found that erythritol caused over a thousandfold spike in plasma levels after just one drink, something that did not happen with glucose. If you’re going to use glucose, make sure it comes from pure cane sugar.
Q: Does xylitol cause the same issues as erythritol?
A: Yes. Xylitol increases platelet activity just like erythritol and raises the risk of cardiovascular events, including heart attacks and strokes. Research showed that even moderate use made blood stickier and that the clotting effects lingered for hours. People with insulin resistance, obesity, or high blood pressure are at even greater risk.
Q: What can I do to protect myself?
A: Cut sugar alcohol from your diet, especially products that have erythritol and xylitol. Instead, use real carbohydrates like whole fruits and root vegetables. Avoid vegetable oils as well, which worsen vascular inflammation, and aim for 200 to 250 grams of quality carbs daily.
How a Woman’s Diet Directly Shapes Her Vaginal Microbiome
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/08/09/diet-vaginal-microbiome.aspx
Analysis by Dr. Joseph Mercola August 09, 2025

Story at-a-glance
- A woman’s vaginal microbiome is shaped by what she eats daily — choosing whole foods over processed ones gives more control over infections, irritation, and long-term health
- Eating more processed meats and drinking alcohol increases harmful vaginal bacteria like Gardnerella, raising the risk for infections, odor, irritation, and pregnancy complications
- Research shows that omega-3 fat alpha-linolenic acid (ALA) supports beneficial bacteria strains that help keep vaginal pH low and defend against bacterial overgrowth and inflammation
- Carbohydrates are crucial during pregnancy — getting over 49% of calories from healthy carbs promotes a balanced vaginal microbiome and lowers the risk of dysbiosis
- Excess linoleic acid (LA) from seed oils like soybean, corn, and sunflower disrupts bacterial balance and promotes inflammation, undermining vaginal and gut health
Many women today deal with recurring vaginal infections, yeast overgrowth, or just a general feeling of discomfort down there. While it may seem like an issue related to hygiene, there’s a chance that the problem goes much deeper — and that diet likely plays a role.
Most women have no idea that their daily food choices are shaping their vaginal health. Yet research now shows that what a woman eats directly influences which bacteria thrive — and which don’t — inside her body. The good news is that this is something that can be controlled. By making certain dietary changes, it’s possible to bring back balance to the vaginal microbiome.
Researchers Studied the Link Between Vaginal Microbiome Patterns and Food Intake
A recent study conducted by researchers in Italy examined how macronutrients in the diet affect the bacterial makeup of the vaginal microbiome. Published in Frontiers in Cellular and Infection Microbiology, the research team investigated which dietary patterns support a protective bacterial environment and which ones led to vaginal dysbiosis (microbial imbalance).1
• Study participants were mostly young women — The cross-sectional study involved 113 sexually active women between the ages of 19 and 30, with a median age of 21 years. All were in good health and free from chronic disease, infections, or pregnancy.
• The participants provided two self-collected vaginal samples — These were taken during the late follicular phase (the final stage in the menstrual cycle). One sample was tested for sexually transmitted infections (STIs) and the other was used for metabolomic analysis and microbiota profiling.
• The vaginal bacteria were grouped into different categories — These categories show which types of bacteria are most dominant. The team also identified the different types of Lactobacillus, a strain known to help protect vaginal health.
• The researchers also evaluated the participants’ food intake — They used a food questionnaire with 188 food items classified into 24 categories. The dietary data included how much alcohol, protein, fiber, and carbohydrates each woman regularly consumed.
“Nutritional data were processed and analyzed for alcohol, energy, and macronutrient intake, and macronutrient balances were examined using Compositional Data Analysis (CoDA), employing additive log-ratio transformations,” News-Medical.net explains.
“Statistical analyses included correlation studies, diversity indices, and multinomial logistic regression adjusted for potential confounders such as stress, contraceptive use, age, and body mass index (BMI).”2
Eating More Plants and Fewer Processed Meats Changes the Vaginal Microbiome
One of the most important findings was how excessive protein intake along with alcohol consumption significantly led to an imbalance in the vaginal microbiome, allowing harmful bacteria to thrive.
• A high intake of animal protein and alcohol was associated with high amounts of harmful bacteria — In women whose diets were rich in meat and alcohol, the bacterial communities shifted into CST IV, meaning they have more anaerobic bacteria and fewer healthy Lactobacillus species.
• In particular, Gardnerella and Prevotella strains are prevalent in these participants’ vaginal microbiome — These two microbes are the main culprits behind bacterial vaginosis (BV), a condition marked by abnormal discharge, odor, irritation, and increased risk of sexually transmitted infections and pregnancy complications.
• These dysbiotic communities were linked to increased glucose and simple sugar metabolites — These conditions favor the growth of unwanted bacteria. These microbial groups also had more diverse species present, which may sound good, but in the vaginal environment, more diversity usually signals an imbalance. A healthy vaginal microbiome is one where just a few dominant good bacteria keep the ecosystem stable and defend against invaders.
• Meanwhile, consuming more vegetables, fiber, and healthy carbohydrates led to more favorable microbiome profiles — Specifically, those with higher intake of these nutrients had more beneficial Lactobacillus strains, which are protective for vaginal health, helping lower infection risk.
• Bacterial balance wasn’t just about which microbes were present — It also came down to the chemical compounds those microbes were producing. In healthy vaginal environments dominated by Lactobacillus strains, researchers found higher levels of branched-chain amino acids like leucine and isoleucine, and antioxidants that support local immune defenses and help keep vaginal pH low, preventing the overgrowth of BV-causing bacteria.
• These results support the idea of a “vagina-gut axis” — This is a two-way street where dietary nutrients modulate not just the digestive system but reproductive health as well. The researchers concluded:
“A healthy diet could preserve the vaginal homeostasis by regulating the trafficking of bacterial species across the vagina and gut (bacterial translocation), in turn modulating the level and type of metabolites produced by the microbiota, acting as indirect players of the vagina-gut axis.
In conclusion, we highlighted that specific dietary habits (i.e., reduced consumption of alcohol and animal proteins, higher intake of linolenic acid) can have a beneficial impact on the vaginal environment, through the maintenance of a microbiota mostly dominated by ‘protective’ Lactobacillus species …”3

Save This Article for Later – Get the PDF Now
Plant-Based Omega-3s Led to Favorable Microbiome Profiles, but There’s a Catch
One of the key beneficial nutrients highlighted by the study was alpha-linolenic acid (ALA). Researchers suggest this plant-based omega-3 may actually interact with vaginal bacteria, possibly converting into other helpful fatty acids that nourish Lactobacillus species directly.4
While I do acknowledge the advantages of ALA shown by this study, I believe that animal-derived omega-3 fats, specifically docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), are far more superior for overall health, for two reasons:
• EPA and DHA surpass ALA in terms of their bioavailability — To put it simply, the body uses these two animal-based omega-3s more easily, making their benefits more easily attainable.
• Plant sources of ALA are also loaded with polyunsaturated fats (PUFs) — Most of the foods high in ALA — nuts, seeds, flaxseeds, and chia seeds — also contain high amounts of linoleic acid (LA), a PUF that disrupts the mitochondria and increases inflammation. Hence, excessively consuming these foods could be causing more damage to your health.
In fact, the featured study made a reference to research on how women’s dietary intake of omega-3s reduces bad bacteria, while supporting the growth of beneficial strains that protect against intestinal inflammation and infections. In the study, DHA and EPA were specifically found to exert these benefits.5
That said, too much omega-3 is just as problematic as too little — after all, they are also a type of PUF. The key is that if you’re raising your omega-3 intake, it is absolutely crucial to lower your LA intake from seed oils and processed foods (especially for women who are pregnant or planning to conceive). Getting too much omega-3s from certain supplements is also not advisable — read more about it in this article, “The Omega-3 Paradox — How Much Is Too Much?”
A Healthier Vaginal Microbiome During Pregnancy Starts with the Right Carbs
Maintaining a balanced vaginal microbiome is essential at every stage of life, but it becomes imperative during pregnancy. Earlier research published in Nutrients looked at how diet quality influences the vaginal microbiome throughout pregnancy.6
• The study followed a group of 40 women during all three trimesters — Both their dietary habits and the bacteria living in their vaginal tract were closely monitored during this time. The participants, who came from different ethnic backgrounds and were between 18 and 45 years old, were all considered low-risk pregnancies.
Each woman completed food questionnaires in the first, second, and third trimesters, while also self-collecting vaginal samples for microbiome analysis. The goal was to determine if better eating habits were linked to a healthier vaginal environment, which could reduce the risk of complications like preterm birth and bacterial infections.
• What the researchers found was eye-opening — Diet quality had a consistent and measurable impact on which bacteria showed up in each woman’s microbiome. Women who scored higher on the Healthy Eating Index (HEI) — a tool that measures how closely their diets align with recommended dietary guidelines — were more likely to have protective bacteria strains.
• The biggest dietary driver of this beneficial balance was carbohydrate intake — Women who got more than 49% of their daily calories from carbohydrates had a microbiome dominated by good bacteria, while those who ate fewer carbs showed a rise in less favorable species and anaerobic bacteria that are linked to vaginal dysbiosis, which raises the risk for infection, inflammation, and complications during labor.
• Timing made a difference, too — In early pregnancy, better diet scores were associated with fewer overall bacterial species, which is a good thing in the vaginal ecosystem. Unlike the gut, where diversity is usually beneficial, the vaginal microbiome works best when just a few dominant good species hold their ground. This low-diversity, Lactobacillus-rich environment is what keeps things balanced and prevents harmful bacteria from taking over.
• The biological mechanisms at play here come down to something simple but powerful — glycogen — When a woman eats enough carbohydrates, her vaginal cells store glycogen, a starch-like compound that acts as food for beneficial Lactobacillus species. These bacteria convert glycogen into lactic acid, which keeps vaginal pH low and stops pathogens in their tracks. Without enough glycogen, the vaginal microbiome becomes imbalanced.
• Hormonal shifts also play a role — Estrogen, which rises steadily throughout pregnancy, helps the body build and store glycogen in vaginal tissue. However, not getting enough carbs means it can’t do its job effectively. That’s why what women eat matters just as much as what their hormones are doing.
Interestingly, even among women with similar body weights or ethnic backgrounds, the quality of their diet still made a difference in microbial outcomes. This means dietary improvements will help almost anyone, regardless of other risk factors.
The Type of Carb Matters
Remember that there’s a world of difference between carbs that nourish the cells and carbs that accelerate inflammation and decline. It’s important to consume high-quality carbohydrates from real, whole foods, and not refined carbs that harm the gut and vaginal microbiome. Aim for 200 to 250 grams of the right carbs per day.
• Carbs from ultraprocessed foods damage health — Avoid carb choices that come in a box, bag, or bar with a long list of hard-to-pronounce ingredients. Refined carbs, like white bread, cookies, breakfast cereals, store-bought baked goods, and granola bars, spike blood sugar, damage both the gut and vaginal microbiome.
• Optimize gut health before consuming complex carbs — Symptoms like bloating, food intolerances, or loose stools, indicate that a compromised gut, and consuming complex carbs will only feed the bad bacteria. The key is to heal the gut first — stick to easy-to-digest carbs like white rice and whole fruit to fuel the body without overfeeding the bad microbes.
• Reintroduce fermentable fibers once the gut is healed — If the symptoms are gone, consider adding in small amounts of fibers that feed the good gut bacteria. Start with cooked and cooled white potatoes or green bananas, which contain resistant starch.
More Strategies to Support the Vaginal Microbiome
If you’re a woman who’s dealing with frequent vaginal infections, irritation, or discomfort, or if you simply want to support a healthy microbiome during pregnancy, your first step is to address the root cause — your diet. What you eat affects your body’s internal ecosystem, especially the balance of bacteria in the vaginal tract.
The right type of macronutrients will either support protective bacteria or feed the ones that lead to imbalance and infection. In addition to consuming the right carbs and getting omega-3s, here are some changes that will help the vaginal microbiome.
1. Eliminate linoleic acid (LA) from your diet — This omega-6 fat promotes inflammation and has been linked to microbial imbalance in the body. If you’re using seed oils like soybean, corn, sunflower, or safflower oil in your cooking or eating a lot of processed foods that contain them, you’re likely getting too much LA.
Replace these oils with healthier fats like grass fed butter, tallow, or ghee. If you often snack on chips or eat out often, cutting back on fried and processed foods will help reset your inflammatory load and support a healthier microbiome.
2. Avoid eating processed meats — As noted by the featured study, eating more processed meats like bacon or deli meat allows harmful bacteria to thrive, which leads to bacterial vaginosis. I recommend getting your protein from whole food sources like pasture-raised eggs, raw dairy, grass fed beef, and wild-caught fish.
3. Skip the alcohol — Even having a few cocktails a few times a week can affect the vaginal ecosystem. Both featured studies linked alcohol intake with increases in bad bacteria tied to BV and increased vaginal pH. Cutting back or eliminating alcohol completely could be one of the fastest ways to reset the balance and prevent unpleasant vaginal conditions.
4. Avoid douching — Despite what is shown in many advertisements, douching is not a healthy, recommended practice. Flushing the vagina with water or another cleansing agent only serves to disrupt its healthy bacteria balance, giving bad bacteria the advantage. According to the U.S. Department of Health and Human Services’ (HHS) Office of Women’s Health:7
“Douching can change the necessary balance of vaginal flora (bacteria that live in the vagina) and natural acidity in a healthy vagina. A healthy vagina has [both] good and harmful bacteria. The balance of bacteria helps maintain an acidic environment. The acidic environment protects the vagina from infections or irritation.
Douching can cause an overgrowth of harmful bacteria. This can lead to a yeast infection or bacterial vaginosis. If you already have a vaginal infection, douching can push the [infection-causing] bacteria up into the uterus, fallopian tubes and ovaries. This can lead to pelvic inflammatory disease, a serious health problem. Douching is also linked to other health problems.”
Frequently Asked Questions (FAQs) About Diet and the Vaginal Microbiome
Q: How does a woman’s diet affect her vaginal health?
A: Daily food choices directly influence the types of bacteria that grow in the vaginal microbiome. Diets high in processed meat, alcohol, and seed oils support harmful bacteria, while whole foods like vegetables, fiber, and healthy carbs promote protective Lactobacillus species that prevent infections and irritation.
Q: What is the role of linoleic acid in disrupting vaginal health?
A: Linoleic acid, found in seed oils like soybean, corn, sunflower, and safflower, promotes inflammation and microbial imbalance. Too much of it fuels harmful bacteria, increasing the risk of vaginal infections and irritation.
Q: What foods or habits should women avoid to prevent imbalance in their vaginal flora?
A: Avoid alcohol, processed meats, and seed oils high in linoleic acid. These promote harmful bacteria and inflammation, leading to discomfort, bacterial vaginosis, and higher infection risk.
Q: Why are carbohydrates especially important during pregnancy?
A: Carbs help the body store glycogen in vaginal tissue, which feeds beneficial bacteria. Pregnant women with higher carb intake (over 49% of calories) had healthier microbiome profiles and lower risk of complications like preterm birth.
Q: Is more bacterial diversity always better?
A: Not in the vaginal microbiome. Unlike your gut, a healthy vaginal environment actually thrives with fewer, dominant good bacteria. High diversity here often means imbalance, especially when harmful species start to outnumber the protective ones.
Linoleic Acid, Mitochondria, Gut Microbiome, and Metabolic Health — A Mechanistic Review
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/21/linoleic-acid-mitochondrial-damage-metabolic-health.aspx
Analysis by Dr. Joseph Mercola July 21, 2025

