Iron
now browsing by category
How Dietary Copper Affects Memory Loss and Brain Aging
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/09/10/copper-and-brain-health.aspx
Analysis by Dr. Joseph Mercola September 10, 2025

Story at-a-glance
- Older adults who consumed between 1.2 and 1.6 milligrams of copper daily scored higher on memory and processing speed tests, with stroke survivors benefiting the most
- Higher copper levels in specific brain regions were linked to slower cognitive decline and fewer Alzheimer’s-related changes
- A high-fat diet combined with high copper intake more than doubled the rate of memory loss, especially in language and verbal recall skills
- Copper regulates enzymes that protect brain cells from oxidative stress and helps shift brain immune cells into a healing state after injury
- Whole foods like grass fed beef liver, bee pollen, and shiitake mushrooms support copper balance, while strategic supplementation with copper bisglycinate helps restore levels in those with deficiency
Your brain runs on a delicate balance of minerals — and copper is one of the most important. It’s easy to overlook, but this trace nutrient controls the very processes that keep your mind sharp: how your neurons fire, how your brain makes energy, and how it clears out damaging waste. Without enough, systems start breaking down. You don’t think as clearly. Your memory slips. And your brain begins to age faster than it should.
What makes copper unique is that it’s both necessary and dangerous in the wrong context. Too little leaves your brain vulnerable to oxidative stress. Too much, and it becomes part of the problem — fueling inflammation and structural damage. That tightrope makes copper one of the most powerful, yet high-stakes, nutrients in your diet.
Most people aren’t thinking about copper when they eat. But what you’re eating — or not eating — could be shifting your copper balance in a way that accelerates cognitive aging without you realizing it. That’s why I want to show you what scientists are now uncovering about copper’s impact on your brain, and how dialing it in — not too much, not too little — is one of the simplest ways to sharpen your memory and protect long-term brain health.
Better Brain Function Seen with Daily Copper
A study published in Scientific Reports analyzed data from 2,420 American adults over age 60 to evaluate how dietary copper influences cognitive function.1 Using data from the National Health and Nutrition Examination Survey (NHANES) between 2011 and 2014, researchers reviewed both diet and memory test scores. Their goal was to determine whether eating more copper-rich foods translated into better brain performance.
• Older adults who consumed more copper scored higher on multiple brain tests — Participants who consumed the most copper — around 1.2 to 1.6 milligrams (mg) per day — consistently scored better on tests measuring memory, language, and processing speed. The relationship held even after adjusting for confounding factors like age, education, calorie intake, and levels of other minerals such as zinc, iron, and selenium.
• The strongest cognitive gains occurred below a specific threshold — Results followed a clear non-linear pattern. When copper intake reached about 1.2 to 1.6 mg per day, cognitive scores improved. But beyond that point, the benefits leveled off.
• Cognitive benefits were greatest in stroke survivors — Among participants with a history of stroke, the effect of copper was even more pronounced. Those in the highest copper intake group had significantly higher global cognition scores than those with the lowest intake. This suggests that copper intake is especially important for neurological recovery and brain resilience after a vascular event.
• Copper’s role in brain recovery likely involves antioxidant and energy enzymes — The study explained that copper serves as a cofactor for key enzymes like superoxide dismutase (SOD1), which neutralizes reactive oxygen species in brain cells. This action helps prevent oxidative damage — one of the main drivers of neuron death in aging brains. When copper intake falls below the optimal range, SOD1 activity drops, and damage from free radicals increases.
• Copper impacts neuroinflammation and brain cell repair — Researchers also noted copper’s influence on immune cells in the brain. Specifically, copper appears to reduce inflammation after a stroke by shifting microglia — the brain’s immune cells — from a damaging “M1” mode to a healing “M2” state. This transition lowers inflammatory cytokines, while boosting anti-inflammatory molecules.
Higher Brain Copper Linked to Slower Memory Loss and Less Alzheimer’s Damage
Published in the journal Molecular Psychiatry, this community-based study followed 657 older adults for nearly seven years before death and analyzed copper levels in four brain regions during autopsy.2 Researchers wanted to know whether brain copper levels were linked to how quickly memory declined and how much Alzheimer’s disease damage was found after death. They also tracked participants’ dietary copper intake to see if it influenced copper levels in the brain or disease severity.
• Participants with more brain copper declined more slowly and had fewer signs of Alzheimer’s — Higher copper levels in specific areas of the brain, particularly the inferior temporal and mid-frontal regions, were strongly associated with slower loss of memory, attention, and thinking speed over time. Those in the top third for brain copper experienced the slowest decline in global cognition and key memory domains.
• Memory and processing speed were the most improved cognitive areas — The biggest differences were seen in global cognition, working memory, semantic memory (understanding words and meanings), and perceptual speed (how quickly the brain processes information). Participants in the top copper group declined 0.03 units per year more slowly than those in the lowest group — small differences that add up over time.
• Higher brain copper was linked to lower odds of advanced Alzheimer’s stage — Participants with the most brain copper had 40% lower odds of being in the most severe stage of Alzheimer’s pathology compared to those with the lowest copper.
• Copper plays a key role in maintaining healthy brain structure and function — Copper is used by enzymes that support brain energy metabolism, gene regulation, antioxidant defense, and neurotransmitter synthesis. These enzymes protect neurons from oxidative stress, regulate iron, and help with signal transmission between brain cells. A copper shortfall weakens these defenses, leaving neurons more vulnerable to damage.

Save This Article for Later – Get the PDF Now
A High-Copper, High-Fat Diet Raises Dementia Risk
Copper is essential for brain health, but having too much also leads to neurodegeneration and neurological disorders. In an analysis published in the American Journal of Epidemiology, researchers tracked 10,269 middle-aged adults over a 20-year period to examine how dietary copper intake — especially when combined with high levels of saturated fat — affected cognitive performance and dementia risk.3
• Copper wasn’t a risk factor until paired with high-fat diets — Among those who consumed the most saturated fat, higher copper intake was linked to significantly faster cognitive decline. In this group, high copper doubled the rate of memory loss. In contrast, people with low saturated fat intake showed no negative effect from copper, even at higher doses. This interaction highlights how nutrients don’t act in isolation. Your overall dietary pattern matters.
• Verbal memory suffered the most in those with high copper and fat intake — The largest decline was seen in language-related skills. Participants with high copper and high saturated fat diets had the steepest drop in word recall and verbal fluency. These are early warning signs of dementia, especially Alzheimer’s-type cognitive impairment.
• Supplements weren’t the issue — most copper came from food — The researchers confirmed that nearly all copper came from dietary sources. Supplement users made up a small minority and didn’t skew the data. This underscores the need to evaluate food combinations, not just isolated nutrient doses.
• Brain damage likely driven by copper-induced oxidation of fats — The study authors proposed that excess copper oxidizes saturated fats and cholesterol in the bloodstream, triggering inflammatory damage inside the brain. When fats are oxidized, they form harmful compounds called aldehydes, which are known to impair neurons and increase beta-amyloid buildup, a hallmark of Alzheimer’s disease. This damage appears to be especially aggressive in brain regions responsible for memory.
• Related study found participants with the highest copper and saturated/trans fat intake had the worst cognitive outcomes — A study published in Archives of Neurology found that in people with diets high in saturated and trans fats, higher copper intake was linked to a dramatic decline in mental function.4 Their rate of cognitive decline was equivalent to aging 19 years faster compared to participants with low copper and low fat intake.
That means a 65-year-old on a high copper, high-fat diet had the brain function of an 84-year-old. The study found no such effect among those with high copper but low fat intake, showing it was the combination — not copper alone — that accelerated damage.
How to Balance Copper and Protect Your Brain from Cognitive Decline
Copper is one of the most misunderstood minerals in your body. While the mainstream narrative often warns about copper excess, the reality is that most people are walking around copper-deficient — and that has far-reaching consequences for your brain. Copper is foundational for mitochondrial function, iron regulation, and energy production. When it’s low, iron builds up in places it shouldn’t, oxidative stress spikes, and your neurons suffer.
If you’re feeling mentally sluggish, forgetful, or easily fatigued, your copper status may be off. But rather than guessing, I recommend a strategic approach that supports your body’s ability to regulate copper naturally — using whole foods, metabolic support, and, if needed, supplementation. Here are five key steps to optimize your copper levels and protect your brain:
1. Add copper-rich whole foods to your diet — Foods like grass fed beef liver, shellfish, shiitake mushrooms, dark chocolate, and bee pollen are some of the best sources of bioavailable copper. These foods don’t just supply copper — they deliver it in a way your body knows how to handle. Retinol (preformed vitamin A), found in beef liver and organ meats, plays a direct role in copper metabolism. Without enough retinol, copper can’t get where it needs to go.
2. Shift your macronutrient balance — more carbs, less fat — A high-fat diet disrupts how your body burns glucose and instead forces it to rely on fat for energy. That imbalance drives chronic disease. I now recommend keeping fat intake between 30% and 40% of your daily calories.
That means prioritizing healthy, digestible carbs like whole fruit, cooked root vegetables, white rice, and small amounts of well-tolerated whole grains, as long as your gut is healthy and you tolerate them. For healthy fats, focus on grass fed butter, ghee and tallow, while minimizing the polyunsaturated fat linoleic acid in vegetable oil.
3. Supplement strategically with copper bisglycinate if needed — If your copper intake is low or you’ve been dealing with signs of deficiency, such as brain fog or unexplained fatigue, consider taking 3 to 4 mg of copper bisglycinate daily. This chelated form is highly absorbable and less likely to irritate your gut. But don’t supplement blindly — test your levels, track your progress and adjust your copper intake as needed.
4. Balance copper and iron — It’s important to recognize the interplay between iron and copper. Iron overload coupled with copper deficiency presents a particularly risky scenario. Copper deficiency is widespread, and many individuals require increased copper intake to support proper iron metabolism.
Balanced copper levels aren’t just about brain performance — they’re about restoring the mineral harmony that drives every system in your body. When copper is where it’s supposed to be, your energy, memory, and clarity come back online.
FAQs About Copper and Your Brain
Q: What does copper do for your brain?
A: Copper is essential for your brain’s electrical activity, antioxidant defense, and energy production. It activates enzymes like superoxide dismutase, which neutralize free radicals and protect neurons from damage. Without enough copper, your brain cells can’t generate energy efficiently or repair oxidative injury, leading to memory problems and cognitive decline.
Q: Can eating more copper-rich foods really improve memory?
A: Yes. Research published in Scientific Reports found that adults over 60 who consumed about 1.2 to 1.6 mg of copper daily had better memory, language skills, and processing speed — especially those recovering from stroke.5 Another study in Molecular Psychiatry showed that higher copper levels in brain tissue were linked to slower cognitive decline and less Alzheimer’s pathology.6
Q: Is too much copper dangerous for your brain?
A: It can be. While copper is necessary, too much — especially when paired with a high-fat diet — fuels oxidative stress. A study in the American Journal of Epidemiology found that high copper intake doubled the rate of memory loss in people eating diets rich in saturated fat.7 The damage is likely caused by copper oxidizing fats in the blood, triggering brain inflammation and beta-amyloid buildup.
Q: What foods help regulate healthy copper levels?
A: Grass fed beef liver, shellfish, shiitake mushrooms, dark chocolate, and bee pollen are excellent sources. Retinol (vitamin A) from organ meats is also needed to direct copper into your cells and prevent accumulation in the wrong places.
Q: Should I take a copper supplement?
A: If your diet lacks copper or you’re showing signs of deficiency, such as fatigue or brain fog, it may help to take 3 to 4 mg of copper bisglycinate daily. This form is gentle on digestion and highly absorbable. However, food-based copper should typically come first.
More Evidence That High Iron in the Brain Promotes Alzheimer’s
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/08/19/brain-iron-and-alzheimers-disease.aspx
Analysis by Dr. Joseph Mercola August 19, 2025
Story at-a-glance
- New research shows excess iron in your brain triggers damage that accelerates Alzheimer’s, especially in people with Down syndrome, who develop the disease earlier and more aggressively
- Too much iron damages the outer layer of brain cells, weakens your brain’s natural protectors like glutathione, and encourages the buildup of plaques that destroy nerve cells and harm memory
- Tiny, often undetected brain bleeds are a major source of iron overload, leaking iron-rich compounds into brain tissue that fuel long-term inflammation and cellular breakdown
- Key brain enzymes meant to protect against iron damage are missing in the exact areas being attacked, leaving neurons highly vulnerable even when overall antioxidant levels appear normal
- You can reduce your risk by testing your ferritin and GGT levels, donating blood if iron is high, increasing copper and calcium from food, eliminating vegetable oils, and restoring glutathione with molecular hydrogen and sulfur-rich foods
Alzheimer’s doesn’t start with forgetfulness — it starts with damage. Long before memory loss appears, your brain begins breaking down at the cellular level. And one of the hidden drivers behind that destruction is something many people don’t think about: iron.
When iron builds up in your brain tissue and reacts with fats and proteins, it causes oxidative stress that destroys neurons from the inside out. This iron-driven process doesn’t just accompany Alzheimer’s — it could be what kicks it into gear. A study from the University of Southern California and the University of California, Irvine uncovered a key clue: people with Down syndrome who develop Alzheimer’s show far more brain iron than those with Alzheimer’s alone.1
That excess iron is tied to brain cell death, inflammation, and early buildup of harmful plaques. If your body can’t safely store and regulate iron, the damage spreads fast — especially in areas tied to memory and executive function. And once your antioxidant defenses are overwhelmed, there’s little left to stop the cascade. Understanding how and why this happens opens the door to new strategies — not just for slowing Alzheimer’s, but for preventing it before it takes hold.
Too Much Iron in Your Brain Speeds Up Alzheimer’s Damage
The study, published in Alzheimer’s & Dementia, looked at how too much iron in your brain drives Alzheimer’s disease, especially in people with both Down syndrome and Alzheimer’s.2 Researchers studied brain tissue from three groups: healthy adults, adults with Alzheimer’s, and adults with Alzheimer’s related to Down syndrome. Their goal was to understand how iron buildup harms brain cells and leads to sticky protein clumps called amyloid plaques, which are tied to Alzheimer’s.
• Iron levels were much higher in people with both Down syndrome and Alzheimer’s — Compared to healthy adults and those with Alzheimer’s alone, people who had both conditions had about twice as much iron in a key brain region responsible for memory and decision-making.
This group had much higher levels of damage from iron reacting with the fats in brain cells and breaking them down. Making matters worse, the natural defenses that protect brain cells from this type of damage were weakened or missing.
• The brain’s protective enzymes were missing where they were needed most — The study found enzymes that normally repair damage to brain cell membranes were reduced by as much as 70% in the affected areas. These enzymes are important because they help prevent brain cell death triggered by iron overload.
Another protective compound, glutathione, also wasn’t being made properly. That’s because the enzyme needed to make it was also reduced by up to 60%. Without enough glutathione, brain cells lose a major line of defense against stress and oxidation.
• Iron harmed key parts of brain cells that act like control centers — The study found that iron was attacking small areas on the cell’s surface where important proteins are handled and messages are sent. In brains affected by Alzheimer’s — especially in people with Down syndrome — these areas were badly damaged. This damage changed how certain proteins were made, increasing the toxic forms that clump together in the brain and destroy nerve cells.
Are Tiny Brain Bleeds the Source of All That Extra Iron?
One major clue came from the discovery of iron deposits in areas linked to microscopic bleeding. These “microbleeds” are tiny leaks from brain blood vessels that often go unnoticed. When blood escapes into brain tissue, it breaks down and releases iron.
Over time, this creates pockets of stored iron that cause more damage. The study found that a cleanup enzyme, which helps process iron from blood, was three times higher in the brains of people with Down syndrome and Alzheimer’s, suggesting chronic bleeding was driving iron overload.
• The brain’s protein-cutting process turned more destructive under stress — Normally, certain brain proteins can be cut in ways that are either safe or harmful. In the damaged brains, the harmful cutting process became more active — not because there was more of the cutting enzyme, but because it was working faster, likely due to iron-related stress. At the same time, the safer cutting process slowed down. This shift caused the brain to make more toxic proteins instead of removing them.
• Even though the body made more antioxidants, they weren’t in the right place — The brain as a whole seemed to increase antioxidant enzyme levels in response to damage, but those enzymes weren’t where they were most needed. This mismatch meant that cells remained vulnerable to damage, even though the body was trying to defend itself. It showed that Alzheimer’s damage isn’t just about overall inflammation or oxidation — it’s about damage happening in precise, high-risk zones.
• Your genes influence how much iron builds up in your brain — In people with rare forms of Down syndrome who didn’t have an extra copy of a certain protein-making gene, there was far less brain iron, fewer harmful protein clumps, and they lived up to 20 years longer than those with the extra gene. This shows that making too much of that protein leads to more iron buildup, more brain damage, and a shorter life — helping explain why some people’s brains decline faster than others.

Save This Article for Later – Get the PDF Now
How to Protect Your Brain from Iron-Driven Damage
High iron is an under-recognized health threat, and there’s a general lack of awareness in the medical community regarding the health risks associated with high iron levels. If you’re concerned about memory loss or have a family history of Alzheimer’s, it’s time to start thinking about iron — not just in your blood, but in your brain.
The study I’ve shared shows that too much brain iron doesn’t just sit there quietly. It ignites a chain reaction of oxidative stress and cell damage that accelerates cognitive decline. Your first move should be reducing the root cause: excess iron accumulation combined with poor antioxidant defenses. Here’s what I recommend to take control of the iron-oxidation cycle and give your brain the support it needs to stay sharp, focused, and protected.
1. Test your ferritin and gamma-glutamyl transpeptidase (GGT) to assess iron burden and oxidative stress — If you don’t know your ferritin level, that’s where you start. Ferritin is the storage form of iron, and the ideal range is between 60 and 75 ng/mL. High ferritin levels indicate your body is holding onto too much iron, which leaks into your brain and triggers damage.
I also recommend asking for a GGT test. GGT is a key marker of oxidative stress and helps identify if free iron is causing damage inside your body. When both ferritin and GGT are elevated, it’s a strong sign your iron is doing harm.
2. Donate blood or request phlebotomy if your iron is too high — If your body is holding onto more iron than it can safely manage, it increases your risk for heart disease, insulin resistance, and oxidative damage to your organs — including your brain. One of the most effective solutions?
Donate blood two to four times a year. This simple act pulls iron out of storage and lowers your levels gradually. If donation isn’t an option due to your health history, ask for therapeutic phlebotomy to achieve the same result.
3. Balance your copper intake to support healthy iron metabolism — Iron reduction is only one piece of the puzzle. If your copper status is low, which is common, your body can’t regulate iron properly. Copper and iron work together. When copper is deficient, iron builds up in places it doesn’t belong. Consider supplementing with 3 to 4 milligrams of copper bisglycinate daily if your intake is low.
You can also focus on copper-rich foods like bee pollen, grass fed beef liver, and acerola cherries — acerola cherry is very high in vitamin C, which contains copper-rich tyrosinase enzyme. Don’t overlook retinol either — this nutrient, found in beef liver and organ meats, helps your body absorb and use copper effectively.
4. Get calcium from food to help keep iron in check — Proper calcium intake reduces your risk of iron overload naturally. When calcium is low, your body produces more parathyroid hormone, which increases iron storage. That creates a feedback loop that worsens brain inflammation over time.
Focus on getting calcium from whole food sources like raw grass fed dairy, pasture-raised egg yolks, and powdered eggshells. Skip the synthetic calcium supplements unless medically necessary, as they don’t offer the same co-factors for absorption.
5. Remove vegetable oils and increase antioxidant-rich foods — Iron is especially dangerous when it reacts with unstable fats, like polyunsaturated fats in vegetable oils. I recommend eliminating canola, soy, corn, sunflower, safflower, and other vegetable oils from your kitchen. These oils break down in your body and feed oxidative stress.
Replace them with stable fats like grass fed butter, ghee, coconut oil, and tallow. At the same time, boost your antioxidant defenses by eating garlic, onions, and pasture-raised eggs. These foods give your body the building blocks to produce glutathione, your brain’s main defense system against iron-triggered damage.
You can also add molecular hydrogen to your daily routine. Hydrogen activates your body’s own healing system by switching on glutathione — especially important when chronic illness and oxidative stress have shut those systems down. Whether through hydrogen-rich water or tablets, this approach helps reactivate your brain’s defense systems where they’re needed most.
By actively lowering excess iron, restoring mineral balance, and strengthening your antioxidant defenses, you protect your brain from the inside out. These steps are simple, actionable, and backed by clear biological mechanisms. Start with testing, make the dietary swaps, and stay consistent — your future brain will thank you.
FAQs About Iron and Alzheimer’s Disease
Q: What does iron have to do with Alzheimer’s disease?
A: Excess iron in your brain causes oxidative damage by reacting with fats and proteins in brain cells. This process leads to neuron death and helps trigger the development of Alzheimer’s. The damage is especially severe in areas responsible for memory and decision-making.
Q: What did the new study find about brain iron and Alzheimer’s?
A: The study found that individuals with both Down syndrome and Alzheimer’s had double the brain iron compared to those with Alzheimer’s alone. The extra iron was linked to faster and more severe buildup of brain plaques, greater cell damage from stress, and weaker natural protections in the brain.
Q: Where does all this excess iron come from?
A: Tiny, undetected brain bleeds (microbleeds) appear to be a key source. When blood leaks into brain tissue, iron from hemoglobin is released and stored locally, causing long-term oxidative stress. People with Down syndrome-related Alzheimer’s had a threefold increase in the enzyme that processes blood-derived iron, suggesting chronic internal bleeding contributes to iron buildup.
Q: How can I find out if I have high iron levels?
A: Start by testing your ferritin, the storage form of iron. Ideal levels fall between 60 and 75 ng/mL. You should also request a GGT test to measure oxidative stress. High ferritin and GGT together suggest your body is not safely managing iron, which impacts brain health.
Q: What steps can I take to reduce the risk of iron-driven brain damage?
A: Donate blood regularly or ask for therapeutic phlebotomy if your ferritin is high. Balance iron with copper-rich foods or supplements, increase calcium from whole food sources, eliminate vegetable oils, and boost antioxidants like glutathione. You can also use molecular hydrogen to reactivate antioxidant enzymes and help your brain neutralize oxidative stress.
The Importance of Getting Regular Health Tests
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/08/16/importance-of-getting-regular-health-tests.aspx
Analysis by Dr. Joseph Mercola August 16, 2025

Story at-a-glance
- Regular lab testing provides precise, actionable insights that enable early detection of possible diseases to improve long-term health outcomes
- Iron overload testing is crucial since excess iron is more common than deficiency; check serum ferritin levels and GGT enzyme levels for accuracy
- Hormone testing reveals metabolic health by measuring cortisol for stress levels, testosterone for mortality risk, and insulin resistance through HOMA-IR calculations
- Comprehensive biomarker monitoring includes vitamin D levels, complete thyroid panel beyond thyroid-stimulating hormone (TSH), and NAD+ testing for cellular function
- Biannual gut microbiome testing provides insights into bacterial balance, enabling smarter dietary decisions
When was the last time you had a thorough assessment of your health? Guessing about the current state of your health can lead to risky assumptions and dangerous oversights. Without concrete information, symptoms are likely to be misinterpreted or dismissed, allowing underlying issues to progress unnoticed. On the other hand, too much intake of a specific nutrient will also lead to health issues.
Lab testing removes uncertainty by providing precise, actionable insights into your health. By leveraging data-driven results, you gain clarity about your body’s true state, enabling you to select the optimal strategy to boost your health and proactively address concerns. The following are the tests I recommend that you take to keep you updated on what’s happening inside your body.
How to Test for Iron
One good reason why I recommend taking regular tests is to catch an unsuspecting health problem affecting many people — iron overload. In fact, it’s more widespread than iron deficiency. In addition, I’ve also written a paper about the duality of iron as a toxin and a nutrient, which will be published in the future. The recommendations I mention below stem from the findings of that specific research.
• How iron is normally tested — Checking for excess iron is straightforward and starts with a basic serum ferritin test, which shows how much iron your body has stored. This test reveals if your iron storage has reached higher-than-normal levels.
For context, transferrin refers to a protein produced in your liver that transports (hence the “transfer” in the name) iron molecules it binds to, transporting it to tissues. One example is your bone marrow, which requires iron to create new blood cells.1
• Transferrin saturation (TSAT) — While a serum ferritin test is a cornerstone test, it shows an incomplete picture. It works best alongside a TSAT test.
TSAT levels — calculated as serum iron divided by total iron-binding capacity (TIBC) then multiplied by 100 — shows the current amount of transferrin protein that’s bound to iron. Thus, it shows you the current iron levels you have available for erythropoiesis, commonly known as red blood cell production.
• Results to watch out for — When it comes to serum ferritin levels, I believe that the ideal range is between 30 and 100 ng/mL (nanograms per milliliter). This is sufficient for hemoglobin synthesis and avoids iron accumulation that can lead to oxidative stress in your body.

As for TSAT, my research indicates that the ideal range is between 25% and 35%. If regular tests show a range above 35%, you likely have iron overload. At 35% to 40%, iron that isn’t bound by transferrin protein — also known as toxic non-transferrin-bound iron (NTBI) — will damage your vital organs.2 In fact, TSAT ranges between 45% and 55% are linked to a 60% to 67% increase in all-cause mortality.
•Ideal ranges — To summarize, healthy results should show TSAT levels between 25% and 35%, alongside serum ferritin levels between 30 and 100 ng/mL.
Now, if your combined results show TSAT levels below 20% and serum ferritin levels below 15 micrograms per liter (µg/L), you likely have depleted iron reserves. Conversely, TSAT levels above 45% and ferritin levels above 100 ng/mL indicate excess iron. Taken altogether, serum ferritin not only serve as diagnostic markers — they also function as risk predictors.

• Other tests that detect iron — A comprehensive assessment usually includes an iron panel, complete blood count (CBC), gamma-glutamyl transferase (GGT), and a metabolic panel to fully understand your body’s iron status and overall health.
A healthy ferritin level is between 20 and 40 ng/mL. If results show that you’re below 20 ng/mL, you’re deficient in iron, which isn’t what you also want to happen. Conversely, you want your ferritin below 100 ng/mL, which is the maximum cut off.
• GGT test — This refers to the enzyme mainly produced by the liver, and is responsible for breaking down medications and toxins. When too much iron builds up in your body, it can harm your liver cells, causing GGT levels to rise significantly in your bloodstream.
What’s great about this test is that it also gives you insights on your excess free iron, as well as your risk for sudden death, insulin resistance, and cardiometabolic disease. Once you have your results, refer to the table below to know where you stand:
| Ideal GGT Level, units per liter (U/L) | Average level, above which your risk for chronic disease increases significantly | “Normal” GGT Level | |
|---|---|---|---|
| Men | Less than 16 U/L | 25 U/L | Up to 70 U/L |
| Women | Less than 9 U/L | 18 U/L | Up to 45 U/L |
Fine-Tuning Your Lifestyle for Longevity
Testing for possible nutrient deficiencies (or overload) is just one aspect of the big picture. You also need to test for other biomarkers, such as your hormones (testosterone, cortisol, and insulin) to detect your current stress levels. Doing so will lead to better metabolic health management.
• How cortisol is measured — Cortisol is produced by your adrenal glands, and it can be detected via your blood, urine, or saliva. Once samples are provided, be sure to follow your doctor’s instructions to generate the most accurate results possible.3
According to the Cleveland Clinic, cortisol in the blood, urine, or saliva are at their highest during the early morning and then decline afterward — midnight is the lowest point.4
• What your cortisol levels tell you about your health — In addition to measuring your stress levels, cortisol tests help rule out other conditions. For example, Addison’s disease occurs when your body isn’t producing enough cortisol. Conversely, Cushing’s syndrome is marked by high cortisol levels. Tumors are also marked by elevated cortisol.5
Finding out your current cortisol levels is important for overall health. It drastically accelerates aging and even contributes to muscle degradation over time. Lastly, it contributes to inflammation and a weakened immune system.
• The importance of testosterone — In a previous article, I cited research showing the link between sex hormones and mortality risk in men. Basically, if your testosterone levels drop by 213 ng/dL (nanograms per deciliter), you have a higher risk of all-cause mortality. In addition, testosterone levels below 153 ng/dL were associated with increased cardiovascular mortality risk.
• Ideal testosterone range — To find out your current levels, you’ll need to have your blood tested. That said, what’s a healthy range? In this article, I mentioned 300 to 1,000 ng/dL as a baseline.
• Testing for insulin resistance — In addition to cortisol, another crucial test that I recommend you take is measuring your insulin resistance. This is essential because results will serve as warning signs for your metabolic health. That said, insulin resistance is measured via the Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) test. It calculates how your fasting glucose and insulin levels interact, and finds out how your body uses insulin.
• Interpreting HOMA-IR results — Below is a breakdown on how the HOMA-IR test is calculated. A score below 1 means you are currently insulin-sensitive and functioning well. Anything above that means that you currently have insulin resistance.
HOMA-IR = (Fasting Glucose x Fasting Insulin) / 405, where
◦ Fasting glucose is measured in mg/dL
◦ Fasting insulin is measured in μIU/mL (microinternational units per milliliter)
◦ 405 is a constant that normalizes the values
If you’re using mmol/L for glucose instead of mg/dL, the formula changes slightly:
HOMA-IR = (Fasting Glucose x Fasting Insulin) / 22.5, where
◦ Fasting glucose is measured in mmol/L (millimoles per liter)
◦ Fasting insulin is measured in μIU/mL, and
◦ 22.5 is the normalizing factor for this unit of measurement