Story at-a-glance
- Linoleic acid (LA), a fat found in vegetable oils, accumulates in your tissues and disrupts mitochondrial function, which drains your energy and slows your metabolism
- This fat becomes toxic when oxidized, producing harmful byproducts that damage DNA, enzymes, and the machinery your cells need to generate energy
- Excess LA damages your gut by interfering with colon cell metabolism, harming beneficial microbes, and promoting inflammation linked to insulin resistance and obesity
- LA’s half-life in body fat is about two years, meaning the damage builds up slowly and requires long-term dietary changes to reverse
- Cutting out vegetable oils, eating gut-repairing whole foods, and switching to stable fats like grass fed butter and tallow are key steps to restoring your metabolic health
A century ago, linoleic acid (LA) wasn’t a major part of the human diet. Today, it dominates. Hidden in nearly every processed food and most restaurant meals, this polyunsaturated fat — found in vegetable oils like soybean, corn, and canola — has quietly become the most consumed fat in the modern world.
You’ve likely been told it’s healthy, even essential. But the truth is, LA behaves very differently inside your body than other fats. Unlike saturated fats, it’s chemically unstable. It breaks down easily, especially when exposed to heat, light, or oxygen — turning into toxic byproducts that your body struggles to clear. And unlike fats your body uses for energy, this one gets stored in your tissues and builds up over time, where it quietly interferes with energy production, gut health, and hormone regulation.
If you’ve been dealing with low energy, unexplained weight gain, or insulin resistance, there’s a good chance this hidden ingredient is working against you. Most people don’t realize that the foods they’ve been told are heart-healthy, like certain oils, nuts and packaged snacks, are loading their cells with something they weren’t designed to handle in such high amounts.
In my mechanistic review, published in Advances in Redox Research, I broke down exactly how LA disrupts your mitochondria — the energy engines inside every one of your cells.1 What the research revealed changed how I look at metabolic disease entirely.

Too Much LA Throws Your Metabolism Into Chaos

My paper looks closely at how high intake of LA disrupts mitochondrial function, damages gut balance, and triggers insulin resistance.2 It’s a mechanistic review, meaning it synthesizes a wide range of cellular, biochemical, and metabolic evidence to show exactly how LA breaks energy production inside your cells.
The figure above shows how your mitochondria get thrown off balance when making energy. When there’s too much fuel coming in, it overloads your system and causes a backup at key points called Complex I and II. This leads to reductive stress, where electrons leak out and create harmful byproducts like reactive oxygen species (ROS).
On the flip side, if the system is damaged or can’t keep up, “oxidative stress” occurs, also producing harmful waste. Both situations disrupt energy flow and increase the risk of cell damage. The figure highlights the importance of keeping this process in balance for healthy energy production and overall cellular function.
• LA does damage in two directions at once — I detailed how LA creates both oxidative and reductive stress. Oxidative stress is when your body produces too many free radicals. Reductive stress, by contrast, is when your cells build up too many unused electrons because the mitochondria can’t process them fast enough. This combination wrecks the redox balance that your body depends on to generate clean, efficient energy.
• The damage starts at the mitochondria — your body’s energy centers — LA embeds itself into a special fat called cardiolipin, found in the inner membrane of your mitochondria. Cardiolipin holds energy-generating protein complexes together, kind of like scaffolding. But LA is chemically unstable and easily oxidized.
Once inside cardiolipin, it sets off chain reactions that weaken mitochondrial structure, unravel protein complexes, and reduce adenosine triphosphate (ATP) output — your body’s core energy currency.
• Reductive stress quietly sabotages your energy long before symptoms appear — When your diet contains too much LA — from fried foods, processed snacks, salad dressings, and even “healthy” nuts, pork and chicken — it leads to constant overloading of the mitochondria with electrons.
The problem is that the mitochondrial transport chain can’t keep up. Electrons back up and spill over, generating ROS and worsening oxidative damage. This imbalance is a hidden engine behind fatigue, weight gain, and poor metabolic flexibility.
Why Macronutrient Balance Matters for Redox Health

The figure above illustrates how the balance of protein, carbs, and fat in your diet help protect your mitochondria from the kind of energy overload LA creates. The example in the figure uses a common ratio — about 15% protein, 55% carbs, and 30% fat — to demonstrate how a balanced mix of macronutrients keeps your metabolism running smoothly.
• Carbs and fats take different pathways to get broken down for energy, but both eventually fuel your mitochondria — As they’re processed, they generate molecules that feed electrons into your mitochondria to make ATP. If you eat too much of any one macronutrient — especially fat — it overwhelms the system. Your mitochondria can’t process the excess electrons fast enough, creating a traffic jam that leads to reductive stress and oxidative damage.
• When your diet is more balanced, energy flows through your mitochondria in a steadier way — This reduces the risk of cellular stress and improves metabolic flexibility. This helps explain why even high-fat diets marketed as “healthy” backfire if they’re rich in unstable fats like LA — they push your mitochondria past their limit.
• LA doesn’t just sit in your tissues — it poisons your energy over time — Unlike other fats that your body burns or clears quickly, LA sticks around. It builds up in your fat stores and stays there for years, literally. As noted in my review, the half-life of LA in body fat is estimated to be two years. That means every meal high in LA adds to a long-term problem that your body can’t easily reverse.
• LA pushes your system into dysfunction — While LA is essential in small amounts, excessive intake, over time, floods your mitochondria with reactive molecules. When the supply of electrons from fat breakdown exceeds the mitochondria’s capacity to use them, your energy system crashes from the inside out. The result is poor glucose handling, inflammation, and insulin resistance — what many people chalk up to aging, but is actually preventable damage.

Save This Article for Later – Get the PDF Now
Your Mitochondria Need These Nutrients to Run

The table above shows the essential nutrients your mitochondria need to turn food into usable energy. These include key B vitamins like niacinamide (B3), thiamine (B1), and riboflavin (B2), which act like spark plugs in your cellular engine. They help fuel the chain of reactions that powers ATP production.
• It also includes CoQ10, a compound your body makes but needs more of as you age or if you take statin drugs — CoQ10 helps shuttle electrons inside your mitochondria and reduces oxidative stress.
• Magnesium plays a starring role too — Magnesium helps stabilize ATP and supports hundreds of enzymes involved in metabolism and insulin sensitivity.
• The nutrient amounts listed in the table are general estimates — Your specific needs depend on your diet, health history, and how much stress your system is under. Making sure you get enough of these cofactors helps restore mitochondrial balance and improves how your body handles energy.
Cardiolipin — Your Energy Stabilizer — Gets Hijacked by LA

Cardiolipin isn’t just any fat. It’s unique in structure and key for keeping your mitochondria’s inner membrane stable.
The figure above shows where cardiolipin lives inside your mitochondria and why it matters for energy production. On the left, you see a simplified diagram of a mitochondrion, highlighting its key parts: the outer membrane, inner membrane, the folds called cristae, and the inner space known as the matrix. In the center, the zoomed-in view of the inner membrane points out spots rich in cardiolipin (marked in magenta), especially around the curved edges of the cristae.
These areas help keep the mitochondrial folds stable and support the formation of energy-producing protein clusters. On the right, the figure compares a typical fat molecule with cardiolipin. Unlike regular fats that have two tails, cardiolipin has four, giving it unique properties that help hold proteins in place, keep the membrane flexible, and power essential energy processes. This figure helps explain why cardiolipin is so important for keeping your mitochondria — and your cells — running smoothly.
My review shows how LA infiltrates cardiolipin and makes it highly vulnerable to oxidation. Once oxidized, cardiolipin can’t hold the mitochondrial protein complexes together anymore. This instability ruins the structure needed for ATP production and accelerates cellular aging.
• This process explains why many “healthy” high-fat diets fail over time — While keto or very low-carb diets often seem to work at first by lowering blood sugar, the LA-rich fats they rely on overload your cell “engines.” Breaking down these fats floods your mitochondria with more fuel molecules than they can handle, clogging the energy-production system, slowing ATP creation, and ramping up internal wear-and-tear.