Save This Article for Later – Get the PDF Now
Testing for Other Important Biomarkers
So far, I’ve covered the importance of having your iron, cortisol, insulin resistance, and testosterone levels tested. While they may seem like a lot, there’s still a few more tests that need to be done.
• Monitor your vitamin D — This nutrient is a crucial contributor to optimal health, and I’ve espoused its importance for many years now. Considering this, a simple blood test is all you need to know your current levels.
My recommended range is between 60 ng/mL and 80 ng/mL, and the cutoff for sufficiency is around 40 ng/mL. Once you’ve confirmed your level, you’ll know how much sun exposure or supplementation (if needed) is necessary for you to reach the ideal range. Then, retest in the next three to four months to make sure you’ve hit your goals.
• Don’t forget your thyroid hormones — Your endocrine system is a complex network of glands and organs that regulate hormone production. Among the many hormones produced in your body, the ones produced in the thyroid are perhaps the most important because they help regulate metabolism and are found in nearly every physiological process within you.
• Understanding thyroid antibodies — Examples include thyroglobulin antibodies (TgAb) and thyroid peroxidase antibodies (TPOAb). Results will give you deeper insight into whether autoimmune processes are attacking your thyroid gland. Pairing these antibody results with symptoms helps you make meaningful connections and clarifies what’s really going on with your body, particularly if you’re dealing with an autoimmune condition.
• Traditional thyroid assessments aren’t effective anymore — Testing for thyroid-stimulating hormone (TSH) alone often misses underlying issues. That’s because TSH levels fluctuate significantly and you’ll even appear relatively normal even when you’re actually experiencing severe symptoms.
For instance, individuals with Hashimoto’s thyroiditis might have completely normal hormone levels yet feel persistently unwell. Similarly, basal body temperature is also an unreliable indicator of thyroid health, as it can be influenced by multiple factors unrelated to thyroid function.
• How to test thyroid function — A full thyroid assessment should show the following results:
◦Low TSH
◦T3 levels in the upper range
◦rT3 levels in the lower range
◦Moderate T4 levels
However, note that even “normal” results will not guarantee that your thyroid is functioning properly. For deeper insight, test for rT3 and cholesterol. Small amounts of rT3 are normal and act as a buffer against thyroid overactivity. On the other end, elevated rT3 is problematic because it competes with T3, reducing your metabolic rate. Elevated cholesterol levels also usually signal suboptimal thyroid function.
Importance of NAD+ Testing
Nicotinamide adenine dinucleotide (NAD+) is an important molecule in your body. It plays a role in converting food to energy, as well as maintaining DNA integrity and proper cell function.
• A new test will come out soon — I’m excited to announce the upcoming Mitochondrial Wellness Test Kit, which will provide a snapshot of your latest mitochondrial function. While helpful, certain specialized tests will be needed to understand the nuances of your health.
• Current NAD+ testing is unsatisfactory — NAD+ rapidly deteriorates once it’s outside your cells, making accurate measurement tricky. Because of this fragility, samples require immediate handling and specialized techniques to avoid losing accuracy.
Typically, precise NAD+ measurement demands blood samples to be drawn and analyzed swiftly within the same specialized research facility — something not possible at most regular clinics. Transporting samples between labs also compromises results significantly due to degradation. However, these challenges haven’t stopped our mission to deliver valuable health insights.
• NAD+ testing standards will rise — My team and I have developed an innovative approach that bypasses the complexity of direct NAD+ measurement. Instead, our method evaluates your NAD+ status indirectly by examining the redox balance among these essential markers — acetoacetate and betahydroxybutyrate, lactate and pyruvate, and the oxidized and reduced forms of glutathione.
• The test will be affordable — I’m proud to share that this cutting-edge NAD+ test is inexpensive, giving more people access to their current cellular health. More announcements will be made once this product is available.
Assessing Your Gut Health
Another crucial aspect of your health that needs to be tested regularly is your gut function. As you know, certain gut strains are beneficial, while others aren’t. Thus, figuring out which bacteria are dominating your gut will give you an insight to what’s happening.
• Gut Microbiome Wellness Test Kit — Just like the Mitochondrial Wellness Test Kit, my team and I will be releasing the Gut Microbiome Wellness Test Kit. It’s uniquely crafted to help you gain insights into your gut bacteria’s profile. It will seamlessly pair with the upcoming Mercola Health Coach app, providing you with a seamless end-to-end journey — from collecting your sample to interpreting your results.
To paint a picture of this process, you’ll need to send over a fecal sample. Afterward, you’ll be provided with a detailed breakdown of key bacterial species, allowing you to make smarter dietary and lifestyle decisions. To encourage broad access among the public, we’re also giving it an affordable price tag.
• Frequency of gut microbiome testing — One major reason why we’ve made this test affordable is to encourage repeat testing, ideally twice a year. This is needed to see whether your situation has improved or worsened, and you cannot know what your status is if a single test already requires a significant amount of cash.
Tips on Addressing Nutritional and Hormonal Deficiencies
The reason why I recommend you get yourself screened is to help save you time and money. For example, if one vitamin is already at an optimal range, you can focus your effort on others that need more attention. That said, I recommend going through the following articles. They contain helpful strategies to help you maintain optimal health after you’ve completed your tests:
- Everything You Need to Know About Vitamin D for Your Health
- High Iron Levels Threaten Bone Health and Increase Fracture Risk
- How Low Testosterone Affects Men’s Health
- Blocking Cortisol Extends Lifespan by Improving Mitochondrial Function
- Key Nutrients to Support Optimal Thyroid Health
- The Crucial Role of NAD+ in Optimal Health
- Unlocking the Secrets of Gut Health
Frequently Asked Questions (FAQs) About Regular Health Screenings
Q: Why is guessing about your health risky?
A: Guessing or relying on symptoms alone can result in serious health issues going undetected, delaying necessary treatments and reducing your chances of successful recovery. Accurate lab testing removes uncertainty, providing clear insights into your health status.
Q: What tests are essential for assessing iron overload?
A: Begin with a serum ferritin test, which reveals how much iron your body stores. For a comprehensive view, consider an iron panel, Complete Blood Count (CBC), gamma-glutamyl transferase (GGT), and a metabolic panel to fully evaluate your iron levels and overall health risks.
Q: Why is it important to monitor cortisol and testosterone levels?
A: Cortisol levels reflect stress and inflammation, significantly influencing aging, muscle health, and immune function. Testosterone is linked directly to mortality risk, cardiovascular health, and overall vitality. Regularly testing these hormones helps detect and manage imbalances early, protecting your long-term health.
Q: How can you accurately assess your thyroid health?
A: Traditional testing methods, like TSH levels or basal body temperature alone, often fail to identify underlying thyroid conditions such as Hashimoto’s thyroiditis. Testing thyroid antibodies (TgAb and TPOAb), along with a comprehensive panel (TSH, T3, T4, reverse T3, cholesterol), provides a clearer picture and helps target autoimmune-related thyroid issues.
Q: How do NAD+ and gut microbiome tests contribute to overall wellness?
A: Measuring NAD+ indirectly through redox balance markers provides critical insights into mitochondrial and cellular health, influencing energy and metabolic functions. Gut microbiome testing identifies beneficial and harmful bacterial strains, guiding informed dietary and lifestyle adjustments. Both tests are designed to be affordable, accessible, and offer actionable results for improving overall wellness.
How to Tell the Difference Between Freckles, Sunspots, and Moles
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/04/26/difference-between-freckles-sunspots-moles.aspx
Analysis by Dr. Joseph Mercola April 26, 2025

STORY AT-A-GLANCE
- Freckles are small, flat, light brown spots that darken in summer and fade in winter; they typically appear in clusters on sun-exposed areas
- Moles can be flat or raised, tan to dark brown, sometimes with hair, and should be monitored for skin cancer warning signs
- Sunspots, often called liver spots, are signs of oxidative damage — not just sun exposure — and reflect excess linoleic acid (LA) and iron in your body
- Lipofuscin, a waste product formed when oxidized LA binds with iron, builds up in sun-exposed skin as you age, creating the brown pigmentation seen in sunspots
- Checking your serum ferritin levels and reducing LA intake helps prevent and reverse oxidative stress that leads to sunspots and premature skin aging
Have you ever looked in the mirror and wondered about those little marks on your skin? Maybe they’re freckles from your childhood, sunspots from sunny vacations or moles you’ve had forever. These spots are more than just part of your look — they’re clues to your health.
The good news? You can take charge of your wellness starting today. In this guide, you’ll learn what freckles, sunspots and moles really are, how to tell them apart and what to do if they signal trouble. Get ready to feel confident about your skin and empowered to keep it healthy.
What Do Your Skin Spots Look Like?
Your skin is like a scrapbook, full of stories from sunny days and family traits. To understand those stories, you need to know what each spot looks like. Let’s break it down so you can spot freckles, sunspots and moles with ease.
• Freckles — tiny paint splatters — Picture freckles as tiny paint splatters on your skin. They’re small, flat and usually light brown or tan. You’ll often see them in clusters on your face, arms or shoulders. These spots love the sun — they get darker in summer and fade in winter, especially if your skin is fair. Freckles are common and usually no big deal.1
It’s interesting to note that newborns are rarely born with freckles; they typically start appearing in early childhood after sun exposure. The tendency to develop freckles is strongly linked to the presence of a gene that affects the type of melanin produced by your body.2
• Sunspots — sun’s lasting marks — Sunspots are flat, brownish and can be as small as a pencil eraser or as big as a small coin. Look for them on sun-exposed areas like your hands, face or chest. Unlike freckles, they don’t fade with the seasons — they stick around all year.3
• Moles — little skin islands — Think of moles as little islands on your skin. They can be flat or raised, tan to dark brown, and sometimes even have hair growing from them. Moles can pop up anywhere — not just where the sun hits — and they’re usually permanent. Most are harmless, but it’s smart to keep an eye on them.
The number of moles a person has can vary greatly, with some individuals having only a few while others have many. Most moles develop during childhood and adolescence, but it’s also common to develop new moles in adulthood, particularly during periods of hormonal change like pregnancy.
The Root Causes — Why Do These Spots Appear?
Why does your skin decide to sprinkle itself with spots? It’s a mix of your genes and how much sun you’ve soaked up. Here’s are several reasons why freckles, sunspots, and moles show up.
• Freckles — a combination of genetics and sun — Freckles are like your skin dancing with the sun, guided by your family traits. If you’ve got fair skin and freckles run in your family, sunlight tells your skin to sprinkle extra color in tiny dots. It’s a natural occurrence — not a sign something’s wrong.
• Sunspots — oxidative damage from linoleic acid (LA) and iron — Unlike freckles, sunspots aren’t just about melanin buildup. They also contain lipofuscin, a brown pigment made from oxidized LA bound to excess iron. High levels of LA from vegetable oils, combined with elevated iron, create oxidative damage that builds up in sun-exposed skin over time. That’s why these spots become more visible with age.
• Moles — clusters of character — Moles are like little bursts of personality, shaped by your DNA and sometimes the sun. Some appear when you’re born, while others grow later as you age or catch some rays. They happen when pigment cells clump together instead of spreading out evenly.

Save This Article for Later – Get the PDF Now
Sunspots Are Signs of Oxidative Stress
Sunspots are more than just the result of sun exposure — they’re a visible sign of oxidative damage happening under the surface. What many people don’t realize is that sunspots, which are sometimes called liver spots, are largely made up of a substance called lipofuscin.
• Lipofuscin is often described as a type of “age pigment” — More accurately, it’s the accumulation of cellular waste formed when LA, a polyunsaturated fat found in vegetable oils, gets oxidized by excess iron in your body. In other words, lipofuscin is a byproduct of oxidative damage — and the brown spots you see are your skin’s way of showing it.
• High levels of iron act as a catalyst for this process — This is especially true when combined with a high intake of LA. The result? An overload of oxidative byproducts that collect in your skin, especially in sun-exposed areas. Over time, this creates the brown pigmentation we recognize as sunspots or liver spots.
• This process doesn’t just affect your appearance — It could also signal an increased risk of skin aging and even cancer. That’s why I recommend checking your iron levels with a simple blood test called a serum ferritin test.
Ideally, your ferritin should fall between 35 and 45 ng/mL. If it’s higher, regular blood donation — two to four times per year — is an effective, natural way to remove excess iron and reduce oxidative stress. You can also remove smaller amounts monthly if needed.
• Another helpful screening tool is a gamma-glutamyl transpeptidase (GGT) test — This serves as a proxy for free iron levels and oxidative stress. Elevated GGT indicates an increased risk for cardiometabolic disease and even sudden cardiac death.
So, while sunspots seem like simple cosmetic issues, they’re actually telling you a deeper story about your internal health. Treat them as a signal to evaluate your diet and iron load.
When Should You Worry?
Most skin spots are just part of your unique look, but some hint at bigger issues. Knowing what to watch for is important to help you catch problems early. Here’s how to tell if your spots need extra attention.
• Freckles are usually safe — Freckles are usually harmless, but if one starts growing, changing color or looking unusual, take notice. It’s rare, but a changing freckle could mean something serious like skin cancer. Don’t panic — just get it checked out.
• Sunspots are caution signs — Sunspots look harmless, but they’re more than just souvenirs from sunny days. This buildup of cellular waste is a visible sign of deeper oxidative stress and damage to your skin. If they get bigger, darker or have uneven edges, they might signal skin cancer. Don’t brush off those changes — get them checked out by a dermatologist.
• Moles — Check the ABCDEs — Moles are often just beauty marks, but some hide risks like melanoma. Use this simple ABCDE checklist to stay on top of them.4 If a mole shows any of these signs, see a doctor right away. Early action is your best defense:
◦Asymmetry — One side doesn’t match the other.
◦Border — Edges are jagged or blurry.
◦Color — Mixed colors or odd shades.
◦Diameter — Bigger than a pencil eraser (about 6 millimeters).
◦Evolving — It’s changing in size, shape or feel.
How to Monitor and Protect Your Skin
You’ve got the know-how — now it’s time to take control. Keeping your skin healthy is easier than you think with a few simple habits. Here’s how to stay on top of your spots and shield your skin.
• Do a monthly skin check — Grab a mirror and set a monthly date to look over your skin. Check your front, back and sides — use a hand mirror for spots like your scalp or back. Look for new spots and note any changes.
• Embrace the sun safely — Regular sun exposure is key for optimal health. However, it’s best to avoid direct sunlight during peak hours (10 a.m. to 4 p.m.) until you’ve cut back on LA-rich vegetable oils for at least six months. When LA accumulated in your skin interacts with the sun’s UV rays, it triggers inflammation and DNA damage.
• Know when to call a pro — If a spot starts growing, itching or changing colors, don’t wait. Make an appointment with a dermatologist. Spotting issues early keeps your skin in top shape.
Your skin’s story is yours to write. You now know how to spot freckles, sunspots and moles, why they pop up and when to get them checked. With a quick monthly scan and some sun-smart moves, you’re already building a foundation for healthier skin. Add in some skin-boosting tools, like healthy foods, methylene blue and niacinamide, and you’re on your way to a healthier you.
FAQs — Your Top Skin Spot Questions Answered
Q: What’s the difference between a freckle and a sunspot?
A: Freckles are small, light brown spots that darken in the sun and fade in winter. Sunspots are larger, darker and stay year-round. They often contain lipofuscin, a compound formed by the oxidation of LA and iron, which signals deeper oxidative damage in your skin.
Q: Can moles turn into cancer?
A: Yes, some moles can become melanoma, a type of skin cancer. Watch for asymmetry, unusual borders, odd colors, size over 6 millimeters or changes. Make it a habit to regularly examine your moles for any of these warning signs.
Q: How can I protect my skin from the sun?
A: Embrace the sun safely by avoiding peak hours (10 a.m. to 4 p.m.) until you’ve cut back on vegetable oils, which contain LA, for six months. This helps reduce inflammation and DNA damage from UV rays, caused by LA accumulated in your skin.
Also, consider checking your serum ferritin levels to ensure your iron is in the optimal range (35 to 45 ng/mL). Reducing both LA and excess iron helps minimize oxidative stress and prevent sunspots and premature aging.
Q: When should I see a doctor about a skin spot?
A: If a spot grows, itches, bleeds or looks different from others, see a dermatologist. Quick action catches problems early. Don’t hesitate to schedule an appointment if you have any concerns about a skin spot.
Q: Are certain people more prone to developing these skin spots?
A: Yes, individuals with fair skin and a family history of freckles are more likely to develop them. Sunspots, on the other hand, are more common in those with high iron levels, elevated LA intake and cumulative sun exposure. The number of moles a person has is often genetically determined.
The Hidden Link Between Vitamins and Hair Loss
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/03/29/vitamin-deficiencies-hair-loss.aspx
Analysis by Dr. Joseph Mercola March 29, 2025

STORY AT-A-GLANCE
- Vitamin deficiencies often cause hair loss, with nutrients like vitamins D, B12, A and iron playing key roles in maintaining healthy hair growth cycles
- Vitamin D supports hair follicle development, while B vitamins help produce keratin — the protein that forms hair structure
- Iron carries oxygen to hair follicles; deficiency causes poor growth, but too much is also harmful, with ideal serum ferritin levels being 20 to 40 ng/mL
- Vitamin A regulates scalp health through sebum production; both deficiency and excess cause hair problems like dryness or thinning
- A nutrient-rich whole foods diet is the best approach to addressing vitamin-related hair loss, with supplement used only when necessary after proper testing
Picture this: you step out of the shower, glance down and see a tangle of hair circling the drain — more than usual. You wonder, “What’s happening to my hair?” While stress or family genes could be culprits, there’s another common reason you might not have thought of: vitamin deficiencies. Your hair acts like a window to your overall health, dropping hints about what’s going on inside your body.
When it thins or falls out more than normal, it’s often a signal that you’re low on some key nutrients. Nutrients like vitamins D, B12 and A, and iron, keep your hair looking full and healthy. If you don’t get enough, your locks could suffer as a result.
Understanding Your Hair’s Growth Cycle
Hair growth follows a structured cycle with three phases: the growth phase (anagen), the transition phase (catagen) and the resting phase (telogen). This process ensures continuous renewal, much like a plant that sprouts, matures and eventually sheds to allow new growth. Vitamins are indispensable to this cycle, acting as nutrients that sustain hair health.
For example, vitamin D supports healthy hair follicles, while B vitamins contribute to keratin production — the protein that forms your hair’s structure. Insufficient levels of these nutrients disrupt the cycle, causing hair to enter the resting phase prematurely and resulting in increased shedding or thinning. In short, vitamins are the foundation for robust hair growth; without them, the cycle falters.
What Are the Benefits of Vitamin D for Your Hair?
Widely recognized for supporting bone health, vitamin D also plays a key role in hair vitality. It promotes the development of cells that develop into hair follicles, the microscopic structures responsible for hair growth. Vitamin D levels are often low in people with hair loss.1 A deficiency impairs follicle production, leading to thinning hair. Consider vitamin D as the catalyst that initiates healthy hair renewal.
• Identifying a vitamin D deficiency — Signs like excessive hair loss, along with fatigue or muscle pain, may point to low vitamin D levels. The best way to know if you’re in an optimal or deficient state is to get your vitamin D level tested. I recommend doing this twice a year. Regular monitoring is key to keeping your vitamin D level in a healthy range, ideally between 60 to 80 ng/mL (150 to 200 nmol/L).
• Strategies to boost vitamin D — The best way to boost your vitamin D level is with regular sun exposure. However, I must caution you about sun exposure during peak hours if you consume dietary seed oils. These oils, which are rampant in processed and fast food, are packed with linoleic acid (LA). When LA accumulated in your skin interacts with the sun’s ultraviolet (UV) rays, it triggers inflammation and DNA damage.
It’s best to avoid direct sunlight during peak hours (10 a.m. to 4 p.m.) until you’ve cut back on seed oils for six months. This gives your body time to clear some of the accumulated LA. If sun exposure isn’t possible, vitamin D3 supplementation is often necessary. Remember to have your vitamin D levels tested and, based on your test results, adjust your sun exposure or your supplement dose accordingly to maintain a vitamin D level between 60 to 80 ng/mL (150 nmol/L to 200 nmol/L).

Save This Article for Later – Get the PDF Now
How Do B Vitamins Help Your Hair Stay Strong?
Biotin (B7) helps make keratin, the protein your hair’s built from. Not enough, and your hair might get brittle or thin.2 Think of biotin as the builder stacking strong bricks for your hair. Vitamin B12 keeps your blood cells healthy, carrying oxygen to your hair roots. When these vitamins are low, hair becomes weak, grows slowly or break easily.
• Signs of deficiency — Thinning hair with symptoms like fatigue or pale skin often signal a B vitamin shortage. Hair loss and red, scaly rashes (especially on your face) are common signs you may need more biotin.
• Increasing B Vitamin Intake — To increase vitamin B12, incorporating B12-rich foods, such as grass fed meat and dairy, into your diet. Vegetarians and vegans, who are particularly at risk for vitamin B12 deficiency due to dietary restrictions, should consider supplements. Oral or intramuscular vitamin B12 supplements help restore adequate levels, depending on the severity of the deficiency.
Oral supplementation is generally effective for mild to moderate deficiency, with dosages ranging from 1,000 to 2,000 micrograms daily. Intramuscular injections, typically administered monthly, may be more suitable for patients with severe deficiency or those with malabsorption issues. Pastured egg yolk is one of the best sources of biotin. Since biotin is water-soluble, your body will not store it. Hence, your intake must remain consistent.
Why Does Iron Matter for Your Hair Growth?
Iron is essential for hair health, helping red blood cells carry oxygen to hair follicles.3 Without enough iron, follicles can’t get the oxygen they need, slowing growth and causing shedding. While too little iron contributes to thinning hair, having either too much or too little iron has serious repercussions. The fact is, iron deficiency is commonly checked for, but iron overload is a far more common problem, yet is often overlooked or ignored.
• Detecting low iron — Hair loss along with fatigue, memory problems or pale skin could mean an iron deficiency.4 A straightforward blood test, known as a serum ferritin test, provides valuable insights into your iron status. You want your ferritin level below 100 ng/mL; the ideal range is 20 to 40 ng/mL. Below 20 ng/mL is an indicator that you are iron deficient, while a level above100 ng/mL indicates inflammation, high iron or both.
• Boosting iron levels — Eat iron-rich foods like grass fed red meat and pair them with vitamin C from citrus fruits to improve absorption.5 Before considering supplements, be sure to get a serum ferritin blood test, as too much iron is harmful.
How Does Vitamin A Help or Hurt Your Hair?
Vitamin A keeps your scalp healthy by controlling sebum production, the natural oil that moisturizes hair.6 Too little dries out hair, while too much contributes to thinning and scalp issues. Vitamin A is like a dial that needs to be set just right for optimal hair growth.
• Recognizing vitamin A imbalance — Dry, brittle hair is often a sign you need more vitamin A, but thinning or scalp irritation could signal excess.7
• How to boost vitamin A levels — To optimize your vitamin A status, focus on consuming a variety of vitamin A-rich foods. Good sources include liver, egg yolks, butter from grass fed cows, and orange and yellow vegetables like sweet potatoes and carrots. These foods provide either preformed vitamin A or provitamin A carotenoids that your body can convert to active vitamin A.
While supplementation can be beneficial if you’re deficient, it’s important not to exceed recommended intake levels, due to negative effects from excessive supplementation. If you’re concerned about your vitamin A status, consider having your levels tested before starting any supplementation regimen.
Supporting Hair Health Through Nutrition
Your hair often reflects your inner health, with thinning or shedding hinting at deficiencies in vitamins D, B12 or A, and possibly iron. Each plays a unique role in hair growth, strength and scalp health. The good news? Fixing these gaps is simple. A diet rich in nutrients, based on a variety of whole foods, gives your hair what it needs.
If hair loss continues, however, see a holistic doctor, as a blood test is useful for spotting nutrient deficiencies, leading to targeted treatments like diet changes or supplements to get your hair growth and overall health back on track.
Frequently Asked Questions About Vitamins and Hair Loss
Q: Which vitamins are most important for hair growth?
A: Vitamin D, vitamin B12, biotin, iron and vitamin A are key nutrients for hair health, supporting follicles, hair strength and scalp health.
Q: How should I get these vitamins?
A: Sunlight is the best source of vitamin D. Vitamin B12-rich foods include grass fed meat and dairy. Pastured egg yolk is one of the best sources of biotin, while iron-rich foods include grass fed red meat. Good sources of vitamin A include liver, egg yolks, butter from grass fed cows, and orange and yellow vegetables like sweet potatoes and carrots.
Q: How can I identify a vitamin deficiency?
A: Watch for thinning hair, fatigue or pale skin. Ask for a blood test from your doctor to confirm any nutrient deficiencies.
Q: Can supplements quickly fix hair loss?
A: While certain supplements support hair health, diet comes first. Be sure to prioritize dietary changes, with a focus on fresh, whole foods, and use supplements only when needed.
Q: What causes excessive hair shedding?
A: Some shedding is normal, but nutrient deficiencies often worsen it. Hair shedding is also triggered by hormonal changes (pregnancy, menopause, thyroid disorders), stress, certain medications, sudden weight loss, seasonal changes and underlying health conditions like autoimmune disorders.
High Iron Levels Threaten Bone Health and Increase Fracture Risk
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/01/16/high-iron-levels-bone-health.aspx
Analysis by Dr. Joseph Mercola January 16, 2025

Story at-a-glance
- High iron levels, particularly serum ferritin above 1,000 µg/L, significantly increase the risk of fractures, with vertebral fractures being most common. Managing iron levels is key to reducing this risk
- Both iron overload and deficiency weaken bones. Excess iron promotes osteoclast activity, leading to bone resorption, while insufficient iron impairs osteoblast function, disrupting bone formation
- Elevated iron levels adversely affect bone microarchitecture, compromising bone strength and increasing fracture susceptibility
- Excess iron leads to the production of reactive oxygen species, causing oxidative stress that damages bone cells and disrupts their function, further weakening bones
- If your ferritin levels are high, establish a regular blood donation schedule of two to four times per year to effectively remove excess iron from your body
Iron overload, often abbreviated as IO, presents a significant risk factor for fractures. Conventional treatments for IO, such as phlebotomy and iron chelation therapy, aim to reduce iron levels but come with their own set of challenges. Phlebotomy, for instance, involves regular blood removal, which is inconvenient and uncomfortable for patients. Iron chelation therapy, while effective, leads to side effects like gastrointestinal disturbances and kidney issues.
The underlying causes of IO are diverse and complex. Hereditary hemochromatosis (HH) is a genetic disorder that leads to excessive iron absorption from the diet. Other conditions, such as thalassemia and sickle cell disease, also result in iron overload due to frequent blood transfusions.
Chronic liver diseases, including hepatitis C and nonalcoholic fatty liver disease, contribute to elevated iron levels as well. Additionally, postmenopausal women may experience increased iron stores due to hormonal changes. These underlying causes disrupt your body’s iron regulation, leading to IO.
In HH, mutations in the HFE gene cause the body to absorb more iron than needed, resulting in accumulation in organs like the liver and heart. In thalassemia and sickle cell disease, repeated blood transfusions introduce excess iron, which the body cannot excrete efficiently. Chronic liver diseases impair the liver’s ability to produce hepcidin, a hormone that regulates iron balance, further exacerbating iron accumulation.
Diagnosing IO is challenging due to the variability in symptoms and the overlap with other conditions. Many individuals with IO remain undiagnosed until significant organ damage occurs.
Iron Overload Significantly Increases Fracture Risk
A population-based matched cohort study investigated the relationship between iron overload disorders and the risk of bone fractures, aiming to determine whether elevated iron levels significantly increase the likelihood of fractures among affected individuals.1
The study included 20,264 patients diagnosed with iron overload and 192,956 matched control participants. The population consisted of adults over 18 years old, with an average age of 57, and approximately 40% were female. The findings revealed a 55% increased risk of fractures among patients with iron overload, with the highest risk observed for vertebral fractures.2
Specifically, patients with serum ferritin levels exceeding 1,000 µg/L, a marker indicating high iron in the blood, had a 91% increased risk of any fracture and a 2.5-fold increased risk of vertebral fractures.3 Notably, the study found no elevated fracture risk among patients without high serum ferritin levels. Additionally, the risk was consistent across both males and females, indicating that iron overload affects fracture risk similarly regardless of sex.4
One of the key biological mechanisms identified is that iron overload adversely affects both bone quantity and the microarchitecture — the tiny structures that make up bone. This deterioration compromises bone strength, making fractures more likely.5 The study underscores the importance of monitoring serum ferritin levels as an indicator of fracture risk, especially in individuals with laboratory-confirmed iron overload.6
Moreover, the research highlighted that hereditary hemochromatosis, thalassemia major and sickle cell anemia are significant contributors to iron accumulation in the body. These inherited blood disorders disrupt iron regulation, leading to excessive iron storage and subsequent bone health issues.7
In fact, decreased bone mineral density was observed in over 70% of adults with sickle cell disease and over 60% of adult thalassemia patients.8 Addressing iron overload effectively therefore helps preserve bone integrity and reduce the incidence of fractures in this vulnerable population.
Iron’s Dual Impact on Bone Health
A review published in the journal Pharmaceuticals further explored how different levels of iron in the body influence bone health, particularly focusing on the roles of osteoclasts and osteoblasts — the cells responsible for breaking down and building up bone, respectively.
The researchers aimed to understand whether having too much or too little iron could disrupt the balance between these two types of cells, ultimately affecting bone strength and increasing the risk of fractures.9 The review examined individuals with various iron-related conditions, including hereditary hemochromatosis, thalassemias and sickle cell disease.
A significant percentage of patients with these iron overload disorders exhibited decreased bone mass and an increased likelihood of bone fractures.10 However, the findings revealed that both high and low iron levels negatively impact bone mineral density, leading to conditions like osteoporosis and osteopenia.
Delving deeper, the research highlighted that excess iron promotes the activity of osteoclasts, the cells that resorb or break down bone tissue. This heightened osteoclast activity accelerates bone loss, weakening the skeletal structure and making bones more susceptible to fractures.
On the flip side, insufficient iron levels also disrupt bone health by impairing the function of osteoblasts, the cells responsible for bone formation. This dual disruption further exacerbates the risk of developing osteoporosis and other bone-related issues.11 The study also uncovered that elevated iron levels lead to the production of reactive oxygen species (ROS), which are chemically reactive molecules containing oxygen.
ROS contribute to oxidative stress, damaging bone cells and impairing their ability to function correctly. This oxidative stress not only hampers the formation of new bone by osteoblasts but also encourages the breakdown of existing bone by osteoclasts, creating a vicious cycle of bone deterioration.12
Biologically, the mechanisms by which iron affects bone health are intricate. Excess iron interferes with the differentiation and activity of osteoblasts by downregulating key genes like Runx2, which are essential for bone formation. Additionally, high iron levels enhance osteoclastogenesis — the formation of more osteoclasts — through pathways involving ROS and NF-κB signaling.
These processes collectively lead to increased bone resorption and decreased bone formation, undermining bone integrity and strength.13
In summary, maintaining balanced iron levels is necessary for bone health. Both iron overload and deficiency disrupt the delicate equilibrium between bone resorption and formation, leading to weakened bones and a higher risk of fractures. Understanding these mechanisms underscores the importance of monitoring and managing iron levels to preserve bone strength and prevent osteoporosis.14