• Once LA oxidizes, it turns into something far more dangerous — The figure above shows how eating too much LA sets off a chain reaction that damages your mitochondria and drains your energy. When you eat a lot of LA, it gets built into the inner membrane of your mitochondria, the part of your cells that makes energy. But LA is fragile. Under stress — especially when your mitochondria are overloaded and energy flow backs up — LA starts to oxidize.
When LA breaks down inside your body, it doesn’t just disappear — it turns into harmful byproducts. One of the worst is called 4-HNE, a sticky, reactive compound that latches onto important parts of your cells like enzymes, DNA, and the machinery inside your mitochondria. Think of it like grease gumming up an engine. It clogs the system that helps your cells make energy. Over time, this damage builds up, draining your energy and stressing your cells even more.
Your Gut Suffers Too, Starting with Your Colon Cells
The figure above shows what happens when your gut microbiome is in balance — and what happens when it’s not. On the left, you see a healthy gut filled with diverse, friendly bacteria that break down fiber into short-chain fatty acids (SCFAs) like butyrate. These compounds feed the cells lining your colon, strengthen your gut barrier, reduce inflammation, and support better blood sugar control. This is how fiber is supposed to work when your gut is healthy.
• LA triggers a cascade that increases inflammation from your gut outward — The right side of the figure tells a different story — one that starts with too much LA in your diet. LA interferes with the ability of colon cells to burn butyrate for fuel, which leaves more oxygen in your gut.
That extra oxygen disrupts the environment, harming helpful bacteria and allowing harmful ones to take over — a condition called dysbiosis. In this inflamed state, the same fiber that normally helps you actually makes things worse by fueling the wrong microbes.
• As dysbiosis deepens, harmful bacteria flourish — They produce toxic byproducts like lipopolysaccharide (LPS), which break through your gut lining and enter your bloodstream. This triggers your immune system, leading to chronic, low-grade inflammation.
Over time, this inflammatory cascade makes insulin resistance worse and raises your risk for problems like fatty liver, obesity, and diabetes. This is known as the fiber paradox — where fiber’s benefits depend entirely on the state of your microbiome.
Insulin Resistance Becomes Inevitable When LA Is High
The table above shows the main tools used to measure insulin resistance and check how well your cells are managing their internal energy chemistry, known as redox balance. One common method is HOMA-IR, a calculation based on fasting insulin and glucose levels that gives a rough idea of how sensitive your cells are to insulin. While it’s convenient for everyday use, it’s not as precise as the gold-standard glucose clamp test, which measures exactly how well your body clears sugar under controlled conditions.
• The table also lists blood markers that reflect how your mitochondria are handling energy — These include ratios like lactate to pyruvate and others that show the balance between NAD⁺ and NADH — a key part of your cell’s energy-making process. When this balance is off, it signals redox stress and early signs of metabolic trouble.
• This is where LA comes in — When your diet is high in LA, it disrupts how your mitochondria produce energy. As that process breaks down, your cells stop responding to insulin the way they should. Your pancreas makes more insulin to compensate, but that only makes things worse. Blood sugar rises, fat starts to build up, and your cells become more inflamed and energy-starved — a downward spiral triggered by too much LA.
Cutting Out LA Helps Restore Your Mitochondria

For more details on the risks of excessive LA intake, read the simplified version of my review. If your energy’s been crashing, your metabolism feels stuck, or your gut hasn’t been right in years, there’s a good chance vegetable oils are part of the problem. You don’t need a lab test to confirm it — just look at what’s in your pantry or what you’ve been eating out.
Getting rid of the LA that’s buried in so many processed foods is the first and most important step to undoing the metabolic damage and giving your cells a chance to function normally again. Here’s what I recommend you do to take back control:
1. Ditch vegetable oils completely — The most direct way to reverse mitochondrial dysfunction is to stop the flood of LA coming in every day. That means eliminating all vegetable oils like soybean, corn, sunflower, safflower, cottonseed, grapeseed, canola, rice bran and peanut oil.
These are hiding in nearly every processed food, packaged snack, and restaurant meal, especially fried foods and dressings. Start reading labels, cook at home more, and treat every elimination as an investment in your energy.
2. Switch to safe fats that don’t damage your mitochondria — Your body needs fat to function — you just need the right kind. Replace those unstable omega-6 fats with stable, saturated fats like grass fed butter, ghee, beef tallow and coconut oil. These fats resist oxidation, don’t overload your mitochondria with electrons, and help restore proper redox balance inside your cells. I use them regularly because they support energy, hormones, and brain health without contributing to inflammation.
3. Eat more foods that repair your gut and feed your colon cells — If your gut’s been compromised by LA, you’ll want to focus on foods that restore the oxygen balance in your colon and support butyrate production. High-quality carbs like sweet potatoes, carrots, squash, and rice are rich in fermentable fibers that fuel this process. But here’s the catch: as mentioned, if your gut is already damaged, throwing in lots of fiber too soon will make symptoms worse. That’s the fiber paradox.
If you’re struggling with bloating, cramping, constipation or loose stools, start by healing your gut first — then introduce fiber-rich foods slowly, in small amounts. Once tolerated, these fibers help reinforce your gut lining, lower inflammation, and recalibrate your immune system. You’ll feel the difference in everything from digestion to energy and mood.
4. Cut back on olive oil, nuts and seeds — even the so-called healthy ones — Nuts and seeds are often seen as health foods, but many, like walnuts, almonds, pecans, sunflower, and pumpkin seeds — are loaded with LA. Even macadamia nuts and olive oil, while lower in LA, are rich in monounsaturated fats that oxidize easily under heat or light.
That oxidation stresses your mitochondria and disrupts energy production. Olive oil is also commonly adulterated with cheaper vegetable oils. If you snack on nut butters or drizzle olive oil over everything, it’s time to rethink those habits.
5. Stay consistent, because LA takes years to clear — This isn’t something you fix in a week. Since LA has a half-life of about two years, it means the fats stored in your tissues now will still affect your mitochondria years from today. But every LA-free meal you eat moves you forward.
Every time you say no to fried foods, chips, or commercial salad dressing, you’re giving your cells a break and slowly offloading the oxidative burden. Think of this like a slow, steady cleanup — each step compounds and helps rebuild your metabolism from the inside out.
FAQs About Linoleic Acid
Q: Why is LA considered harmful if it’s labeled as “heart-healthy”?
A: While LA is essential in small amounts, modern diets overload your body with it, mainly from vegetable oils. In excess, LA embeds itself in your mitochondria, oxidizes, and creates toxic byproducts that damage energy production, promote inflammation, and drive insulin resistance.
Q: What are the signs that LA is damaging my metabolism?
A: If you experience chronic fatigue, weight gain, blood sugar issues, gut problems, or difficulty losing fat despite a healthy diet, LA could be a hidden factor. It accumulates in your fat tissue, disrupts mitochondrial function, and lingers in your body for years, slowing energy output and triggering inflammation.
Q: How does LA affect gut health?
A: LA interferes with the metabolism of colon cells, which alters the gut environment by raising oxygen levels, harming beneficial microbes and favoring the growth of harmful bacteria. This shift leads to dysbiosis and increases the production of inflammatory compounds that breach your gut lining and enter your bloodstream, contributing to systemic inflammation.
Q: What foods should I avoid to lower my LA intake?
A: Steer clear of vegetable oils like soybean, corn, safflower, sunflower, and canola oils. Also limit high-LA foods such as processed snacks, fried foods, salad dressings, and even chicken, pork, nuts, seeds, and olive oil.
Q: How long does it take to get LA out of my body?
A: LA has a half-life of about two years, so it takes time to clear. However, every LA-free meal you eat helps reduce your oxidative burden, improve mitochondrial function, and restore metabolic health day by day.
Intimidation and Censorship — A Doctor’s Personal Account of the Pandemic
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/13/dr-mary-talley-bowden-intimidation-censorship.aspx
Analysis by Dr. Joseph Mercola July 13, 2025
Story at-a-glance
- Dr. Bowden used rapid PCR (polymerase chain reaction) tests and early interventions like monoclonal antibodies and ivermectin to successfully treat over 6,000 patients during the COVID-19 pandemic
- Government agencies and medical boards coordinated to suppress effective treatments while promoting expensive alternatives through an $11.5 billion propaganda campaign
- Hospitals indiscriminately used ventilators and harmful protocols, with some cases resembling euthanasia rather than proper patient care during the peak of the pandemic
- Athletic sudden deaths rose from 29 to 290 annually, with myocarditis cases rising significantly, yet politicians remain silent due to pharmaceutical industry influence
- Despite growing political support for medical autonomy, powerful medical organizations continue suppressing free speech and patient choice regarding treatments
In a three-hour interview with Joe Rogan, Dr. Mary Talley Bowden recounts her experience in the trenches during the COVID-19 pandemic.1 While she has saved thousands of lives, the establishment vilified her by refusing to use treatments they endorsed. I encourage you to watch the entire episode, as it’s an eye-opening story of what went on behind the scenes.
Early Testing and Treatment Save Lives
According to Bowden, early pandemic testing delays were severe, often lasting up to two weeks. These delays allowed the virus more time to spread, exacerbating illness and overwhelming health care systems.
• Quick testing helps the appropriate patients — Bowden contributed to widespread testing by adopting saliva-based polymerase chain reaction (PCR) tests, dramatically reducing waiting times to just 24 hours:
“I was already working with a lab for patients with chronic sinusitis, they were doing a PCR testing for chronic sinusitis. So, tests for bacterial and fungal infections of the sinuses. It’s called Microgen DX, and they came out with a saliva test for COVID.
So, we were able to get the results back the next day. So, I started offering that and my little clinic exploded …”
• Doctors still helped whenever they could — Even if patients already had a full-blown infection, Bowden was still bound by her oath to help treat them with whatever tools were available:
“I also had patients come in that were really sick in the second week. And that, that was such a learning experience for me because, you know, normally, if somebody walked into my office with an oxygen saturation in the low 80s, I would call an ambulance. But I had patients who were refusing to go to the hospital, and I had to give them the option to possibly die in my office, which is scary, but we saved them.”
• Monoclonal antibodies worked — Simply put, monoclonal antibodies are lab-grown antibodies2 designed to stimulate your immune system. Bowden recounts how they “worked very well” for her patients, and she would notice improvement the following day.
• Early treatment increases survival outcomes — Bowden says that patients coming in during the beginning phases of the disease helped improve their chances of full recovery:
“[O]nce I knew it was safe, then I started using [ivermectin] and found it worked … All in all, I treated well over 6,000 patients and everybody that got early treatment stayed out of the hospital.”
What Happens When Doctors Speak Out Against the Narrative
Bowden personally encountered severe side effects of the COVID-19 jab while treating patients. But when she spoke out, she was met with vehement opposition:
• More and more athletes are dying due to myocarditis — In 2023, I wrote about how athletes suddenly experiencing heart attacks when the shots were rolled out. Now, the situation has gotten worse, Bowden says:
“So, it used to be 29 per year. Now it’s 290 per year, [a] growth [of] 10 times … And I worry about these kids because myocarditis, the primary symptom is chest pain. But if you’ve got a kid who’s not even speaking yet, you have no idea if they have myocarditis, and myocarditis can leave a permanent scar on the heart and then lead to a lifelong increased risk of sudden cardiac death and we have no idea if these kids have been affected.”
• The government schemed to hit ivermectin — In addition to the rollout of the shots, Bowden believes there was a concerted effort by different parties to suppress ivermectin:
“[T]he Federation of State Medical Boards, which is this private entity — they’re actually located in Texas — who oversees all the state medical boards, they sent out a directive to all the state medical boards concerning ivermectin, concerning misinformation, and basically encouraging the medical boards to go after doctors like myself.”
• Opposition will have a hard time prosecuting lifesavers — While Bowden has been maligned, she is proud of what she did to help patients. In turn, her attackers have no leverage because in the end, she saved lives:
“They can’t find an expert witness to testify against me. There have been three continuances. They finally were awarded summary judgment against me. So, they’ve decided I’m guilty. And now I’m waiting for my punishment. There was a hearing about a month ago to find out what they’re going to find me with and that sort of thing. And I’m just waiting on that, but I do plan on appealing.”
Going deeper into the censorship angle, Bowden shares that the big players are working together to bring down cheap, effective treatments for patients suffering from the COVID-19 pandemic:
• Money was involved in propaganda and censorship — Bowden recounts that all the pieces moved very quickly at the start of the pandemic to usher in the shots as the primary solution:
“If you look at the timing, in March, the government put out the big information on ivermectin and why you should not take it for COVID. They put that on the FDA ‘s website. At the same time, they launched COVID-19 Community Corps, and this was April 1st, 2021.
This was an $11.5 billion slush fund to feed out propaganda and censor people. And the day that they launched the COVID-19 Community Corps was the same day that Houston Methodist, which is where I had privileges, mandated the COVID shots for all their employees, and they were the first in the country.”
• The government purposefully made it hard for doctors to do their jobs — This led to the suppression of effective treatments, such as monoclonal antibodies. Bowden said she didn’t even use ivermectin until the government took over distribution of monoclonal antibodies. After that, it became increasingly difficult to get them.