Save This Article for Later – Get the PDF Now
Simple Steps to Reduce Iron Overload and Protect Your Bones
Iron overload wreaks havoc on your bone health by disrupting the delicate balance between bone formation and breakdown. The good news? You have the power to address this issue through straightforward lifestyle changes that make a real difference in protecting your skeletal system. Here are four powerful ways to get your iron levels under control:
1. Get your iron levels tested regularly — You can have your iron levels checked using a simple blood test called a serum ferritin test. I believe this is one of the most important tests that everyone should have done on a regular basis as part of a preventive, proactive health screen.
You want your ferritin level below 100 ng/mL, however the ideal range is 20 to 40 ng/mL. Below 20 ng/mL is an indicator that you are iron deficient. Aside from a serum ferritin test, a gamma-glutamyl transpeptidase (GGT) test is another screening marker for excess free iron and is a great indicator of your risk for sudden cardiac death, insulin resistance and cardiometabolic disease.
2. Donate blood to lower excess iron — Your body has a limited capacity to excrete iron, so it can easily build up in organs like your liver, heart and pancreas. This is dangerous because iron is a potent oxidizer that damages your tissues and contributes to a variety of health problems, including cancer.
If your ferritin levels are high, establish a regular blood donation schedule of two to four times per year. This natural approach effectively removes excess iron from your body since blood loss remains the only way your body eliminates iron. Your contributions help others while protecting your bone health.
You can also remove blood in smaller amounts once a month according to the schedule below. If you have congestive heart failure or severe COPD, you should discuss this with your doctor, but otherwise this is a fairly appropriate recommendation for most. If, for some reason, a blood donor center is unable to accept your blood for donation, you can obtain a prescription for therapeutic phlebotomy.
| Men | Postmenopausal Women | Premenopausal Women |
|---|---|---|
| 150 ml | 100 ml | 50 ml |
3. Monitor your diet — Avoid cooking in iron pots and pans, limit alcohol consumption, which increases iron absorption, and be cautious with iron-fortified processed foods. If you drink well water, install an iron precipitator or reverse osmosis filter to reduce iron exposure.
4. Optimize your calcium and copper intake — Adequate calcium intake reduces iron overload naturally. Focus on getting calcium from whole food sources rather than supplements. When calcium levels are low, your body releases more parathyroid hormone (PTH), which not only dissolves bone but also increases iron storage. Breaking this cycle through proper calcium nutrition helps protect both your bones and overall health.
Iron and copper are also highly interdependent and need to be considered together. Iron overload along with copper deficiency is a dangerous combination. Most people are deficient in copper and need more in order for their iron metabolism to function properly.
Depending on your copper levels, you may need to take up to 3 milligrams (mg) to 4 mg of copper bisglycinate per day, or eat copper-rich foods, such as bee pollen, grass fed beef liver and acerola cherry.
Acerola cherry is very high in vitamin C, which contains copper-rich tyrosinase enzyme. Retinol, which makes copper bioavailable, is also important. It’s found in beef liver and beef organs.
- 1, 2, 3, 4, 5, 6, 7, 8 The Journal of Clinical Endocrinology & Metabolism November 18, 2024, dgae807
- 9, 10, 11, 12, 13, 14 Pharmaceuticals 2018, 11(4), 107
All About Phytic Acid and Phytates – Good and Bad
Reproduced from original article:
https://www.precisionnutrition.com/all-about-phytates-phytic-acid
By Ryan Andrews, MS, MA, RD, RYT, CSCS
Phytic acid – the storage form of phosphorus – is one of those pesky “anti-nutrients” the Paleo community keeps telling you to avoid.
It’s often considered an anti-nutrient because it binds minerals in the digestive tract, making them less available to our bodies.
Yet these same anti-nutrient properties can also help in the prevention of chronic disease.
What is phytic acid?
Seeds — such as nuts, edible seeds, beans/legumes, and grains — store phosphorus as phytic acid. When phytic acid is bound to a mineral in the seed, it’s known as phytate.
The tables below compare various seed types according to their phytic acid/phytate content.
Whole grains
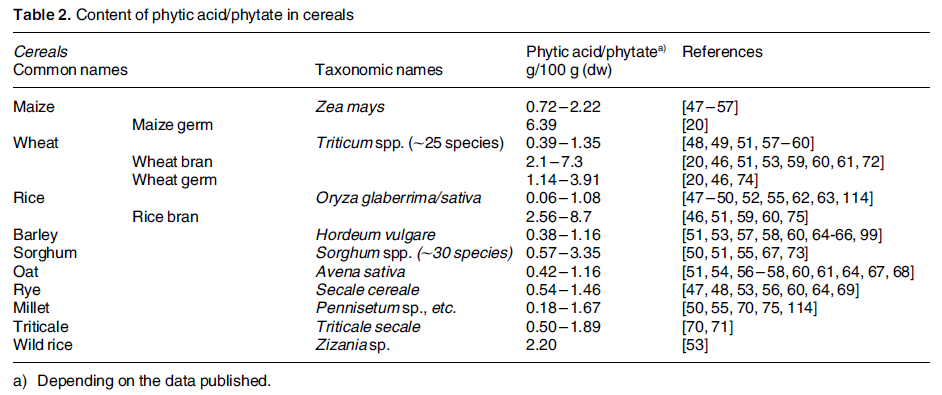
Legumes
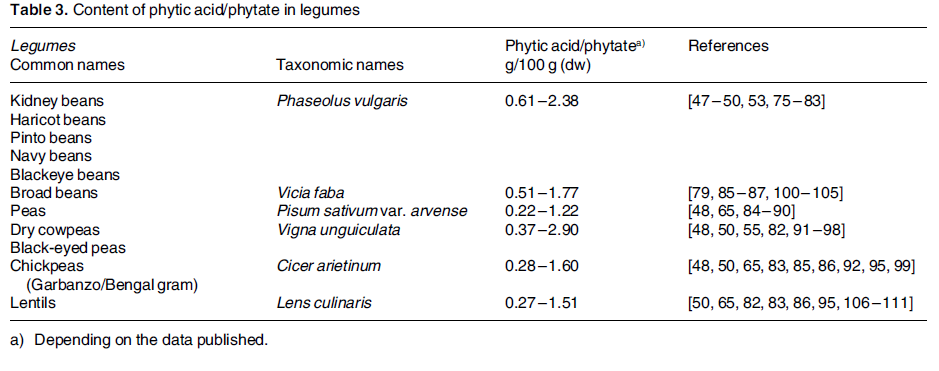
Nuts
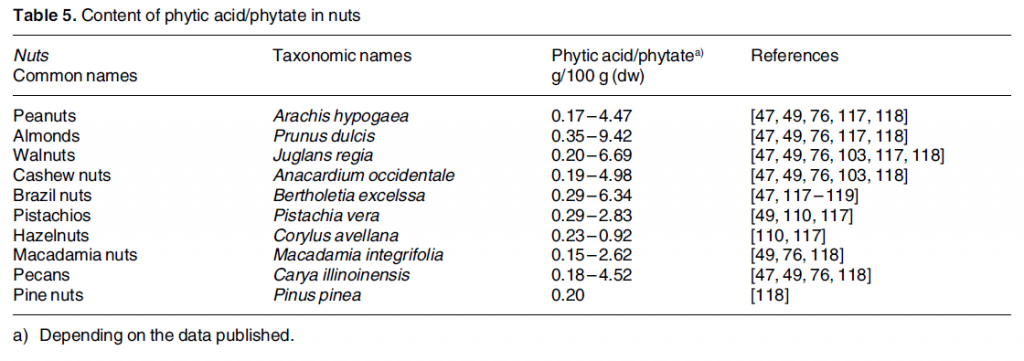
Oil seeds
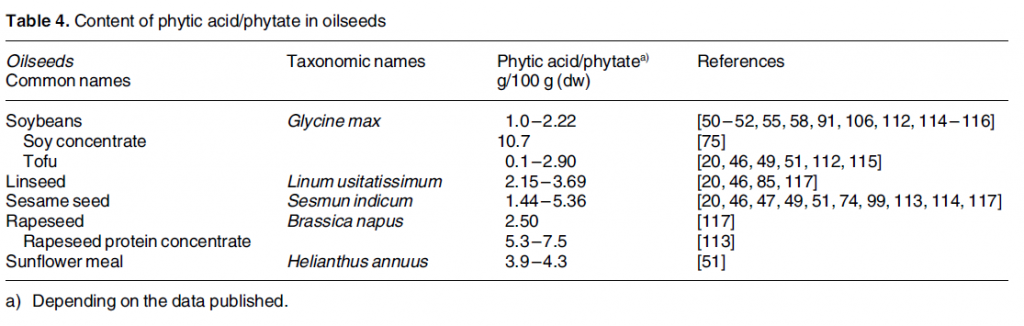
As you can see, phytic acid content varies greatly among plants. This is due to the type of seed, environmental condition, climate, soil quality, how phytate is measured in the lab, and so forth.
Roots, tubers, and other vegetables may also contain phytic acid, but usually in lower amounts.
The most concentrated sources tend to be whole grains and beans. Phytic acid is isolated in the aleurone layer in most grains, making it more concentrated in the bran. In legumes, it’s found in the cotyledon layer (where the protein is).
Phytate = phytic acid bound to a mineral
Phytates perform an essential role in plants, as they are an energy source for the sprouting seed. When a seed sprouts, phytase enzymes break down the stored phytates.
When we eat the plant, phytates are hydrolyzed during digestion to myo-inositol-1,2,3,4,5,6-hexkisphosphate (IP6) and lower inositol polyphosphates including IP1 through IP5 (these are phytate degradation products).
Who’s eating phytic acid?
Everyone who eats plants consumes some phytic acid. It’s all a question of degree.
As you can imagine, intake tends to be much higher among those who follow non-Westernized diets. In developing countries, plants are staple foods, which means people eat more of them, and therefore get more phytic acid.
In developed countries, plant-based or vegetarian eaters tend to consume more phytic acid than omnivores. Further, males usually consume more phytic acid than females, simply because they eat more food.
Phytate digestion
Most phytate (37-66%) is degraded in the stomach and small intestines.
Ordinarily, our bodies regulate phytate levels pretty well, adjusting uptake in the gut and excretion until body levels come into balance.
Vitamin D status in the body seems to influence how much phytate is actually retained. The more vitamin D, the more phytate retained; the less vitamin D, the less phytate retained.
Potential problems with phytic acid
Phytic acid can bind minerals in the gut before they are absorbed and influence digestive enzymes. Phytates also reduce the digestibility of starches, proteins, and fats.
Here’s an example.
Vegan eaters often consume more iron than omnivores. Yet, they also consume more anti-nutrients, including phytates, and these reduce the amount of iron available to their bodies. Consuming 5-10 mg of phytic acid can reduce iron absorption by 50%.
This is why vegetarian eaters should eat more iron than omnivores (33 mg for veg eaters vs. 18 mg for omnivores).
Daily iron loss for men & women
- Adult men lose ~1 mg of iron per day
- Adult menstruating women lose ~1.4 mg/day
- Postmenopausal women lose ~0.8 mg/day
- Lactating women lose ~1.1 mg/day
While in the intestines, phytic acid can bind the minerals iron, zinc, and manganese. Once bound, they are then excreted in waste.
This can be a good or bad thing, depending on the condition. It’s a bad thing if you’re having trouble building up iron stores in the body and have developed iron-deficiency anemia.
When is it a good thing? Keep reading – you’ll find potential benefits of phytic acid below.
Potential benefits of phytic acid
Despite its potential drawbacks, phytic acid is similar in some ways to a vitamin, and metabolites of phytic acid may have secondary messenger roles in cells.
Some experts even suggest that it’s the phytic acid in whole grains and beans that lends them their apparent protective properties against cardiovascular disease, cancer, and diabetes.
(Remember, the grains with little to no phytic acid are the refined ones.)
The supplement industry has caught on to this. Have you even seen a bottle of inositol hexaphosphate, or IP6? That’s simply a supplemental source of phytic acid.
When phytic acid binds minerals in the gut, it prevents the formation of free radicals, thus making it an antioxidant. Not only that, but it seems to bind heavy metals (e.g., cadmium, lead) helping to prevent their accumulation in the body
Phytic acid’s preventative properties
Cancer
Foods higher in phytic acid seem to enhance the activity of natural killer cells and inhibit tumor growth.
Those who consume more phytic acid are less likely to succumb to breast and prostate cancer. Exposing the colon to less iron seems to decrease the risk of colon cancer. And phytic acid might reduce the side effects of chemotherapy.
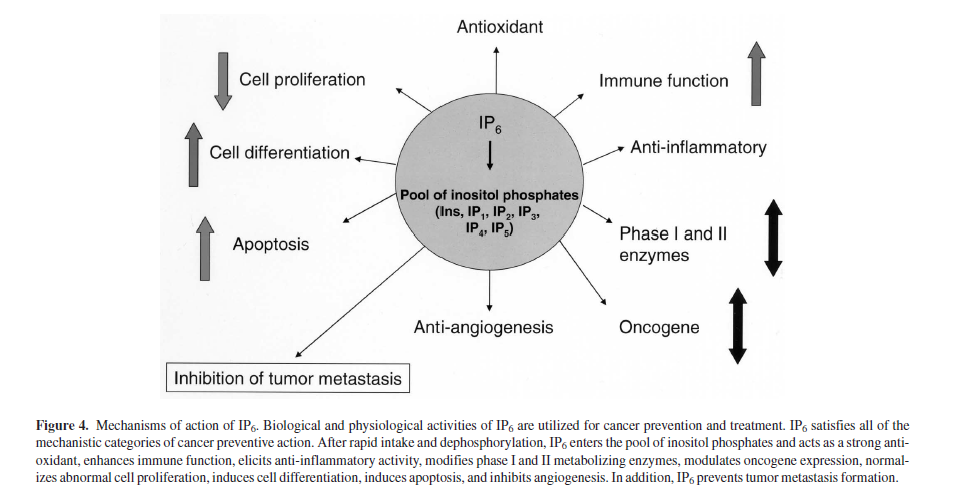
Cardiovascular disease
Phytic acid helps prevent hardening of the arteries and platelet formation.
Kidney stones
With some phytate being excreted in the urine, this may improve kidney health and prevent stones.
Insulin resistance
Phytic acid plays a role in pancreatic function and insulin secretion. And it may reduce the glycemic response from meals, meaning you feel full for longer.
Hemochromatosis
Hemochromatosis, or iron overload, is a common genetic disorder that phytic acid’s iron-binding properties can protect against or reduce.
In the balance
Is phytic acid worth worrying about? Maybe not, for most of us.
One study showed that subjects consuming a Mediterranean-style diet that included 1000-2000 mg of phytic acid per day did not suffer from reduced mineral bioavailability.
At the same time, certain people might have to be more wary.
In particular, iron intake and absorption can be critical for infants nearing six months of age. So when plants are added to infants’ diets, it may be important to adopt strategies to reduce phytic acid and enhance iron absorption.
Overcoming phytic acid as an antinutrient
Luckily, it’s possible to overcome the anti-nutrient effects of phytic acid in our foods while still getting the benefits of a plant-rich diet. Here are a few strategies that my be more or less helpful depending on the specific situation:
Heat
Heating foods can destroy small amounts of phytic acid. (Note: heat can also destroy phytase and vitamin C.)
Processing
Milling grains and removing the bran decreases phytic acid. Unfortunately, milling also tends to remove many of the minerals! Removing the bran and then enriching a food with minerals might allow for enhanced nutrient absorption in the body.
Soaking
Soaking beans and grains can reduce phytic acid (and other antinutrients).
Fermenting
Fermentation and bread leavening (using yeast) can help to break down phytic acid due to the activation of native phytase enzymes, reducing the number of phosphate groups.
This is big stuff since myo-inositol phosphates with fewer than five phosphate groups don’t inhibit zinc absorption (IP1 to IP4). And those with fewer than three phosphate groups don’t inhibit iron absorption (IP3 to IP2).
Also, some of the acids produced during fermentation might actually boost absorption of certain minerals.
Sprouting
Sprouting and malting enhances native phytase activity in plants and thus decreases phytic acid.
Vitamin C
Vitamin C appears strong enough to overcome phytic acid. In one study, adding 50 mg of vitamin C counteracted the phytic acid load of a meal. In another study, 80 mg of ascorbic acid (vitamin C) counteracted 25 mg of phytic acid.
Protein powders
During processing of plant-based protein powders, it’s possible to de-phytinize (via addition of microbial phytase). Also, protein isolates and concentrates can be treated with dialysis or ultrafiltration to remove phytic acid.
Seed breeding
Scientists are working on seed breeds containing less phytic acid. There are modern seed hybrids of grain and legume plants that contain less phytic acid.
Animal protein
Animal protein may enhance absorption of zinc, iron, and copper. Adding small amounts of animal protein might increase the absorption of these minerals in the body. (Well, except for dairy/casein, as it also seems to hinder iron and zinc absorption.)
Gut health
A low pH in the gut enhances iron absorption. Balancing the level of beneficial bacteria in the GI tract might help with this. See All About Probiotics.