Save This Article for Later – Get the PDF Now
Were Hospital Protocols Helping or Hurting Patients?
Early pandemic hospital protocols often used ventilators aggressively and universally, regardless of patient-specific needs, frequently worsening outcomes for many individuals:
• Ventilators were forced on patients — Despite leading to worsened pulmonary function, hospitals still put patients on ventilators:
“You don’t look at a number to put somebody on a ventilator. And unfortunately, the people in the hospital didn’t learn. They didn’t experiment in that fashion. They just went by this protocol and automatically put people on ventilators. They also didn’t give people breathing treatments. They thought that breathing treatments would spread the virus.”
• Hospitals were indiscriminately harming patients — During the height of the pandemic, Bowden recounts that hospitals were essentially euthanizing patients to make room for others:
“They’ll justify giving morphine because they’ll say, ‘Oh, well, they’re struggling to breathe.’ Well, guess what? Morphine actually depresses your drive to breathe. Like this one case I remember, this patient, he was sick, he looked like he was dying, but they just pushed morphine. He had no pain. They do a pain score, so zero to 10.
This guy had zero pain. And then they pushed insulin to drop his sugar, and his glucose was fine. And then he died three minutes later … I reviewed this chart and turned him in the medical board. Nothing. They didn’t do anything.”
• Profits over lives — In the end, Bowden believes that greed ultimately won out, with the COVID shots linked to the deaths of countless people:
“[W]e have hard facts showing it should be pulled off the market. I mean, any other product would have been pulled a long time ago. If this were an antibiotic and we’d seen all the carnage from an antibiotic, it would have been yanked off long ago. It should have been yanked off in the first month. There’s no other explanation than there’s just fraud, there’s corruption, there’s ego, there’s money. But it’s not science.”
Medical Freedom Is Constantly Under Threat
Recent victories for medical freedom, such as Idaho’s ban on jab mandates,3 demonstrate growing support for patient autonomy. Yet powerful medical organizations remain opposed to broad reforms.
• More like-minded politicians are needed — Bowden formed the Americans for Health Freedom to increasingly influence policy discussions, advocating strongly for the restoration and protection of medical freedoms:
“I started an organization called Americans for Health Freedom to try to find the politicians with moral courage to simply state that the COVID shot should be pulled off the market. It has been slow-growing, but we are up to 252 politicians who will go on record just to state that these shots should be pulled off the market.”
• Politicians have been bought — Rogan and Bowden agree that money has caused many politicians to stay quiet about the efficacy and safety of the shots, most likely because of Big Pharma’s bribery:
“[T]hese politicians are not getting these shots anymore and they’re not giving them to their kids, and yet they’re fine just staying quiet and not saying anything. They’re fine letting their constituents get these shots when we know all the complications, we know that it doesn’t work.
We know that the risk far outweighs the benefit, and the politicians are staying quiet. So, our goal is to support the ones who will speak up and get them more power.”
• Organizations continue to suppress free speech — Bowden frequently clashed with mainstream medical experts during the pandemic. She called out the Texas Medical Association, saying:
“They are anti-free speech for physicians. They are pro-mandate. They’ve gone after me, and they have a tight control over the people in our House and State. So, I just think we need to be careful. I mean, you saw it during the pandemic and the economy of our state is dominated by health, and people don’t realize that. They just think oil, but health is a huge dominating factor in our economy and, you saw what they did to me, what they’re still doing to me.”
The Best Ways to Protect Yourself
Despite the assault on physicians and patient medical freedom, Bowden hasn’t given up. Things are looking up, and she hopes that the new Health Secretary, Robert F. Kennedy Jr, “will save us all.” In the meantime, there are things you can do to protect yourself against the ever-evolving SARS-CoV-2 variants, as well as other diseases by boosting your immune system.
As noted in Dr. Patrick Soon-Shiong’s interview with Tucker Carlson, your immune system is everything, especially against chronic diseases. However, many people have compromised immune function nowadays due to getting the shot. To rebuild your resilience, here are my recommendations:
1. Prioritize sleep — Ensure you’re getting at least seven to nine hours of high-quality sleep every night. Sleep is when your body heals and rejuvenates. Lack of proper sleep weakens your immune system and increases inflammation. But that’s not all — you also need to consider sleep quality. For simple, actionable fixes that will help you get the rest you need, read “Subtle Signs You Are Not Getting Enough Sleep.”
2. Dietary adjustments — Your diet plays a huge role in your overall health. If you’re eating unhealthy foods, it’s time to change. Limit ultraprocessed foods, refined sugar, and linoleic acid (LA), which is an inflammatory polyunsaturated fat (PUF). Focus instead on healthy carbohydrates to optimize your metabolic health and reduce immune-damaging inflammation.
3. Sunlight exposure — In a previous article, I noted that vitamin D from sunlight exposure helps prevent respiratory infections. I recommend you get daily sunlight exposure at solar noon, but only after you’ve been off vegetable oils for two to six months.
4. Add C15:0 fat to your diet — In relation to the point above, did you know that after you eat enough LA, it becomes embedded in your skin? Once it’s exposed to sunlight, inflammatory metabolites are produced, leading to increased risk of chronic disease and inflammation.
Taking 250 milligrams of pentadecanoic acid (C15:0) daily may help shorten the time it takes for your skin to safely interact with sunlight again, but emerging research suggests much larger doses may be even better.
The logic behind this strategy is to push out the existing LA from your tissues, replacing them with healthier fat. If you simply followed a low-LA diet, it would take two to three years for the strategy to work. But if you add C15:0, the LA clearance significantly shortens to 12 to 18 months. To understand this strategy in more detail, read “The Skin Microbiome Secret to Sun Protection and Radiant Health.”
5. Manage your stress — Chronic stress weakens your immune response due to elevated cortisol levels. Engage in daily stress-relief activities like meditation, deep breathing exercises, gentle yoga, or simply spending more time in nature. For more information, read “Key Strategies to Reduce Your Cortisol Levels.”
6. Don’t get the COVID shot — Given concerns raised by Bowden about serious side effects, opting out of the COVID jab and focusing instead on natural strategies to boost your immunity provides a safer, more effective approach.
If you or a loved one has already gotten the jab, I recommend you go over the I-RECOVER program by the Independent Medical Alliance (IMA), formerly known as the Front Line COVID-19 Critical Care Alliance (FLCCC). It provides extensive information about how to treat long COVID4 and post-jab injuries.5
Frequently Asked Questions (FAQs) About the Doctors During the COVID-19 Pandemic
Q: What was Bowden’s approach to COVID-19 testing and early treatment?
A: Bowden emphasized that early testing and intervention were crucial in saving lives during the pandemic. She implemented saliva-based PCR testing with a 24-hour turnaround, enabling faster diagnosis compared to the then-common two-week delays. She treated patients with monoclonal antibodies and ivermectin, and that early intervention kept thousands out of the hospital.
Q: Why did Bowden face backlash from the medical establishment?
A: Bowden publicly challenged the mainstream COVID-19 treatment protocols, questioned the shot safety, and promoted off-label use of ivermectin. As a result, she was targeted by medical boards and hospital administrators who allegedly acted on federal directives to suppress dissent. She claims that propaganda, financial incentives, and censorship motivated the backlash, not science.
Q: How did hospital protocols during the pandemic impact patient outcomes, according to Bowden?
A: Bowden criticized hospitals for over-reliance on ventilators, often administered without patient-specific evaluation. She alleges that some institutions essentially euthanized patients through unnecessary morphine and insulin use, and even withheld supportive care like breathing treatments. She argues that these decisions were driven by protocols, profit motives, and flawed incentives — not patient welfare.
Q: What role does Bowden believe government and pharmaceutical interests played in shaping the pandemic response?
A: She asserts there was a coordinated effort to suppress effective, low-cost treatments like ivermectin in favor of shot mandates. She points to initiatives like the $11.5 billion COVID-19 Community Corps, claiming it was used to spread propaganda and enforce censorship, while pharmaceutical interests influenced both policy and the public’s perception.
Q: What is Bowden’s stance on medical freedom and jab mandates today?
A: Bowden founded Americans for Health Freedom, an organization aimed at supporting politicians who oppose COVID-19 shot mandates and advocate for medical autonomy. She celebrates moves like Idaho’s decision on mandates and criticizes institutions like the Texas Medical Association for suppressing physician free speech.
– Sources and References
What to Do if You Get Diagnosed with an Ovarian Cyst
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/05/what-to-do-diagnosed-with-an-ovarian-cyst.aspx
Analysis by Dr. Joseph Mercola July 05, 2025

Story at-a-glance
- Most ovarian cysts are harmless and disappear naturally, but some cause severe complications like rupture or twisting the ovary, requiring emergency surgery
- Vegetable oils like canola and sunflower act as fake estrogens, damaging ovarian tissue and fueling cyst formation due to linoleic acid content
- PCOS drives recurring cysts through hormonal chaos, particularly insulin resistance and elevated estrogen that disrupts normal ovarian function and cycles
- Natural pain relief includes heat therapy, massage, and gentle movement, while chamomile and ginger teas help reduce inflammation and balance hormones
- Prevention focuses on eliminating vegetable oils, addressing insulin resistance and considering natural progesterone to restore hormonal balance and stop cyst recurrence
Ovarian cysts are among the most common gynecological findings, yet they often strike without warning. These fluid-filled sacs grow on or inside the ovaries and are typically harmless. But when they rupture, twist the ovary or grow too large, they trigger sudden, severe pain, disrupt your hormones, and even threaten fertility. In rare cases, they signal ovarian cancer.
Most women don’t even know they have a cyst until an ultrasound reveals it. That’s a concerning gap in awareness, especially considering the risk of complications. Pain in your lower abdomen, bloating, irregular periods, pain during sex, and changes in urination or bowel habits are common signs of an ovarian cyst. But depending on its size and type, some women feel nothing at all.
While about two-thirds of cysts disappear on their own, some do not.1 In some cases, cysts even cut off blood flow, requiring immediate surgery to save the organ. The concern isn’t just the cyst, however — it’s the conditions that create them. Polycystic ovary syndrome, or PCOS, is one major culprit. Characterized by irregular periods, facial hair, weight gain, and multiple small cysts, PCOS is also linked to infertility and insulin resistance.
Left unmanaged, it opens the door to long-term hormonal chaos. Understanding what kind of cyst you have and what caused it, is the key to avoiding unnecessary treatment, managing your symptoms and preserving your reproductive health. That’s where the first set of findings comes in.
Some Cysts Vanish on Their Own, While Others Send You Straight to the ER
Ovarian cysts are not always a cause for alarm, as many are part of a woman’s normal cycle. Speaking with TIME, ob-gyn Dr. Mary Jane Minkin of Yale Medicine explains that ovulation itself often produces what’s called a “functional cyst.”2 This happens when a follicle, the small sac that holds your egg, swells up with fluid during the release process. These types of cysts usually dissolve on their own without causing problems.
• But some cysts don’t disappear — and that’s when trouble begins — If a cyst grows too large, ruptures or causes ovarian torsion (twisting of the ovary), it often becomes a medical emergency. If torsion cuts off blood flow to the ovary, it risks permanent damage. Symptoms like intense pain, nausea and vomiting are red flags that demand immediate care.
Transvaginal ultrasound remains the gold standard for evaluating ovarian cysts. Radiologists look at shape, size, fluid content and blood flow. These details help determine whether the growth is benign or needs further attention.
• Size, content, and structure guide your next steps — Cysts filled only with fluid and under about 5 centimeters are often left alone. But if they have “solid components” or fingerlike projections, or if they keep growing, doctors often order blood tests such as cancer antigen 125 (CA-125) to check for cancer-related proteins.
• You may not need surgery even if you’re over 50 — One study followed women over 50 who had stable ovarian cysts and found their risk of developing ovarian cancer was just 0.27% over 3.5 years.3 That means many postmenopausal cysts are still safe to monitor rather than remove immediately.
• Ovarian preservation is part of the strategy — Even when surgical removal is necessary, doctors try to avoid removing the entire ovary whenever possible. Preserving hormonal function is key to protecting your heart, bones and brain long-term, especially if you’re still menstruating.
Ovarian Cysts Form for Many Reasons — and Not All Cysts Are Harmless
According to the Cleveland Clinic, while most ovarian cysts are classified as “functional” and develop as part of ovulation, other types like dermoid cysts, cystadenomas and endometriomas don’t follow this pattern.4 These growths form due to abnormal cell reproduction or endometriosis and need more monitoring to ensure they don’t lead to complications.
• Some cysts don’t cause symptoms, but others press on organs — Depending on their size and location, these growths may trigger pain in your back or pelvis, frequent urges to urinate or even pain during sex. Large cysts often create pressure and discomfort in the lower abdomen, especially if they start pressing against your bladder or bowel.
• Hormonal disorders raise your odds of getting more cysts — If you’ve ever had a cyst before, your chances of getting another are higher. But conditions like endometriosis or PCOS significantly raise the risk by disrupting your hormonal balance. Medications used to stimulate ovulation, like Clomid, also increase cyst formation.
• Cysts don’t always stay small — when they grow, the risks climb — While many shrink and disappear within a few menstrual cycles, some keep growing. Once a cyst crosses the 10-centimeter mark (nearly 4 inches), doctors often recommend surgical removal. This is especially true if the cyst starts causing pain or shows signs of abnormal structure on ultrasound.
• Ovarian cysts are rarely cancerous, but some are — Fewer than 1% of ovarian cysts turn out to be cancer. However, the odds increase if you’re postmenopausal. If the cyst is complex or solid in appearance, or if blood tests show high CA-125 levels, your doctor may refer you for a deeper evaluation.
• Prevention isn’t always possible, but tracking your symptoms helps — Most cysts don’t require treatment. But if you feel bloated, notice changes in your period or have pelvic pain that won’t go away, bring it up. Keeping track of symptoms gives your provider better insight into whether you need imaging or follow-up care.

Save This Article for Later – Get the PDF Now
Vegetable Oils Act Like Fake Estrogens and Damage Your Ovaries
In a study published in Environmental Science and Pollution Research, researchers tested common vegetable oils on female rats over a 28-day period and found they harmed ovarian function.5 The oils tested included genetically modified (GM) canola, GM maize and sunflower.
• Even without affecting basic hormone levels, these oils caused visible ovarian damage — The study found no major changes in lipid profiles or in the main reproductive hormones, but serum estradiol levels spiked in both the canola and sunflower oil groups.
Estradiol is a form of estrogen, and elevated levels of it are known to fuel cyst formation and disrupt ovarian function. Rats fed these oils developed ovarian atrophy, meaning the ovaries began to shrink and weaken structurally.
• Sunflower oil caused the most severe ovarian changes — While all oil-fed rats showed some form of ovarian toxicity, the sunflower group displayed the worst damage. Researchers observed severe congestion of ovarian blood vessels and numerous follicular cysts — fluid-filled sacs that distort normal ovary function. This mirrors the type of cystic development often seen in PCOS and other reproductive disorders.
• Canola oil triggered similar ovarian degeneration — The canola group also experienced atrophied ovaries and elevated estradiol levels. Although the structural damage wasn’t as extreme as in the sunflower-fed rats, it still indicated hormonal disruption and tissue breakdown. The presence of secondary and simple cysts pointed to interference with the ovulation process and follicular development.
• PUFs act like xenoestrogens inside the body — Bioenergetic researcher Georgi Dinkov emphasized that polyunsaturated fats (PUFs) like linoleic acid (LA), found in these oils, behave like endocrine-disrupting chemicals.6
That puts them in the same category as compounds like phthalates, parabens, and bisphenols. These substances mimic estrogen and hijack normal hormone signaling, leading to overstimulation of estrogen receptors in reproductive organs.
Unlike synthetic chemicals, which are increasingly regulated or avoided by health-conscious consumers, PUFs from vegetable oils are still consumed in massive quantities. They’re marketed as healthy, yet this study showed they have a direct toxic impact on ovarian structure — without the protections or warnings given to more notorious hormone disruptors.
• Estrogen overload from dietary oils fuels cyst formation — The mechanism is clear: elevated estrogen, triggered by LA-rich vegetable oils and other endocrine disruptors, increases the likelihood of abnormal follicle growth and cyst development. When your ovaries receive repeated, estrogen-like signals from environmental sources, they lose the ability to maintain balanced hormone cycles, setting the stage for dysfunction.
If you’re struggling with irregular cycles, ovarian cysts or PCOS symptoms, eliminating canola, sunflower and other vegetable oils is a key step. These oils actively interfere with your reproductive health on a cellular level. Awareness and dietary changes give you a powerful way to start reversing the damage.
Natural Therapies Help Ease Symptoms
While most home remedies won’t shrink cysts, they do ease your discomfort. At-home strategies like heat therapy and stretching help relieve pressure and reduce pain from ovarian cysts. These are symptom-focused tools, not treatments for the cyst itself. Still, if you’re in pain, these methods help you feel more in control and less anxious.
• Pain relief is more effective when you target tight muscles — Ovarian cyst pain often leads to muscle tension in your lower back, stomach or thighs. Massaging these areas reduces the surrounding tightness and improves your comfort.7 Other options include warm compresses or alternating heat and ice packs to loosen muscles and improve blood flow, both of which reduce the perception of pain.
• Movement is medicine, especially if your cysts are linked to PCOS — A systematic review found that regular exercise, especially when combined with dietary changes, had a stronger impact on PCOS symptom relief than diet alone.8 Daily walking is important, and yoga is another good place to start. It reduces stress hormones, increases flexibility, and supports hormonal regulation, all of which help if your cysts are tied to hormonal imbalance.
• Relaxation techniques go a long way toward managing pain — Stress amplifies pain, and cyst-related anxiety makes everything feel worse. Gentle exercises like slow breathing, guided meditation and yoga movements help interrupt pain signals and calm your nervous system.
• Chamomile and ginger tea help your hormones — Chamomile helps reduce menstrual cramps and inflammation. It also lowers testosterone levels, which are often elevated in women with PCOS.9,10 Ginger supports this process by reducing inflammation and helping balance reproductive hormones.11 These herbal teas help support hormonal recovery at the root level.
How to Support Your Ovaries and Stop Cysts from Coming Back
If you’ve been diagnosed with an ovarian cyst, or if you’re dealing with recurring ones, the next step isn’t just managing the pain. You need to focus on the root cause. Whether your cysts are tied to hormone imbalance, diet or environmental exposures, the goal is to create a body environment where those cysts don’t keep forming.
I want to help you take back control by giving you practical, no-nonsense steps that target what’s really going on under the surface. To begin rebuilding your hormonal foundation from the inside out, here’s where I recommend you start:
1. Eliminate vegetable oils from your diet — Stop eating LA in vegetable oils like canola, sunflower, corn, soybean, and grapeseed oil. These oils are marketed as healthy, but they act like synthetic estrogens inside your body.
They overstimulate your ovaries and fuel cyst development, even causing atrophy and congestion in ovarian tissue. Stop cooking with them. Stop eating processed foods made with them. Swap them out for saturated fats like tallow, ghee or grass fed butter.
2. If you have PCOS, fix the root issue — don’t just manage the symptoms — PCOS is driven by hormonal chaos, especially insulin resistance and excess androgens like testosterone. To start correcting it, you’ll need to move your body regularly — walking, stretching, and strength training all count.
You’ll also want to eliminate endocrine-disrupting chemicals and foods from your routine. That means cutting out plastic containers, personal care products with phthalates, and anything containing seed oils.
Vitamin D deficiency and insufficiency are also common among PCOS patients. Get regular daily sunlight to optimize your vitamin D — but avoid peak sun hours (10 a.m. to 4 p.m.) until you’ve cut back on LA for at least six months. These changes will reduce cyst formation and help bring your hormones back into balance.
3. Consider using natural progesterone to restore balance — If your cysts are tied to hormone imbalances, especially high estrogen, natural progesterone offers a powerful, targeted solution. Progesterone directly counteracts the effects of excess estrogen and helps normalize your cycle.
A 2020 study found that “cyclic progesterone for PCOS lowers androgens and restores estradiol-progesterone balance.”12 Used correctly, natural progesterone supports ovulation, reduces cyst formation and brings your hormones back into sync, without the side effects of synthetic options.
4. Take the guesswork out of your insulin status — If your cysts are connected to PCOS, there’s a good chance you’re insulin resistant, even if your blood sugar looks normal. Ask your practitioner for a test called HOMA-IR, short for Homeostatic Model Assessment of Insulin Resistance.
This test looks at both fasting insulin and glucose to show how well your body is processing sugar. If your score is above 1.0, it’s time to clean up your carb quality, lower LA intake and focus on blood sugar stability.
5. Use pain relief and movement to stay consistent while you heal — If your cyst is causing you pain, don’t wait it out in bed. Use a warm compress on your abdomen to increase blood flow. Massage the surrounding areas, especially your lower back and thighs.
Gentle yoga or walking helps keep your hormones moving in the right direction and stops muscle tension from making things worse. The goal is to stay active and consistent, not push through unbearable pain.
FAQs About Ovarian Cysts
Q: What causes ovarian cysts, and are they dangerous?
A: Ovarian cysts are fluid-filled sacs that often form during ovulation. Most are harmless and resolve on their own. However, some cysts grow large, rupture or twist the ovary, which causes intense pain and requires emergency surgery. In rare cases, complex cysts, especially those with solid components, are a sign of ovarian cancer.
Q: Do vegetable oils really affect your ovaries?
A: Yes. Research shows that vegetable oils high in LA, such as canola and sunflower oil, act like xenoestrogens — compounds that mimic estrogen in your body. These oils trigger ovarian atrophy, hormonal disruption and the development of cysts, even without raising conventional hormone markers. Eliminating these oils is a key first step in protecting ovarian health.
Q: What’s the link between PCOS and ovarian cysts?
A: PCOS is a hormonal disorder that causes irregular periods, high androgens (like testosterone), insulin resistance and the formation of multiple small cysts on the ovaries. PCOS is a root cause of recurring cysts and is strongly influenced by lifestyle factors like diet, movement and exposure to environmental toxins.
Q: Are there natural ways to relieve cyst-related pain and symptoms?
A: Yes. Heat therapy, massage, and gentle movement like yoga ease pelvic pressure and reduce pain. Herbal teas like chamomile and ginger help lower inflammation and balance hormones. These remedies won’t shrink the cyst itself but do improve your comfort and support hormonal healing while you address the root cause.
Q: What’s the best way to stop ovarian cysts from coming back?
A: Start by removing dietary sources of linoleic acid (vegetable oils), addressing insulin resistance through a blood test like HOMA-IR and cleaning up environmental hormone disruptors. If you have PCOS, support your body with regular movement, consider natural progesterone and focus on hormone-friendly habits like drinking herbal teas and managing stress.
- 1, 2 TIME May 13, 2025
- 3 Gynecology October 2024, Volume 231, Issue 4, P440.E1-440.E7
- 4 Cleveland Clinic, Ovarian Cysts
- 5 Environmental Science and Pollution Research February 2022;29(6):9153-9163
- 6 To Extract Knowledge from Matter
- 7, 9 Medical News Today, Home remedies for ovarian cyst symptoms
- 8 Syst Rev. 2019 Feb 12;8:51
- 10 J Res Med Sci. 2018 Apr 26;23:33
- 11 Front Nutr. 2022 Nov 29;9:1071515
- 12 Drug Discovery Today: Disease Models, Volume 32, Part B, Winter 2020, Pages 71-82, Highlights
High-Fat Diets Increase Breast Cancer Risk and Metastasis
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/05/27/high-fat-diets-breast-cancer-risk-metastasis.aspx
Analysis by Dr. Joseph Mercola May 27, 2025