Bonus: Can other animals digest phytic acid?
Ruminant animals (e.g., cattle, sheep, goats, buffalo) possess phytase producing flora for digesting phytic acid.
Non-ruminant animals (e.g., pigs, chickens, dogs, cats) don’t have phytase producing flora, so phytic acid passes through them undigested and makes its way into the soil.
Feeding livestock too much grain can inhibit mineral absorption and increase phosphorus excretion, leading to pollution. Ever heard of the Dead Zone in the Gulf of Mexico?
Summary and recommendations
In healthy people eating balanced diets, phytic acid’s effects on iron, zinc, and manganese status is minimal and it doesn’t seem to cause nutrient deficiencies.
To argue that some plant foods are “unhealthy” because of their phytic acid content seems mistaken, especially when phytic acid’s potential negative effects on mineral assimilation may be offset by its health benefits.
So we should aim to reduce phytic acid rather than eliminate it.
To reduce the anti-nutrient effects of phytic acid in foods, try the following:
- Soak, sprout, ferment, and cook plant foods.
- Consume vitamin C-rich foods with meals that contain phytic acid. Dense source of vitamin C include guava, bell pepper, kiwi, oranges, grapefruit, strawberries, Brussels sprouts, cantaloupe, papaya, broccoli, sweet potato, pineapple, cauliflower, kale, lemon juice, and parsley.
- Use vinegar in salad dressings and cooking to enhance mineral absorption and offset phytic acid.
- Supplement with phytase enzymes if necessary.
- Eat mineral fortified foods if necessary
- Supplement minerals if there is still a shortfall in your diet.
- If you’re eating a plant-based diet and have confirmed nutrient deficiencies, and you’ve tried all the above strategies with no success, adding small amounts of animal foods on occasion might boost stores of necessary minerals in your body.

‘Long Vax’ Finally Enters Lexicon
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/05/covid-vaccine-long-vax.aspx
Analysis by Dr. Joseph Mercola April 05, 2024

Story at-a-glance
- Dr. Pierre Kory and Dr. Paul Marik are trying to get the word out that long vax is not only real but has disabled many Americans who were at the peak of health prior to getting a COVID jab
- At Kory’s long COVID clinic, 70% of the patients actually have long vax and reported their symptoms began “minutes, hours, days or several weeks” after receiving a COVID-19 shot
- Long vax symptoms are nearly identical to those of long COVID — the difference being that the long vax patients tend to be sicker, with more frequent small fiber neuropathy and dysautonomia
- A study by Yale scientists detailed long vax, which they called chronic post-vaccination syndrome, in 241 people
- Top reported symptoms include exercise intolerance, excessive fatigue, numbness, brain fog and neuropathy
An estimated 6.4% of U.S. adults have experienced symptoms of long COVID, a term used to describe a complex disorder that persists for three or more months after contracting COVID-19.1 While long COVID has been extensively covered in the media, millions more suffer from long vax — a condition with nearly identical symptoms to long COVID, but often even more severe.
New York pulmonologist Dr. Pierre Kory and Dr. Paul Marik, a critical care doctor formerly with Sentara Norfolk General Hospital in East Virginia, are part of the Front Line COVID-19 Critical Care Working Group (FLCCC). They’re trying to get the word out that long vax is not only real but has disabled many Americans who were at the peak of health prior to getting a COVID jab.2
At Long COVID Clinic, 70% of Patients Have Long Vax
Kory opened a tele-health practice that specializes in treating COVID disease, including long COVID. Kory says:3
“Long COVID, although a new name, is not a new disease. It meets the diagnostic criteria for a decades-old condition called myalgic encephalitis/chronic fatigue syndrome (ME/CFS).
The three symptom ‘pillars’ which lead to the diagnosis are fatigue, post-exertional malaise (PEM), and ‘brain fog’ (i.e. cognitive deficits ranging from word finding difficulties, short term memory loss, inability to focus/comprehend, and more rarely confusion or disorientation).
Although this triad is present in nearly every patient I see (rarely brain fog is missing), the patients also present with a ‘side menu’ of problems which can include sensory neuropathies, dysautonomia/POTS, motor neuropathies, abdominal issues, musculoskeletal complaints, and cranial symptoms (i.e tinnitus, vertigo, headaches, vision, hearing loss, smell loss, taste loss).
Many of my patients are debilitated and meet criteria for disability, despite the majority reporting being in the peak of health and functioning prior to the pandemic.”
Yet, Kory and colleagues quickly noticed that most of their patients reported their symptoms began “minutes, hours, days or several weeks”4 after receiving a COVID-19 shot. While many had also had COVID-19, only a small number tied their symptoms to the viral infection.
While the team initially called the condition post-COVID vaccine injury syndrome, they changed the diagnosis to “long vax” because the symptoms were so close to long COVID — the difference being that the long vax patients tended to be sicker, with more frequent small fiber neuropathy and dysautonomia, Kory said.5
Research Details Neuropathic Symptoms Following COVID-19 Jabs
Scientific studies detailing long vax symptoms continue to emerge. In one study from early in the pandemic, more than two-thirds of those reporting long COVID symptoms had negative antibody tests, suggesting at least some of them didn’t even have COVID-19.6 Meanwhile, many COVID jab recipients report long COVID-like symptoms.
As reported by Science magazine in 2022, “In rare cases, coronavirus vaccines may cause long COVID-like symptoms,”7 which can include (but is not limited to) brain fog, memory problems, headaches, blurred vision, loss of smell, nerve pain, heart rate fluctuations, dramatic blood pressure swings and muscle weakness. The feeling of “internal electric shocks” are also reported.
Also in 2022, a preprint study from the U.S. National Institutes of Health reported new neuropathic symptoms that began in 23 adults within one month of receiving a COVID-19 shot.8 All of the patients felt severe tingling or numbness in their faces or limbs, and 61% also experienced dizziness when standing up, intolerance to heat and heart palpitations.
When 12 of the patients had their nerve function tested, seven had less sweating in their hands and feet than normal, while six had a condition where their heart beats too fast when they stand up.9
The researchers also took skin samples from the lower legs of 16 patients. Among them, 31% showed signs that the small nerves in the skin were not as dense as they should be, which can indicate nerve damage. Another 13% were on the border of being considered damaged, and 19% had swollen nerve fibers. When five of the samples were evaluated more closely, signs of an immune reaction in the blood vessels were detected.10
Further, while electrical tests on the nerves were normal for most participants, 52% showed clear signs of damage to the small nerves that can be felt but not easily seen. The study shows that after getting the COVID-19 shot, a range of symptoms related to nerve damage is possible, which might be caused by an immune system reaction.

Save This Article for Later – Get the PDF Now
Yale Scientists Detail Long Vax Symptoms
A study by Yale scientists, including Dr. Harlan Krumholz of Yale School of Medicine in New Haven, Connecticut, also shed light on long vax, which they described as chronic post-vaccination syndrome, or PVS.11 In a study of 241 people who reported PVS after an mRNA COVID-19 shot, the median time from the jab to the onset of symptoms was three days, with symptoms continuing for 595 days. The five most common symptoms included:12
- Exercise intolerance (71%)
- Excessive fatigue (69%)
- Numbness (63%)
- Brain fog (63%)
- Neuropathy (63%)
In the week before the survey was completed, patients reported a range of additional symptoms highlighting the mental toll the condition takes. The symptoms required a median of 20 interventions for treatment and included:13
| Feeling unease (93%) | Fearfulness (82%) |
| Overwhelmed by worries (81%) | Feelings of helplessness (80%) |
| Anxiety (76%) | Depression (76%) |
| Hopelessness (72%) | Worthlessness (49%) |
“In this study,” the researchers explained, “individuals who reported PVS after COVID-19 vaccination had low health status, high symptom burden, and high psychosocial stress despite trying many treatments. There is a need for continued investigation to understand and treat this condition.”14
Even a 2021 study reported a series of patients who experienced new autoimmune conditions — or flare-ups of existing autoimmune disease — following mRNA COVID-19 shots,15 highlighting the importance of careful research into the ongoing health risks.
Will Long Vax Be Censored?
It’s hopeful that scientific on long vax is reaching medical journals and getting some media coverage.16 But Kory and Marik are concerned it could reach a similar fate as other COVID shot coverage during the pandemic.
“The concern is that our findings, Krumholz’s study, and any reports of adverse events from COVID-19 vaccination, will be subject to the same institutional censorship we saw throughout the pandemic. Suppressing this information risks creating an even bigger disaster,” they told The Hill,17 referring to a potential epidemic of autoimmune diseases that could occur as a result.
“America’s health agencies need to snap into action to help study this problem so we can better understand and treat these conditions. Unfortunately, there doesn’t seem to be much hope of this happening,” Kory and Marik wrote. “The National Institutes of Health is fixated on studying the effect of Paxlovid, an antiviral COVID treatment, to treat long COVID and long vax, despite it having no proven effect on autoimmune disease.”18
Further, Kory explains that while major medical centers and hospitals across the U.S. have opened long COVID clinics, the treatments they offer are largely ineffective, and they often gas-lit long vax patients who tried to get help:19
“[F]or most of 2022 into 2023, those centers consistently gas-lit the Long Vax patients who presented to those clinics. Gaslighting of medical injuries is the well-described inability for physicians to recognize or accept when their own treatments (i.e the mRNA vaccines) cause harm …
The stories my patients would tell me of the care they received included what I would describe as abuse or insults from the treating physicians when the patients tried to convince them that the vaccines were the cause. These stories still make my blood boil and have estranged many of my patients from ‘the system.’ I believe the gaslighting responses have lessened somewhat but I don’t really know how much.
What angered me even further is that the health agencies only directed funding at long COVID and the medical literature and media only referred to sufferers as having long COVID. The contribution of the gene therapy vaccines are consistently ignored.”
Is Long Vax Behind the Explosion of Disability Claims?
Kory believes that long vax, and to a lesser extent long COVID, are behind the explosion of disability claims that have occurred since COVID-19 shots rolled out.20
Data compiled by former BlackRock analyst and fund manager Edward Dowd revealed a sobering glimpse into the true carnage that occurred at the hands of the COVID-19 shot campaign,21 and its results are striking. It revealed the following estimated human and economic costs:22
Human cost:
- 26.6 million injuries
- 1.36 million disabilities
- 300,000 excess deaths
Economic cost:
- Total: $147.8 billion
- Injuries: $89.9 billion
- Disabilities: $52.2 billion
- Excess deaths: $5.6 billion
What’s more, this data is from the employed population, aged 16 to 64 — a typically healthy crowd. To put this into perspective, John Leake writes on Courageous Discourse, “Note that this death count in one year is 5.2 times the number of men killed in ten years of combat in Vietnam.”23
Help for Long Vax Symptoms
As long vax and its symptoms become increasingly recognized, it will hopefully lead to increased access to effective treatments. If you’re experiencing symptoms, it’s important to find a holistic health care practitioner who’s familiar with long vax and how to treat it. You can also access FLCCC’s I-RECOVER24 guide,25 which offers step-by-step instructions on how to treat reactions from COVID-19 injections.26
I also summarized strategies to optimize mitochondrial health if you’re suffering from long COVID or long vax, with a focus on boosting mitochondrial health. To allow your body to heal you’ll want to minimize EMF exposure as much as possible. Your diet also matters, as the cristae of the inner membrane of the mitochondria contains a fat called cardiolipin, the function of which is dependent on the type of fat you get from your diet.
The type of dietary fat that promotes healthy cardiolipin is omega-3 fat, and the type that destroys it is omega-6, especially linoleic acid (LA), which is highly susceptible to oxidation. So, to optimize your mitochondrial function, you want to avoid LA as much as possible and increase your intake of omega-3s.
Primary sources of LA include seed oils used in cooking, processed foods and restaurant foods made with seed oils, condiments, seeds and nuts, most olive oils and avocado oils (due to the high prevalence of adulteration with cheaper seed oils). Animal foods raised on grains, such as conventional chicken and pork, are also high in LA.
Another major culprit that destroys mitochondrial function is excess iron — and almost everyone has too much iron. You can learn more about the health risks of excess iron in my interview with Christy Sutton, D.C. The most effective way to lower your iron is to donate blood two to four times a year.
Copper is also important for energy metabolism, detoxification and mitochondrial function, and copper deficiency is common. Other strategies include sun exposure and near-infrared light therapy, NAD+ optimizers and methylene blue, which can be a valuable rescue remedy. By improving your mitochondrial function and restoring the energy supply to your cells, you’ll significantly increase your odds of reversing the problems caused by the jab or the virus.
- 1 U.S. CDC, MMWR February 15, 2024 / 73(6);135–136
- 2, 3, 4, 5, 19, 20 Pierre Kory’s Medical Musings March 8, 2024
- 6 TNR December 8, 2022
- 7 Science January 20, 2022
- 8, 9, 10 medRxiv May 17, 2022
- 11, 12, 13, 14 medRxiv November 10, 2023
- 15 Int Immunopharmacol. 2021 Oct:99:107970. doi: 10.1016/j.intimp.2021.107970. Epub 2021 Jul 10
- 16, 17, 18 The Hill March 6, 2024
- 21 Phinance Technologies, The Vaccine Damage Project March 2023
- 22 Zero Hedge March 28, 2023
- 23 Substack, Courageous Discourse March 29, 2023
- 24, 25 FLCCC Alliance, I-RECOVER
- 26 FLCCC Alliance, I-RECOVER, Post-Vaccine Treatment Guide
Prunes or Plums — Which Has More Benefits?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/03/22/prunes-or-plums.aspx
Analysis by Dr. Joseph Mercola March 22, 2024