Story at-a-glance
- Eating a high-fat diet (defined as 60% of daily calories) significantly increases your risk of developing breast cancer and accelerates the disease’s spread throughout your body
- High-fat foods activate your platelets, making them overly sticky, which helps cancer cells attach and grow rapidly in vital organs like your lungs
- Unhealthy fats, commonly found in processed foods and fast food, trigger harmful inflammation and hormonal imbalances that directly fuel breast cancer
- Making simple dietary shifts, such as cutting down on processed foods and vegetable oils, dramatically reduces your breast cancer risk and supports healthier cell function
- Regularly choosing whole, nutrient-dense foods and healthy carbohydrates helps your body lower inflammation, balance hormones, and create an environment less conducive to cancer growth
Breast cancer, characterized by lumps in the breast, unexplained swelling, skin changes, and sometimes persistent pain, remains the second most common cancer among women worldwide. In the U.S. alone, the American Cancer Society estimates that 316,950 women will be diagnosed with this disease in 2025.1
While it’s commonly believed that breast cancer occurs due to factors such as gene mutations or inherited genes, research shows that there’s one alarming factor that dramatically influences risk — your diet. Specifically, eating a diet excessively high in fat.
A High-Fat Diet Makes Cancer Spread Faster
A study published in Nature Communications2 explored how a high-fat diet speeds up the spread of breast cancer, particularly focusing on the role played by platelets, which are blood cells involved in clotting. Specifically, the researchers set out to determine the link between 60% of calories as fat and faster cancer metastasis (the spreading of cancer cells) into the lungs.
• A high-fat diet had a significant effect on platelet activation — Platelets in mice fed a diet consisting of 60% fat did not behave normally. They became excessively sticky and aggressive, and began forming clumps, especially in the lung tissues.
• Aggressive platelets didn’t just randomly cluster — These cells specifically released a protein called fibronectin, which significantly enhances the cancer cells’ ability to stick to blood vessels. Fibronectin acts like glue, providing cancer cells with a firm grip onto blood vessel walls.
Without fibronectin, cancer cells would struggle to latch onto the blood vessels in the lungs, severely limiting their potential to invade and spread. But when fibronectin levels are elevated, as it happens with high-fat diets, cancer cells easily attach, survive, and rapidly proliferate in new areas.
• Fibronectin damages cellular health — To confirm how pivotal fibronectin was, the researchers conducted an additional test — they blocked fibronectin’s action. In doing so, they dramatically slowed cancer spread, emphasizing how damaging a high-fat diet can be by ramping up fibronectin production.
• Reversing the harmful effects is doable — When the researchers switched the test mice from a high-fat diet back to a normal one, they noticed a significant reduction in platelet activation and cancer spread.
The change didn’t take long, showing that dietary adjustments provide rapid and powerful protection against metastasis. It’s a convincing reason to take immediate action, especially if you’re constantly consuming high-fat meals.
• Blood coagulation provides a clue to cancer risk — Another observation was related to blood coagulation times. Blood from the animals on high-fat diets coagulated faster — a change that accurately predicted worse outcomes. Essentially, faster blood-clotting indicates platelet hyperactivity, making your bloodstream a more hospitable environment for cancer cells.
By monitoring blood clotting times, health care providers can identify individuals at greater risk of aggressive cancer spread due to dietary factors, enabling earlier and more targeted interventions.
• The mechanism of platelet hyperactivation is closely linked to dietary fats — As noted earlier, activated platelets secrete high amounts of fibronectin, setting the stage for cancer metastasis by enhancing cancer cell adhesion to the blood vessels and lung tissues. But there’s another mechanism at play — they also shield cancer cells from your immune system.
Normally, your immune cells patrol your bloodstream, identifying and eliminating rogue cancer cells. However, these clumped platelets form a protective barrier around cancer cells, making them practically invisible to immune surveillance. As a result, cancer cells survive longer, multiply rapidly, and spread more efficiently throughout your body.
• Obesity compounds the risks of a high-fat diet — According to the researchers, having excess weight worsens the metastasis:
“As well as affecting primary BC [breast cancer] tumor growth, obesity enhances the metastasis of these cells to the lungs in a manner that is dependent on neutrophils, involving vascular dysfunction and increased endothelial transmigration of the tumor cells.
Moreover, obesity also induces chronic inflammation, while enhancing pro-thrombotic signaling in both platelets and endothelial cells, and promoting a state of hypercoagulability in cancer patients.”
Other Research Supports the Link Between Fat Intake and Higher Breast Cancer Risk
In a similar study published in Cureus,3 researchers conducted a meta-analysis to determine whether diets high in fat directly influence the risk of breast cancer in women. They chose eight studies from various countries, that involved large and diverse sample sizes, ranging from groups as small as 172 up to 91,779 people.
Each of the selected studies measured dietary fat intake among participants using food questionnaires and tracked breast cancer diagnoses through medical records confirmed by histology or radiological methods. Just like the Nature Communications study, the findings were clear for this one — high dietary fat significantly increased the risk of developing breast cancer.
• High polyunsaturated fat (PUF) intake is harmful — The study identified PUFs, particularly omega-6, as particularly detrimental. As noted by the researchers:
“[O]verall caloric intake has a larger impact on the development of obesity, which is linked to redox and hormonal abnormalities that promote tumor proliferation …
[E]xcess oxidative stresses may activate many transcription factors, including those that control the expression of genes implicated in pro-inflammatory pathways. The effect of polyunsaturated fatty acids (PUFAs) on cancer risk has been shown to depend on the ratio of -6 to -3 PUFAs. In vivo findings demonstrated that -6 PUFAs stimulate tumor development, while -3 PUFAs are protective.”
• Timing and duration of fat consumption influence cancer risk — Researchers noted that consistent consumption of high-fat foods over several years markedly amplified the risk. In other words, prolonged exposure to these dietary fats created cumulative damage, increasing the likelihood of breast cancer diagnosis later in life.
• The underlying biological mechanisms of fat intake on cancer — Excess fat consumption elevates your body’s levels of harmful substances called reactive oxygen species (ROS). These are unstable molecules that cause oxidative stress in cells, leading directly to DNA damage and cancerous changes.
Chronic oxidative stress doesn’t just damage individual cells — it sets off a chain reaction of inflammatory reactions, activating genes known to drive breast cancer growth.
• High intake of unhealthy fats disrupts hormone levels — The researchers noted that excess body fat tissue actively produces estrogen, and elevated estrogen levels strongly correlate with breast cancer development, especially in postmenopausal women. The estrogenic activity accelerates breast cell growth. Thus, consuming high-fat diets also indirectly amplifies the body’s own hormonal environment.
Just like the previous study, this research makes it clear that the amount of fat you put on your plate each day influences your risk of breast cancer. Reducing dietary fats, particularly those that trigger chronic inflammation and hormone imbalances, like omega-6 fats will improve your risk of developing breast cancer.

Save This Article for Later – Get the PDF Now
Reduce Your Breast Cancer Risk by Changing Your Diet
To reduce your risk of breast cancer, addressing the root cause — your diet — is necessary. As shown in the studies, eating a high-fat diet sets the stage for inflammation, hormone imbalances, and aggressive cancer growth.
I recommend you take immediate action today to reverse the risks mentioned and build a healthier future. Here are my five strategies that will set you on the right path:
1. Cut back on linoleic acid — Linoleic acid (LA) is a harmful type of fat commonly found in vegetable oils and processed foods, as it promotes inflammation that fuels cancer growth. Start checking labels carefully and avoid foods containing soybean oil, corn oil, sunflower oil, safflower oil, and ultraprocessed foods.
Choose healthier fats like grass fed butter, ghee, or tallow instead, as these fats do not contribute to inflammation and help protect your cellular health. For more information on how LA causes cellular damage, read my article “Linoleic Acid — The Most Destructive Ingredient in Your Diet.”
2. Moderate your fat intake — As the earlier research noted, high levels of fat are strongly linked to breast cancer, but completely eliminating fat is neither realistic nor healthy — the key is moderation. Aim for dietary balance, because your body still needs fat to function properly.
For metabolic efficiency, aim for a daily fat intake of about 30% of daily calories, and ensure they come from healthy sources, including full-fat raw dairy, which is a primary source of the essential odd-chained fat C15:0. Glucose is the preferred fuel for your cells, so those should make up the bulk (45% to 55%) of your calories.
3. Switch to whole, nutrient-dense foods — If you’re regularly eating processed or fried foods, now’s the right time to make a change. Swap out processed meals and snacks for natural, nutrient-dense whole foods.
Good choices include fresh vegetables, fruits, pasture-raised meats, wild-caught seafood, pastured eggs, and raw, grass fed dairy. These foods provide essential nutrients that support your immune system and promote optimal health.
4. Optimize your carb intake for healthy cells — Your cells rely heavily on carbohydrates for energy, so severely restricting carbs is not a good idea. Instead, choose healthy carbohydrates to fuel cellular energy without triggering inflammation.
Whole fruits (with pulp), cooked root vegetables, and easily digestible sources like white rice will provide stable, beneficial carbohydrates. These carbs support balanced hormone levels and reduce the oxidative stress that feeds cancer growth.
5. Get regular exercise — Supporting your healthy diet by adding regular exercise is an effective way to protect your health against cancer. Research shows that higher muscle strength and cardiovascular fitness reduced all-cause mortality by 31% to 46% across different cancer types and stages.4
Now, what kind of exercises are good for you? The best, and easiest one, you can do right away is go for a walk outside — aim for 10,000 steps a day. If you’re doing strength training, the sweet spot is around 40 to 60 minutes per week.
Any longer than that, your longevity becomes the same as if you weren’t exercising at all. For a more detailed explanation on this topic, read my article “Physical Fitness Strongly Linked to Improved Cancer Survival, Study Shows.”
Frequently Asked Questions About the Link Between High-Fat Diets and Breast Cancer
Q: How does a high-fat diet influence the spread of breast cancer?
A: A high-fat diet dramatically accelerates metastasis of breast cancer cells by altering platelet behavior. Platelets become hyperactive and release fibronectin, a protein that helps cancer cells stick to blood vessel walls and invade other organs, especially the lungs. This dietary pattern also leads to faster blood clotting, which predicts more aggressive cancer progression.
Q: Can changing my diet reduce breast cancer risk?
A: Yes, dietary changes rapidly and significantly reduce cancer risk. Research shows that switching from a high-fat to a whole-food diet with an emphasis on carbohydrates as cellular fuel decreases platelet activation and fibronectin production, reducing the likelihood of cancer cells from spreading.
Q: What types of fats are most harmful when it comes to breast cancer?
A: Polyunsaturated fats (PUFs), especially omega-6 fatty acids found in vegetable oils (like corn, soybean, and sunflower oil), are particularly dangerous. They promote oxidative stress, hormonal imbalances, and chronic inflammation — all factors that contribute to tumor growth and metastasis. While omega-3 is beneficial for overall health, moderation is required because even too much healthy fats won’t be good for you.
Q: How does obesity interact with dietary fat to affect breast cancer?
A: Obesity exacerbates the harmful effects of a high-fat diet. It leads to chronic inflammation, vascular dysfunction, and increased blood clotting, all of which support cancer metastasis. Obese people also experience hormonal imbalances, particularly increased estrogen levels, which fuel breast cancer cell growth, especially after menopause.
Q: What are the recommended steps to reduce dietary risks for breast cancer?
A: To lower your risk, follow the recommendations below:
•Avoid vegetable oils — Take note of products containing soybean, corn, safflower, and canola oil.
•Keep fat intake below 30% of daily calories — Look for healthy, animal-based fats like ghee or grass fed butter. Coconut oil is also recommended.
•Eat whole, unprocessed foods — Examples include vegetables, fruits, and raw, grass fed dairy.
•Focus on healthy carbs — Dietary recommendations include root vegetables and white rice.
•Exercise regularly — Aiming for 10,000 steps per day and 40 to 60 minutes of weekly strength training.
The Immune System Is Your Body’s Defense Against Cancer
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/05/25/immune-system-bodys-defense-against-cancer.aspx
Analysis by Dr. Joseph Mercola May 25, 2025
Story at-a-glance
- Cancer is affecting younger individuals more than before. There’s even a case wherein a 13-year-old has developed metastatic pancreatic cancer
- Inflammation plays a central role in cancer development, with poor diet, environmental chemicals, and persistent viral infections contributing to immune system suppression
- The COVID-19 jab contributes to cancer risk through persistent inflammation from spike proteins
- Your immune system, particularly T-cells and natural killer cells, is crucial for fighting cancer
- Practical preventative measures include eating whole foods instead of processed foods, reducing chemical exposure, maintaining proper sleep, and avoiding mRNA shots
Cancer was once viewed as a disease that rarely surfaced in younger individuals, but today, that assumption no longer holds. So, what makes the current cancer trend so alarming? This, along with other topics, was discussed by Dr. Patrick Soon-Shiong, a surgeon and businessman, in an interview with Tucker Carlson, featured above.1
Most arguments about cancer center on genetic predisposition or external carcinogens like cigarettes. That conversation has merit, but it misses a key piece of the picture — your body’s own immune defenses. The bigger story involves strengthening the body’s protective mechanisms, and avoiding repeated hits to those defenses that allow cancer cells to take hold.
Investigating the Root Cause
Younger individuals once escaped the worst forms of cancer, but that has changed. Soon-Shiong tells the story of a case of a 13-year-old with metastatic pancreatic cancer, which in the past was basically unheard of. A growing body of clinical observation suggests that these cancers progress faster than older standards would predict, prompting doctors to label them “turbocharged” tumors.
• Inflammation is at the root of cancer — In Soon-Shiong’s words, your body “must inhibit the thing called P53 … and protect your body from … cancer. And if it persists and causes inflammation and inhibits P53, it begins to have the hallmarks of an oncogenic virus.”
• The rise of modern diets contribute to cancer — Soon-Shiong noted that ultraprocessed foods and other toxins keep a person’s gut in disarray. That scenario can worsen the immune system’s struggles. Excess linoleic acid from canola, soy, or similar oils triggers chronic inflammatory signals in many individuals.
These signals disrupt the cellular environment that NK cells and T-cells need for normal function. Meanwhile, diets that rely on refined sugar and cheap filler starches can further undermine metabolic health, though the problem runs deeper than sugar alone.
• Manmade chemicals in the environment also contribute to cancer — These include PFAS, red dyes, pesticide residues, and continuous exposure to microplastics and endocrine disruptors that hamper the body’s inherent defenses. Extra stress placed on immune cells can push them toward a suppressed state, giving malignant cells the opportunity to thrive.
Some interpret these trends as a perfect storm of poor nutrition, hidden toxins, and immunosuppression. Yet Soon-Shiong remains guardedly hopeful. He points to practical methods that hinge on T-cell function and a different approach to therapy. By focusing on the body’s innate ability to kill tumors, he believes more children and younger adults will be able to escape from this dreaded disease.
Is COVID-19 Altering Your Immune System in New Ways?
Soon-Shiong places part of the blame for rising cancer rates on persistent, chronic inflammation. His suspicion includes both COVID infections and the COVID jabs, wherein the virus’ spike protein lingers in tissues well after an active infection has ended. That prolonged presence maintains a continuous inflammatory response, fueling immune dysregulation.
• Standard antibody-based COVID shots have not cleared the virus from the body — Soon-Shiong wonders if repeated boosters further embed these spike protein fragments. He believes the shot keeps your immune system busy without resolving the underlying threat.
• COVID-19 gets into every cell of your body — Soon-Shiong also noted that spike protein, either from infection or the COVID shot, penetrates all of your cells, including the cells lining your blood vessels. As he explains in the interview:
“It goes wherever you have the thing called the ACE2 receptor, which is in the blood vessels. So, wherever we have a blood vessel in your body, it’s where it’s going to go and it has an ACE2 receptor on that blood vessel. That’s where it can go because that’s the purpose of the spike protein — to penetrate, to hijack that ACE2 receptor and get into their cells.”
• Spike protein results in different adverse health events down the line — Once spike protein enters your body, that’s when different complications arise, depending on the tissues affected. According to Soon-Shiong:
“That’s why it gets in the pancreas. That’s why you have brain fog. It disrupts the blood vessels of the brain and causes mitochondrial dysfunction. It’s why in the colon, which is high in the GI tract, is a high ACE2 receptor [organ].
That’s why pancreas has a high ACE2 receptor where — that’s why you people have in the heart — you have dysfunction, you, you’ve seen young people have sudden heart attacks.”
• Viruses have caused cancer in other contexts — Hepatitis leads to liver cancer, while HPV can spark cervical and throat cancers. A suppressed immune system cannot remove these intruders. That same risk appears in the post-COVID era.
Individuals with persistent inflammation are more likely to see T-cells go dormant, as Soon-Shiong described. The body basically loses its first responders against malignant transformation, whether the intruder is an outside virus or a mutated cell from within.
In the interview, Soon-Shiong goes deeper into the topic of cancers stemming from viruses due to inflammation, so I highly recommend listening to the whole thing. He concludes:
“What we know about virally induced cancers is well established. We know that if you get hepatitis, you get liver cancer. Hepatitis is a virus infection. We know if you get human papillomavirus, HPV, you get cervical cancer … If you get HIV, you get Kaposi sarcoma …
We call that oncogenic viruses in medical terms, meaning viruses that are … carcinogenic. And the fundamental basis for that are threefold. The hallmarks of our oncogenic virus is one; it must persist.
And why? Because it continues to create inflammation. And … with inflammation you get suppression because your body’s trying to suppress it. It must inhibit the thing called P53 that’s in your body to try and protect your body from … cancer. And if it persists and causes inflammation and, and [it] inhibits P53, it begins to have the hallmarks of an oncogenic virus.”