STORY AT-A-GLANCE
- Once known as prunes, dried plums are now the more palatable name for the fruit that, whether fresh or dried, contains numerous compounds that impart amazing health advantages
- Studies show that a single serving or about five dried plums may help prevent bone loss in older, osteopenic postmenopausal women
- Plums are loaded with flavonoid polyphenolic antioxidants, primarily lutein and cryptoxanthin, as well as neochlorogenic and chlorogenic acid, but the nutrients are highly concentrated in the dried fruits
- The vitamin C is destroyed when plums are dried, but they become significantly higher in other antioxidants and contain significantly higher concentrations of most of the other nutrients found in the fresh fruit
If you know anyone with osteoporosis, you may be familiar with some of the more overt signs, such as broken bones, weak grip strength or back pain. People with this condition may develop a “stooped” posture or even become shorter because their bones are literally being compressed.
There’s good news, though, as a study revealed dramatic and positive effects from dried plums. Scientists found that “dried plum not only protects against but more importantly reverses bone loss in two separate models of osteopenia,” another name for bone loss and the forerunner of osteoporosis.
Osteoporosis affects both males and females, although more women than men. One study describes it as a “debilitating disorder” exacerbated by age:
“As the demographic shift to a more aged population continues, a growing number of men and women will be afflicted with osteoporosis and a search for potential non-pharmacological alternative therapies for osteoporosis is of prime interest.
Aside from existing drug therapies, certain lifestyle and nutritional factors are known to reduce the risk of osteoporosis.
Our [three]-month clinical trial indicated that the consumption of dried plum daily by postmenopausal women significantly increased serum markers of bone formation, total alkaline phosphatase, bone-specific alkaline phosphatase and insulin-like growth factor-I by 12, 6, and 17%, respectively.”1
Ironically, several drugs taken for osteoporosis taken for five years or more have been shown to actually cause esophageal cancer, according to an Oxford study.2 However, in exploring non-pharmacological alternative therapies, researchers discovered dried plums may not only protect against, but reverse, the condition.
Researcher Bahram H. Arjmandi, Ph.D., from Florida State University, said that over his entire career, he’d examined many fruits, including figs, dates, strawberries and raisins, but none of them come close to having the effe
ct on bone density that dried plums or prunes have.
He added that in terms of bone health, this particular food is exceptional.3 Studies show that a single serving of dried plums may help prevent bone loss in older, osteopenic postmenopausal women as well as the previous recommendation of two servings, equating 100 grams or eight to 10 dried plums.4
Plum History and Description
Closely related to apricots, peaches and almonds, plums are an ancient fruit that experts believe may have originated in China, but were cultivated by Alexander the Great in Mediterranean regions by around 65 B.C.
Plums are about the size of limes, but that’s the only similarity. They’re dark purple (some have a golden tinge) with smooth, rather dull skins and sweet, delectable flesh inside, wrapped around a single, large pit, the main criteria for a drupe. Prunes are simply dried plums, the latter name thought to be more palatable.
All prunes are plums, but the reverse is not always the case. The high sugar content in plums allows them to be dried without fermentation. Further, like all dried fruit, dried plums are dehydrated by natural-drying, sun-drying and the use of dehydrators. Medical Daily clarifies:
“So if dried plums are just plums with the water taken out of them, why do they lower our colon cancer risk while fresh plums don’t? Not only does dried plum retain both soluble and insoluble fiber from its original form, but it also contains more sorbitol than fresh plums.”5
Far more than just a tasty snack, these juicy little fruits are loaded with flavonoid polyphenolic antioxidants, primarily lutein and cryptoxanthin, as well as neochlorogenic and chlorogenic acid, which can help prevent cell damage from oxidation of lipid molecules.
All cell membranes, including those in your brain, are mainly composed of fat-containing lipids, found to inhibit LDL cholesterol oxidation and making them a significant factor in helping prevent chronic disease.6
A Comparison of Nutritional Attributes Between Plums and Prunes
Plums contain 26% of the reference dietary intake (RDI) in vitamin C; 13% in vitamin K; and 11% in vitamin A, or retinol, as well as iron, potassium, thiamine, riboflavin and calcium, plus vitamin B6 and niacin to metabolize one of their most serious drawbacks: high natural sugar and carbohydrate content.
As for prunes, a 1-cup serving gives you 87% of the RDI of vitamin K. The Guardian notes that soluble fiber helps slow down the absorption of glucose, which stabilizes blood sugar levels.7
Because prunes are a concentrated source of the nutrients and phytonutrients found in plums, their antioxidant potential is six times that of the fresh fruit. Prunes are also significantly higher in antioxidants than many other dried or fresh fruits or vegetables. Comparing the two, Healthy Eating observes:
“Although most of the vitamin C in plums is destroyed during the drying process, prunes contain significantly higher concentrations of most of the other nutrients found in the fresh fruit.
One cup of pitted prunes provides 129 percent, 36 percent, 27 percent and 9 percent of the daily recommendations for vitamin K, potassium, vitamin A and iron, respectively. Vitamin K is vital to the function of several proteins involved in blood coagulation, and vitamin A promotes healthy vision.”8
These vitamins, minerals and phytonutrients have several benefits throughout your entire body, including your skin and improved vision due to the high iron, of which a deficiency can cause hair loss.

Save This Article for Later – Get the PDF Now
Fiber: Good for Gut Health and Colorectal Cancer Prevention
Bone health isn’t the only benefit of this oft-neglected fruit, though. Studies indicate dried plums can lower your risk of colon cancer.
One factor that helps give plums and prunes such high marks in this category is fiber, crucial for moving food along smoothly through your colon for elimination, but also the natural chemicals sorbitol and isatin, both helpful for relieving constipation. These three ingredients are why prunes have the (earned) reputation as a laxative. Media outlet Chatelaine notes that fiber:
“Helps to … [optimize] cholesterol by soaking up excess bile in the intestine and then excreting it. Bile is made from cholesterol in the liver in order to digest fat.
When the body excretes bile along with the fiber from prunes and plums, the liver must use cholesterol in the body to make more bile thereby lowering the amount in circulation in the body. Soluble fiber may also inhibit the amount of cholesterol manufactured by the liver in the first place.”9
Plums contain 2 grams of fiber in a 1-cup serving, which also helps produce beneficial gut microbiota. One of the big differences between fresh and dried plums is that the dried version contains 12 grams of fiber, which, compared to fresh plums, is about half of the RDI needed for an entire day (although I believe about 50 grams per 1,000 calories consumed is ideal).
According to Alimentary Pharmacology and Therapeutics, prunes are even more effective than psyllium as a laxative.10 Plus, the sorbitol pulls moisture into your digestive tract to help bring about a bowel movement.11 That’s where its effectiveness as a colorectal cancer preventive comes in.
More Benefits From Plums and Prunes
An online resource called Colon Cleansing and Constipation recommends stewed prunes to alleviate constipation, or infrequent bowel movements. Eating them regularly can help prevent subsequent stomach pain and hemorrhoids. All of these can become serious enough to necessitate surgery.
Aside from skin cancers, colorectal cancer is the third most common cancer in the U.S. It encompasses both rectal and colon cancer, which together have stricken around 140,000 people in the U.S., and more than 50,000 die from it every year, according to the American Society for Gastrointestinal Endoscopy.12
Medical Daily mentioned one study that found eating dried plums can help lower your risk for colon cancer by maintaining good gut bacteria in your colon, adding that “a diet high in [certain] red meats can increase colon cancer risk while a diet high in fruits … [and] vegetables … can reduce colon cancer risk.”13
A FASEB Journal study backed up the gut bacteria benefit, noting that their data supported their initial hypothesis:
“Diet is known to alter metabolism and composition of colon microbiota, which has major implications for disease prevention and treatment … The hypothesis tested by this experiment was that consumption of dried plums would promote retention of beneficial microbiota and patterns of microbial metabolism throughout the colon, and that by doing so would reduce colon cancer incidence.”14
Fructose in Plums and Prunes
It takes around 4 pounds of fresh plums to produce 1 pound of dried plums, and both are very versatile. You can chop them up to add to raw grass fed yogurt, blend them in smoothies and shakes and add them to salads and vegetable dishes. In fact, just about anything you use raisins for, prunes are a tasty, healthy alternative.
Eating plums and prunes may also help alleviate problems related to obesity, heart disease and diabetes. However, whether it’s fresh plums or dried prunes you crave, make sure you consume these in moderation, as they both contain high amounts of sugar. Nutritionist Anshul Jaibharat cautions:
“Prunes are high in natural sugar, so too many may not be good for people watching their weight. After all, excess of anything is stored as fat in your body. Prunes have such high nutritional values ensuring that you can eat just one piece and still gain measurable nutrients.”15
However, the sorbitol, which is a sugar alcohol, is not a source of ethanol, the substance found in alcoholic beverages. It’s a natural substance found in many fruits and vegetables, and is about 50% as sweet as sugar.16
Plums are often used to make the French form of Armagnac, a quickly distilled version of cognac with a raw, earthy body. They also end up soaked in brandy for several desserts, including brûlée. The sugar (and, for the former, alcohol) content in these, however, is considerable and outweighs the nutritional benefits that the fruit provides.
Additionally, prune juice is often loaded with high-fructose corn syrup and, even if it’s not, will still be a significant source of fructose without the fiber benefits, so be aware that consuming the whole fruit is preferable.
- 1 Ageing Res Rev. 2009 April;8(2):122-7
- 2 BMJ. 2010 September 1;341:c4444
- 3, 11, 15 NDTV May 11, 2016
- 4 Osteoporos Int 27, 2271–2279 (2016), Abstract
- 5, 13 Medical Daily September 29, 2015
- 6, 9 Chatelaine January 15, 2016
- 7 The Guardian February 16, 2013
- 8 Healthy Eating
- 10 Alimentary Pharmacology and Therapeutics April 13, 2011
- 12 Gastrointestinal Endoscopy Volume 63, Issue 4, April 2006, Pages 546-557, Introduction
- 14 FASEB Journal April 2015
- 16 Livestrong, October 3, 2017
The Silent Epidemic of Excess Iron
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/03/10/high-iron.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola March 10, 2024
STORY AT-A-GLANCE
- High iron is an under-recognized health threat. There’s a general lack of awareness in the medical community regarding the potential health risks associated with high iron levels
- A ferritin level above 100 typically means you’re either inflamed, have high iron, or both. A level above 200 is considered pathological. The higher your ferritin level, the shorter your lifespan. You’re also more likely to die of a heart attack and cancer
- Left untreated, high iron levels can cause liver damage and an increased susceptibility to certain diseases, including infections and cancer
- Lab tests that can help diagnose iron-related conditions such as hemochromatosis include a full iron panel, a complete blood count (CBC) test, gamma-glutamyl transferase (GGT), and a comprehensive metabolic panel to ensure you have sufficient liver enzymes. Measuring your copper and ceruloplasmin levels can also be helpful
- The easiest way to lower your iron is to donate blood on a regular basis. Natural supplements such as curcumin, silymarin and alpha-lipoic acid can also help prevent from continuing to accumulate iron from your food
In this interview, Christy Sutton, D.C., reviews the dangers of excessive iron. While most doctors look for iron deficiency, few ever pay attention to elevated iron. Sutton is the author of two books, “Genetic Testing: Defining Your Path to a Personalized Health Plan: An Integrative Approach to Optimize Health,” and “The Iron Curse, Is Your Doctor Letting High Iron Destroy Your Health?”
Iron plays an important role in health, especially for children and young adults. Without sufficient iron, you’re not going to be able to form red blood cells and certain proteins in your mitochondria that are responsible for producing energy. On the flip-side, an excess of iron can cause significant damage.
A Silent Epidemic
Sutton’s interest in iron has been “lifelong” she says, as she struggled with low iron while her husband has a genetic anomaly that causes him to have elevated iron levels. So, she has personal experience with both ends of the spectrum.
“I have Crohn’s [disease], celiac, and lost part of my small intestine due to Crohn’s when I was 16,” she says. “Because of that, I have to take a bile sequestrant. Then, being menstruating female who’s had a child, low iron has been something that I have been watched very closely for and I had to take iron a lot.
Like a lot of clinicians, when I came into practice, I seemed to be more hyper-focused on people’s problems that were my own problems. I dealt with iron issues. So, I wanted to watch my patients’ iron levels closely. Then I realized, ‘Oh, not everybody is low. A lot of people actually have high iron.’
It wasn’t until I was writing my first book, ‘Genetic Testing: Defining Your Path to a Personalized Health Plan,’ that I discovered the hemochromatosis genes. I realized that my husband had a hemochromatosis gene, and I realized that that was why I kept telling him to donate blood.
His doctor would order iron labs, ferritin, CBC, and he would get elevated iron often, high ferritin. He was developing high liver enzymes and his red blood cells were getting high as well, which is a common issue with people that have too much iron …
He went to a gastroenterologist, because he was trying to figure out why his liver enzymes were high. I thought it was the high iron, but that was presented to the gastroenterologist and dismissed. So, they went down this rabbit hole of misdiagnosing him with autoimmune hepatitis.
Later we went to a hematologist where we figured out he had hereditary hemochromatosis. So, it’s not something that’s particularly difficult to treat. Removing blood, diet supplements, things like that can help.
But once I got really savvy about looking for the genes and the labs combined, I realized that this is a silent epidemic that is not really being talked about. I would tell people, ‘You have a problem with high iron,’ and then they would often go and get a second opinion.
Their second opinion would say, ‘You’re fine. Don’t worry about it,’ which is a common issue where people are getting high iron labs that should warrant more investigation and then they’re just getting dismissed.”
How to Lower Your Iron Level
I have beta thalassemia, a hemolytic anemia that results in a high turnover of red blood cells. My red blood cells only live about two months, rather than the normal three months. As a result, my iron tends to accumulate because of the rapid turnover. So, while I do not have the hemochromatosis gene, it results in similar problems. I inherited it from my father, who had a ferritin level close to 1,000 by the time he was diagnosed. Ideally, it should be below 40.
One of the supplements he tried was inositol, also referred to as hexaphosphate or IP-6, but it did nothing. I rapidly came to the conclusion that the supplements typically recommended for high iron are useless and potentially even dangerous, because they prevent you from doing what is really helpful, which is to remove iron through regular phlebotomies.
The most effective way to lower your iron is to donate blood two to four times a year. If losing 10% of your blood in one sitting is problematic for you, then you can remove blood in smaller amounts once a month on the schedule I have listed below. If you have congestive heart failure or severe COPD, you should discuss this with your doctor, but otherwise this is a fairly appropriate recommendation for most.
| Men | Postmenopausal Women | Premenopausal Women |
| 150 ml | 100 ml | 50 ml |
As it turns out, Sutton did not include IP-6 in her book, as she couldn’t find any research to back up the claims. She doesn’t dismiss all supplements, however. One of the most helpful, in her view, is curcumin.
“Clinically, I have seen curcumin’s ability to lower iron almost to a fault,” she says. “It’s annoying to me, because I can’t take curcumin for inflammation because it makes me low in iron. But for people that are high in iron or even inflamed with high iron, high ferritin, that’s a great place to start, because curcumin binds to iron.
It also has all of these other wonderful health promoting properties. It’s so good for your brain — it actually helps remove excess iron from the brain and other organs, the heart, liver, spleen.
So, unlike other iron chelators that might be used pharmaceutically, it doesn’t have all these possible negative side effects, but it works very effectively. I mean, I’ve seen it be used in hereditary hemochromatosis patients to lower iron without blood removal … Now, people that have really high iron might need 3 grams a day, which can create diarrhea. So, you have to look at other potentially limiting factors.”
She also recommends taking curcumin with an iron-rich meal, such as shellfish or red meat, to inhibit iron uptake. Other supplements that help bind iron include silymarin, (an extract from milk thistle). It too is very good for hemochromatosis patients, because it lowers iron and helps protect and repair the liver. Another thing that binds to and lowers iron is alpha-lipoic acid. It’s also great for protecting nerves and lowering blood sugar.
“I don’t think silymarin lowers iron quite as much as curcumin, but it’s still a significant way to lower iron,” she says. “The best way to take these — to lower iron — is take them with iron-rich meals. If you want to take them just for medicinal properties but not to lower iron, take them away from iron-rich meals.”

Download this Article Before it Disappears
Health Risks Associated With High Iron
The health risks of high iron are manifold and include an elevated risk of skin infections and skin cancer. I suspect high iron may actually be a catalyst when it comes to skin cancer, along with high linoleic acid (LA) intake. LA is oxidized by iron, creating something called lipofuscin, which is basically iron attached to oxidized LA.
A more common term for lipofuscin is liver spots. So, liver spots are a dermal representation of oxidative damage to LA by high iron. Similarly, skin cancer is likely driven by a combination of high LA and high iron. Ancestral LA levels were below 2%. Today, the average is around 25%. If you had normal ancestral levels, you could have higher iron yet not get as much damage.
Understanding Hemochromatosis
There are several potential diagnoses related to iron, including iron deficient anemia, copper deficient anemia, iron overload and hereditary hemochromatosis, and getting to the correct diagnosis can be tricky.
“The nice thing is that you can always fall back on labs,” Sutton says. “You don’t want to just use symptoms to guide you, because if you’re using symptoms, then this person is well far down a pathological path that you could have potentially stopped years ago, if not decades before.”
Starting with hereditary hemochromatosis, this is when you have inherited one of three hemochromatosis genes, which causes increased iron absorption by decreasing hepcidin, a liver protein. If you have the hemochromatosis gene, you don’t make as much hepcidin, causing you to absorb more iron.
That can become pathological, because over time, you just keep absorbing more and more iron, until your body finally runs out of places to put it. The first place that gets overloaded is your liver. After that, your body will store the iron in other organs, such as your heart, pancreas, brain, pituitary gland, gonads, ovaries, testes and skin.
Eventually, the iron will go everywhere because the human body has evolved to hold onto as much iron as possible. The only way, really, to lose iron is through blood loss. This is why menstruating women have a lower risk for high iron and a higher risk for low iron.
“Having said that, when you start looking at the hemochromatosis genes, all bets are off, because you’ll see females that have these hemochromatosis genes that develop high iron … you will even see children with the hemochromatosis genes that develop high iron,” Sutton says.
“I discovered that in my colleague’s 5-year-old, where predatory hemochromatosis was causing her to have severe neurological problems. That was a very difficult thing to get through because the hematologist didn’t really want to deal with it.
When you look at labs, hereditary hemochromatosis can look very similar to non-hereditary hemochromatosis, which is where you have high iron but you don’t have one of those hemochromatosis genes.
So, for you, you have more of a non-hereditary secondary hemochromatosis, because you have that thalassemia issue where your red blood cells are breaking and letting all this iron out and then you develop high iron with potentially low red blood cells.
That’s common with thalassemia. Some people, they don’t have a thalassemia gene and they develop high iron without hemochromatosis gene, because they’re just eating a lot of iron-rich foods and they’re not losing iron through menstruation. This is usually men.”
How to Diagnose Hemochromatosis
When it comes to lab work, Sutton recommends starting with a full iron panel, a complete blood count (CBC) test, gamma-glutamyl transferase (GGT), and a comprehensive metabolic panel to ensure you have sufficient liver enzymes. Measuring your copper and ceruloplasmin levels can also be helpful.
“The full iron panel has the ferritin, the TIBC [total iron-binding capacity], the UIBC [unsaturated iron-binding capacity], the serum iron and the iron saturation. With hereditary hemochromatosis, you develop high ferritin with a high iron saturation. That combination is hereditary hemochromatosis. So, over 45% iron saturation and high ferritin …
With hereditary hemochromatosis, you’ll see high iron, you’ll see the TIBC go low, the UIBC go low. The serum iron often goes high, and then that ferritin will go high. You’ll often see the liver enzymes go high and it’s common to see the red blood cells, hemoglobin, hematocrit go high.
But that doesn’t always happen. These days, so many are taking testosterone. So, you have to always ask, ‘Are you on testosterone?’ Because that can cause red blood cells, hemoglobin, hematocrit to go high as well …
I always get the GGT as a part of the labs that I order. Occasionally, I will see a high GGT when the AST and ALT, which are the other two liver enzymes, are normal. More often than not, I’ll see a high ALT or high AST. Usually, if they’re not drinking alcohol and they just have high iron, you’re going to see that high ALT.”
What’s the Ideal Ferritin Level?
Sutton recommends keeping ferritin below 100. Ferritin above 100 means you’re either inflamed, have high iron, or both. Studies referenced in her book suggest that anything over 200 is pathological. The higher your ferritin level, the shorter your lifespan. You’re also more likely to die of a heart attack and cancer.
“I feel like 100 is high enough that I’m not swooping everybody in, but low enough that I’m not leaving stragglers out,” she says. “Now, if somebody has a ferritin over 100 with an iron saturation that is in the 40s or higher, then I’m highly suspicious of a hemochromatosis gene and I immediately want to get those hemochromatosis genes tested.
If they have a hemochromatosis gene, then we know why they’re high on iron and we know where this story is going — and it’s not going to be a pretty picture most likely. Then it’s time to refer to a hematologist … and talk to them about how to get iron lower …
The key is, if you don’t have a hemochromatosis gene, then you need to figure out ‘Why does this person have high iron? Do they have a thalassemia gene? Are they just eating a lot of iron?’ And then, ‘Do they have hemolysis for some unknown reason?’ That’s a non-hereditary hemochromatosis situation.
The treatment is basically the same, other than you want to use more of the supplements, go really heavy on the supplements to lower iron. If you have plenty of red blood cells and hemoglobin, then therapeutic phlebotomy is a wonderful place to start.
A lot of times people don’t because they either have a thalassemia issue where their red blood cells are getting chewed up too quickly, or they have lost so much blood so quickly because their doctors are just trying to get the iron down that they become low in hemoglobin or red blood cells. Rather than waiting for months for that to recover, you could be doing the supplements to lower the iron.”
The Link Between High Iron and Cushing’s Disease
Sutton’s husband also developed a pituitary tumor that was causing him to have high cortisol (Cushing’s disease). “Ultimately, I think the high iron created a lot of oxidative stress on his pituitary gland,” Sutton says. The only reason he was diagnosed early enough to save him was that they’d been checking his cortisol and DHEA on a regular basis.
“Periodically, they would jump up and then go back down. Then when the hemochromatosis got properly treated and the DHEA was still high, we were like, ‘Why is this happening?’ So we went to the endocrinologist and I said, ‘I’m worried my husband has Cushing’s.’ She was like, ‘He doesn’t have Cushing’s. He doesn’t look like somebody with Cushing’s. His hemoglobin A1C is normal.’
Five months later, he’s having surgery to remove the pituitary tumor. The reason I say that is because for years, he was told, ‘You just need to exercise and lose weight.’ His problem was not exercise. He had a pituitary tumor and hemochromatosis. Hemochromatosis was destroying his liver and his brain and his heart and everything else, and the pituitary tumor was causing him to have high cortisol, which made him look overweight.”
I believe progesterone may be one of the best ways to treat Cushing’s disease, as it very effectively blocks cortisol. Other natural substances that will inhibit cortisol include aspirin, DHEA, pregnenolone, emodin, vitamins A and D, gelatin or glycine, and niacinamide.1
The normal dose for progesterone is 25 to 50 milligrams. For Cushing’s, I would recommend about 300 mg. It’s virtually impossible to overdose on progesterone and there are no downsides to it. One caveat is that you need to administer it correctly to gain the optimal effects.
Avoid creams, pills and suppositories. Instead, mix pharmaceutical grade progesterone with the contents of one natural vitamin E capsule. Mix it with a paperclip or tiny spoon until all the powder is dissolved, then rub it on your gums. Vitamin E is the only natural compound that dissolves progesterone completely. For guidance on how to pick a good vitamin E supplement, see “The Four Hormones Most Adults Need More Of.”
Understanding Iron-Deficient Anemia
As explained by Sutton, iron deficient anemia is a serious issue. Children born of women with iron-deficient anemia have significantly higher risk of low IQ, ADD, ADHD and other neurological issues that often do not go away with age.
“Many kids suffer from low iron, because they eat a lot of calcium rich foods. Calcium binds to iron, and then you get low in the iron. Maybe they’re picky eaters, they’re growing rapidly. So many kids are not being checked for their iron levels and they’re being diagnosed with ADHD when their problem is actually just low iron, because if you don’t have enough iron, you can’t make dopamine. So, low iron is a serious issue.”
People with iron-deficient anemia will typically have high TIBC and UIBC, as their bodies are trying to mobilize more iron. Serum iron and iron saturation will be low and ferritin will typically be below 30.
“Now, iron deficient anemia is more complicated in many ways because the question is, why are you low in iron?” Sutton says. “There’s so many reasons that you can be low in iron. Are you just not eating enough? Are you not absorbing it? I think the most common reasons that people develop low iron is because they have a GI bleed. They have intestinal malabsorption issues, maybe undiagnosed celiac disease.
There is a gene that can cause you to be more likely to have low iron. I have that gene and that gene actually causes you to make more hepcidin. With iron-deficient anemia you’ll also see low red blood cells sometimes, low hemoglobin and low hematocrit. MCH [mean corpuscular hemoglobin] might get low, MCV [mean corpuscular volume] might get low.”
Copper Deficiency Can Cause Both Low and High Iron
One common cause for iron-deficient anemia is a deficiency in copper. Paradoxically, lack of copper is also a common cause for iron overload. Sutton explains:
“The reason for that is because copper is necessary for two key enzymes. The first one is called hephaestin and the second one is called ceruloplasmin. Hephaestin is in the lining of the gut, the intestinal lining. Copper is necessary for iron to be absorbed in the gut lining. So, without copper, you will not absorb iron and you will develop iron deficient anemia.
Once iron has been absorbed in the gut lining by hephaestin, it passes it off to ceruloplasmin, which is the second copper-rich enzyme. Ceruloplasmin basically then allows that copper to transfer in and then move throughout the body. So, without ceruloplasmin, iron gets stuck in the tissues. It’ll get stuck in the digestive system, it’ll get stuck in the retina, it’ll get stuck in the brain, it’ll get stuck in the liver.
So, you develop iron overload in the tissues. But eventually, if you’re low in copper long enough, you might then become low in iron, and then you don’t end up with all this extra iron in the tissues. The solution is take copper to fix that problem. That’s the way you solve copper-deficient anemia.
Copper-deficient anemia looks very similar to iron-deficient anemia if you’re looking at the iron panel. You’ll have a high TIBC, high UIBC, low serum iron, low iron saturation, low ferritin. You’ll also potentially see low neutrophils and low white blood cells, because you need copper to have normal immune function as well. So, you might be more at risk for infections.
Then of course you can look at the ceruloplasmin. I don’t find ceruloplasmin to be the easiest lab to look at, because it’s an inflammatory marker … If you’re taking hormones like estrogen or birth control or you’re pregnant or you’re just inflamed or have an infection, ceruloplasmin can jump around and go high.
If you have a low or low-normal ceruloplasmin, and then you take copper and ceruloplasmin goes up, that’s a good sign that you didn’t have enough copper.”
How to Get More Iron Into Your Diet
The best way to get iron is through your diet. Shellfish and beef are iron-rich foods with highly absorbable iron. That’s key, because there are two types of iron: heme iron and non-heme iron, the latter of which is not very absorbable. Heme iron is found in animal products while non-heme iron is found in vegetables such as spinach.
“If you’re not eating iron-rich foods like red meat, then you’re more likely to get low in iron if that is something that you struggle with,” Sutton says. “If you struggle with being high in iron, maybe you don’t want to eat as many of those things or maybe you just want to remove blood and supplement accordingly, so that you continue to eat those things.
The form that I like if I’m going to go to a supplement is ferrous peptonate, which I found to be the gentlest on my gut but also get the iron levels up. I really don’t like ferrous sulfate, which is the most common given iron. I don’t think it works very well, and it tends to create a lot of stomach pain. I always have to take my iron with food and sometimes I’ll add copper or vitamin C to it. If I don’t take it with food, it’s really going to upset my stomach.”
More Information
To learn more, check out Sutton’s books, “Genetic Testing: Defining Your Path to a Personalized Health Plan: An Integrative Approach to Optimize Health,” and “The Iron Curse, Is Your Doctor Letting High Iron Destroy Your Health?”