Save This Article for Later – Get the PDF Now
Your Immune System Is the Foundational Pillar Against Cancer
A typical complete blood count (CBC) includes measurements of white blood cells. However, many oncologists rarely track T-lymphocyte or NK-cell counts unless something extreme surfaces. That omission frustrates Soon-Shiong.
• Your immune system is key to fighting cancer — Soon-Shiong notes that T-cells and NK cells handle the main job of seeking and destroying aberrant cells. If those protective warriors vanish, standard treatments may buy time, but fail in the end.
“It’s … job is to kill … anything that threatens the body, whether you, the body has infection, if you have TB, you have HIV, if you have hepatitis, you have COVID. These cells are there to recognize these infected cells and kill it.
As you and I are sitting here today, our stem cells are growing in order to replenish parts of your body, your heart, you, if you didn’t have that, you wouldn’t have a heart at the age of 14. You need those stem cells. But mathematically, there are some cells that are transformed and your body recognizes that through these natural killer cells and kills it,” he says.
• Immune system cells protect your body from tumor growth — In Soon-Shiong’s words, your immune system cells are “nature’s first responder.” He continues:
“That’s how we are all protected, and we are [in] the state of equilibrium or balance. On the other hand, the moment either the tumor finds a way to hide from these cells, or your body’s, or the tumor causes these cells to be suppressed.
And that’s why I call this the suppressor cells. And there are certain cells in your body called Treg cells or myeloid-derived suppressor cells … that, when they get upregulated, you’ve lost your protection.
And so, the question then is, how do we understand this balance? How do we increase the killers and how do we decrease the suppressors?”
• Traditional cancer treatments only provide short-term results — Chemotherapy and radiation, which often crush immune cells, produce a short remission in many. “But then, so often you watch it roaring back,” Soon-Shiong says.
That’s because the protective cells died along with the original tumor. The correct approach, he says, involves subtle stress on the tumor to expose it, followed by immunological activation to finish the job.
• Teach your own body to create a “bioshield” — Soon-Shiong references a product he’s currently developing called “BioShield.” While it is injected into your body, it’s not a vaccine, but rather a training mechanism for your immune system cells, which will help purge cancer cells from your body. He explains:
“A tumor has molecules that is foreign to the rest of your body. And if you educate your T-cell, you recognize as molecules that is foreign to the rest of your body that T-cell can remember. Now you have a memory T-cell … We now have bladder cancer patients who have lost their bladder in complete remission for nine years …”
While BioShield looks promising, it’s unlikely to be a magic bullet against cancer. That’s why Soon-Shiong stresses that cancer is all about your immune system. If your immune system is in top shape, your risk for cancer will be significantly reduced.
Practical Ways to Strengthen Your Body’s Defenses
To lower your cancer risk, start addressing what’s weakening your immune system in the first place. Inflammation, toxins, stress, poor food choices, and lack of sleep aren’t just small issues — they are the main reasons why your body fails to spot and destroy cancer cells. Here are my recommendations:
1. Clean up your diet and eat more whole foods — If you constantly rely on frozen dinners, fast food, or packaged snacks, it’s time to shift. Aside from being nutritionally lacking, these are loaded with dyes, additives, and inflammatory vegetable oils that confuse your immune system.
Swap them out with fresh produce, grass fed meats, and whole ingredients you recognize. Cook meals at home and store them in glass or stainless steel instead of plastic.
2. Cut your exposure to harmful chemicals — If you are a parent, office worker, or anyone constantly touching printed receipts, using fragranced cleaners, or microwaving in plastic, you are surrounded by chemicals that disrupt your immune cells. These chemicals don’t just sit on the surface — they enter your bloodstream and quietly weaken your immune defenses.
3. Spend enough time outdoors and get sufficient high-quality sleep — If your schedule has you staying up late, glued to screens, or skipping daylight, your immune system isn’t recharging.
Go outside each morning for natural light — it resets your body clock. Sleep at the same time each night in a cool, dark room for seven to nine hours at a consistent schedule. Even missing just an hour or two of deep sleep affects your immune system’s ability to function at its best.
4. Don’t get the COVID shot — If you already got the shot, don’t get any more boosters or mRNA gene therapy shots. Following this strategy immediately ends the assault on your body. But if you’ve already developed a shot-related injury, the next section contains more in-depth tips.
Other Strategies to Help Address COVID-Related Injuries
If you or a family member is suffering from long COVID or adverse effects from the shot, know that there is still hope for recovery.
• Protect your health with these protocols — I recommend you go over the I-RECOVER program by the Front Line COVID-19 Critical Care Alliance (FLCCC). It provides extensive information about how to treat long COVID2 and post-vaccine injuries.3
• Get rid of electromagnetic fields (EMFs) in your home — In addition to the measures discussed by the FLCCC, I recommend reducing your EMF exposure in your home. Research has shown that manmade sources, such as your Wi-Fi router and 5G towers “can disturb the homeostasis of free radicals leading to dysfunctions such as the ‘cellular stress response.'”4
• Minimize linoleic acid (LA) intake — Your fat intake matters because your mitochondria contain cardiolipin, which influences mitophagy and overall mitochondrial quality control.
To promote proper cardiolipin function, boosting omega-3 fat intake is important while simultaneously cutting back on omega-6 fat. However, don’t make the mistake of eating too much omega-3, as eventually it will cause the same damage as eating too much omega-6. For a more detailed explanation on this balance, read “Linoleic Acid — The Most Destructive Ingredient in Your Diet.”
• Optimize your vitamin D level — This nutrient plays an important role in supporting your immune system. Research shows that low vitamin D levels are linked to an increased risk of cancers.5 Vitamin D attaches to the vitamin D receptor in your cells, creating a cascade of signals that affect how cancer cells grow, develop, and survive.6 Studies have also confirmed that vitamin D helps prevent respiratory infections, including COVID-19.
I recommend raising your vitamin D level to a range between 60 ng/mL and 80 ng/mL. To know if you’re hitting that range, you need to get tested. For more information about the benefits of vitamin D for cancer, as well as tips on how to optimize it properly, read “More Evidence Showing Vitamin D Combats Cancer.”
Frequently Asked Questions About the Immune System and Cancer
Q: Why is cancer affecting younger people more than before?
A: According to Dr. Patrick Soon-Shiong, the increase in cancer cases among children and young adults is a result of immune system damage caused by chronic inflammation, poor diet, environmental toxins, and lingering effects from COVID-19 infections or shots. These cases often involve rapidly progressing “turbocharged” tumors that behave more aggressively than traditional cancers.
Q: What role does inflammation play in the development of cancer?
A: Inflammation is central to cancer’s progression. Chronic inflammation suppresses key tumor-suppressing proteins like P53 and compromises the immune system’s ability to eliminate cancerous cells. This persistent immune activation, sometimes from viral proteins like the COVID-19 spike protein, allows malignant cells to thrive by weakening the body’s natural defense mechanisms like T-cells and natural killer (NK) cells produced by your immune system.
Q: How do diet and environmental toxins increase cancer risk?
A: Modern diets high in ultraprocessed foods, refined sugars, and vegetable oils (like canola and soy) disrupt gut health and fuel systemic inflammation. Simultaneously, everyday exposure to manmade chemicals such as “forever chemicals,” food dyes, pesticides, and microplastics overwhelm the immune system. This perfect storm of poor nutrition and hidden toxins suppress immune cells, allowing tumors to escape detection and grow unchecked.
Q: How is COVID-19 linked to rising cancer risks?
A: Soon-Shiong theorizes that both COVID-19 infections and shots contribute to persistent inflammation and immune dysfunction. The virus (or spike protein from the vaccine) enters cells via ACE2 receptors found throughout the body — including the heart, brain, and pancreas — and disrupt mitochondrial function. Over time, this leads to increased risk of cancer.
Q: What strategies can strengthen the immune system and lower cancer risk?
A: Key strategies include:
• Eating whole, unprocessed foods to reduce inflammation
• Avoiding harmful chemicals in plastics, printed receipts, and fragranced products
• Improving sleep and natural light exposure to support immune regulation
• Reconsidering COVID-19 boosters, especially for those experiencing adverse effects
- 1 YouTube, The Tucker Carlson Show, March 27, 2025
- 2 FLCCC Alliance, Long COVID Treatment
- 3 FLCCC Alliance, Post-Vaccine Treatment Guide
- 4 Int J Mol Sci. 2020 Nov; 21(21): 8031, Role of CL in Mitochondrial Quality Control
- 5 The Journal of Steroid Biochemistry and Molecular Biology July 2023, Volume 231, 106308
- 6 Ageing Research Reviews June 2023, Volume 87, 101923, Introduction
The Impact of Vitamin D Supplementation on Your Blood Pressure
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/05/20/vitamin-d-supplementation-and-blood-pressure.aspx
Analysis by Dr. Joseph Mercola May 20, 2025

Story at-a-glance
- Research shows that optimizing your vitamin D level can lower systolic blood pressure within weeks
- People with low vitamin D levels saw the most dramatic improvements, making testing your level a smart first step if you struggle with high blood pressure
- Vitamin D helps lower blood pressure by reducing fluid retention and relaxing blood vessels
- Taking vitamin D alongside magnesium and vitamin K2 increases its effectiveness and reduces the dose needed to reach optimal levels
- Have your vitamin D level checked to establish a baseline. From there, you’ll be able to determine whether you need more sunlight exposure or need to take an oral supplement
More than 122 million American adults — nearly half — have high blood pressure (hypertension).1 Left untreated, hypertension dramatically increases your risk of stroke, heart failure, kidney failure, and sudden death, so it’s not an exaggeration to say that high blood pressure is one of the most dangerous and most overlooked conditions you can face. Early signs include headaches, dizziness, shortness of breath, or no symptoms at all — which is why it’s often called the “silent killer.”
Once diagnosed, most people are put on a lifetime prescription of medications, with little to no discussion of underlying causes or lifestyle-based solutions. However, new research has shown that optimizing your vitamin D level offers hope, even if you haven’t changed other contributing factors, such as your diet. This revelation offers immediate relief for people looking to address their blood pressure without suffering from the side effects of blood pressure medications.
Vitamin D Supplementation Slashes Blood Pressure
A meta-analysis published in Cureus analyzed how vitamin D supplementation impacts blood pressure in adults across a wide range of clinical settings and populations.2 The researchers selected 12 studies from all around the world, spanning countries such as the United States, China, Iran, Denmark, and Australia.
For the analysis, the team looked at changes in both systolic and diastolic blood pressure after vitamin D supplementation. Most of the participants were adults dealing with either high blood pressure or borderline hypertension — not already on medication for more serious conditions, but at enough risk to warrant intervention. Some were vitamin D deficient at baseline, while others had suboptimal but not deficient levels.
• High-dose vitamin D creates rapid results in a short span — In one of the reviewed studies, subjects took 50,000 IU of vitamin D per week for just eight weeks. The results were remarkable — systolic blood pressure dropped by 28.44 mmHg, and diastolic pressure fell by 7.38 mmHg.
“This finding suggests that high-dose supplementation over a short duration may yield greater blood pressure reductions, potentially due to the rapid correction of vitamin D deficiency,” the researchers said.
• Other studies saw more modest improvements, depending on the dose and duration — For example, one study wherein participants were given 1,200 IU per day for eight weeks still saw a drop in systolic pressure by 4.5 mmHg.
In another study, using only 200 IU daily for 16 weeks, researchers reported a 3.4 mmHg drop in systolic pressure and a 2.6 mmHg drop in diastolic pressure. Although smaller, these changes are still profound, especially in those with early-stage hypertension. According to the researchers, some of these shifts occurred even without changes to diet or exercise, showing the direct role vitamin D plays in blood pressure regulation.
• High weekly doses worked faster and produced greater results than lower daily doses spread over months — For instance, the study that administered 50,000 IU per week not only produced the biggest reductions, but did so in just two months.
In contrast, trials that stretched out over 24 to 48 weeks and used smaller doses (like 2,000 to 4,000 IU/day) resulted in blood pressure reductions closer to 1 to 4 mmHg. The results weren’t uniform, but the pattern was clear.
• Results vary, but deficient participants benefited the most — In these individuals, correcting vitamin D deficiency triggered rapid, noticeable improvements in both systolic and diastolic pressure. This reinforces the importance of testing your vitamin D level.
Researchers also pointed out the wide range in outcomes, noting that studies with similar doses produced very different effects depending on the starting health status of the participants. For example, one study gave 4,000 IU/day for 48 weeks and saw almost no change, while another used the same dose over 24 weeks and saw a clear 4 mmHg drop in systolic pressure.
What Happens to Your Body When You Take a Vitamin D Supplement?
One key mechanism has to do with how vitamin D affects the renin-angiotensin-aldosterone system (RAAS). This system controls how much fluid your kidneys retain and how tightly your blood vessels constrict.
When vitamin D is low, RAAS tends to be overactive, leading to more fluid retention, higher vascular resistance, and elevated blood pressure. The review found evidence that vitamin D helps suppress renin, which then lowers the activity of angiotensin II, a hormone that causes blood vessels to tighten up.
• Vitamin D supports blood pressure by improving endothelial function — The endothelium is the lining of your blood vessels. When it’s healthy, your vessels expand and contract easily. When it’s damaged, they stiffen, and that raises blood pressure.
Vitamin D also increases the production of nitric oxide, a molecule that helps blood vessels relax as well as reduces oxidative stress. Over time, this prevents stiffening of the arteries and supports better blood flow.
• Chronic inflammation is regulated — Many of the participants in the reviewed studies had markers of inflammation, either due to obesity, hypertension, or metabolic syndrome. In the context of the study, the researchers noted that vitamin D reduces levels of interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), two cytokines known to worsen vascular inflammation.
Taken altogether, the study provides insight into the importance of maintaining proper vitamin D levels, and what can happen to your health if you don’t have enough of it. While the researchers looked into supplementation, you actually don’t have to spend a single cent to optimize your vitamin D levels — sunlight exposure may be enough, provided you live in a sunny enough locale.

Save This Article for Later – Get the PDF Now
How to Optimize Your Vitamin D Level
If you notice your blood pressure creeping up, or if you’re already on medication and wondering why it’s not fully working, take a look at your vitamin D level. Here are my recommendations to get your health on the right path again:
1. Sensible sunlight exposure is the best way to optimize your vitamin D — The ideal way to optimize your vitamin D levels is via safe sun exposure. Harnessing the sun’s power for vitamin D production offers benefits far exceeding simple vitamin synthesis. However, if your diet includes significant amounts of seed oils, extra caution is warranted.
These oils, rich in linoleic acid (LA), an omega-6 fatty acid, readily oxidize under UV light. This interaction on your skin initiates a cascade of breakdown products, leading to inflammation and DNA damage.
Ideally, reduce consumption of these oils for four to six months before increasing sun exposure. During this time, limiting time in the sun to early morning or late afternoon is recommended. Avoid direct sunlight during peak hours (10 a.m. to 4 p.m.) until your body has cleared the seed oils. Individual factors like skin pigmentation and body composition also influence safe sun exposure.
Those with darker skin tones require longer exposure to generate the same amount of vitamin D as those with lighter skin. Since body fat stores LA, individuals with higher body fat percentages should also exercise additional caution, as those stored oils prolong the risk period even after dietary changes.
To determine safe sun exposure, use the “sunburn test.” Monitor your skin for any redness. Staying below the threshold of even slight pinkness indicates you’re within safe limits. Avoid sunburn at all costs.
2. Take high-quality vitamin D3 if necessary — For individuals living in northern climates or those with limited sun exposure, supplementing with high-quality vitamin D3 is often necessary to achieve and maintain optimal vitamin D levels. Vitamin D3 is synthesized naturally in your skin when it’s exposed to sunlight, specifically ultraviolet B (UVB) rays.
On the other hand, vitamin D2 is typically derived from plant sources, including yeast and mushrooms exposed to UV light. While both forms are available as supplements, research has uncovered distinct differences in their effectiveness. Vitamin D3 is significantly more effective than D2 at raising blood vitamin D levels.3
3. Take your vitamin D with magnesium and vitamin K2 — If you take supplemental vitamin D3, you also need to be mindful of taking extra vitamin K2 and magnesium. It’s important to increase your vitamin K2 intake when taking high-dose supplemental vitamin D to avoid complications associated with excessive arterial calcification.
You need 146% more vitamin D to achieve a blood level of 40 ng/mL (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
Vitamin D improves magnesium absorption, but taking large doses of vitamin D can deplete magnesium, as magnesium is required in the conversion of vitamin D into its active form. Combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually. You need 244% more oral vitamin D if you’re not concomitantly taking magnesium and vitamin K2.
4. Take your supplements with a bit of healthy — Both vitamin D and K2 are fat-soluble nutrients, which means they require fat to get into your system effectively. However, the type of fat matters.
If you’re still eating food high in vegetable oils — like soybean, canola, or even too much olive oil — you’re flooding your cells with linoleic acid (LA), which damages how your mitochondria process light and nutrients. Switch to grass fed butter, tallow, or ghee instead. I recommend reducing your LA intake to less than 5 grams per day, but don’t go overboard with healthy fat, either. Carbohydrates are still your body’s preferred fuel — not fat.
Additional Guidelines for Safe Sun Exposure
When you begin getting regular sun exposure, use this simple safety test — watch your skin for the first sign of pinkness, which is an early warning of sunburn. Stop sun exposure before your skin turns pink to prevent damage. This pinkness threshold helps you determine your safe exposure time.
Now, what if you need to spend time under the sun but haven’t completely removed LA from your body yet? Here are some protective strategies I recommend:
• Take 12 milligrams of astaxanthin daily to enhance your skin’s UV resistance.
• Apply topical niacinamide (vitamin B3) cream before sun exposure to protect against UV-induced DNA damage.
• Take a baby aspirin 30 to 60 minutes before sun exposure to help prevent LA conversion to harmful oxidized linoleic acid metabolites (OXLAMs).
• Use molecular hydrogen supplements to combat oxidative stress.
Check Your Vitamin D Levels Regularly
For optimal health, you’ll want to aim for a vitamin D level between 60 ng/mL and 80 ng/mL. The minimum cut off for sufficiency is 40 ng/mL to 60 ng/mL.
I’ve published a comprehensive vitamin D report in which I detail vitamin D’s mechanisms of action and how to ensure optimal levels. I recommend downloading and sharing that report with everyone you know. A quick summary of the key steps is as follows:
1. First, establish your baseline — Once you know what your current blood level is, you can assess the dose needed to maintain or raise it. If you cannot get enough vitamin D from the sun (you can use the DMinder app4 to see how much vitamin D your body can make depending on your location and other individual factors), then you’ll need an oral supplement.
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.
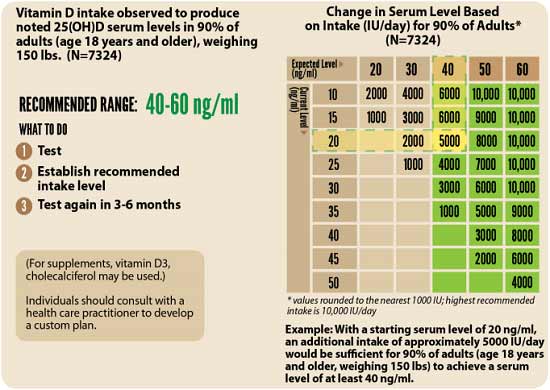
3. Retest in three to six months — Lastly, have your vitamin D level retested in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
Frequently Asked Questions About Vitamin D and Its Impact on Blood Pressure
Q: Why is high blood pressure often called the silent killer?
A: High blood pressure (hypertension) affects around half of U.S. adults. It often shows no symptoms for years, quietly damaging vital organs like the heart, kidneys, brain, and eyes. If left untreated, it leads to stroke, heart failure, kidney failure, and even sudden death, making it one of the most dangerous and overlooked health conditions.
Q: Can vitamin D supplementation help lower blood pressure?
A: Yes. Research revealed that high-dose vitamin D supplementation reduces blood pressure within weeks. Even smaller daily doses showed modest but significant drops. The benefit was most noticeable in people who were vitamin D deficient to begin with.
Q: How does vitamin D influence blood pressure levels?
A: Vitamin D helps regulate the renin-angiotensin-aldosterone system (RAAS), which controls blood vessel constriction and fluid retention. It also enhances nitric oxide production, helping vessels relax. Moreover, it reduces oxidative stress and vascular inflammation and lowers levels of inflammatory markers like IL-6 and TNF-alpha.
Q: What’s the best way to optimize my vitamin D levels naturally and safely?
A: Start with smart sun exposure — aim for 15 to 30 minutes of midday sunlight on bare skin without sunscreen, but only if you’ve purged your body of vegetable oils for at least six months. If you’re just working to removing these oils, avoid peak sunlight hours to protect your skin.
Q: How should I monitor and adjust my vitamin D levels?
A: Regular testing is key. Aim for blood levels between 60 ng/mL and 80 ng/mL for optimal health. The steps below summarize the process:
1. Test your vitamin D level.
2. Use GrassrootsHealth’s Vitamin D*calculator to determine your proper dose.
3. Retest every three to six months to track and fine-tune your approach. Apps like DMinder can help estimate vitamin D synthesis from sun exposure based on your location and lifestyle.

