Breathing
now browsing by category
Mindless Habits That Fuel Overwhelm and Exhaustion
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/03/28/energy-draining-habits.aspx
Analysis by Dr. Joseph Mercola March 28, 2025

STORY AT-A-GLANCE
- Daily habits like poor posture, shallow breathing and cluttered environments significantly drain your energy without your awareness
- Workspace chaos such as cluttered desks, too many browser tabs and constant interruptions scatters focus and depletes mental energy throughout the workday
- Task management problems like leaving things unfinished, overplanning and letting small tasks accumulate create mental weight that exhausts you
- Lifestyle choices including intense TV shows and bright lights before bed disrupt your circadian rhythm and emotional balance, leaving you tired
- Sensory overload from environmental stimuli and ignoring your body’s needs overwhelm your nervous system, requiring intentional breaks and stress management
Do you often feel wiped out, even after sleeping all night? You’re not the only one — lots of people deal with low energy every day. The sneaky part? Your daily habits could be the culprits, quietly draining you without you noticing.1 From putting up with household clutter to staying up with bright lights, these little things add up fast.
But here’s the best news: you can turn it around with easy fixes. Let’s explore why these habits tire you out and give you simple tips to feel better. Soon, you’ll spot these energy-drainers in your own life and know how to kick them out — starting right now.
Your Body’s Energy SOS — Habits That Wear You Down Physically
Your body needs steady care to keep going strong. Disregard that, and you’ll feel slow and tired. Here are three habits that zap your physical energy — and how to stop them.
• Sitting like a couch potato — Slouching feels cozy, but it’s secretly exhausting. When you hunch over, your muscles strain to hold you up, and your lungs can’t fill with air. It’s like lugging a heavy bag the wrong way all day — it wears you out. Sit up straight with a cushion or a good chair to help your back. Stretch a couple times during the day, and you’ll feel a lift.
• Breathless and drained — Ever catch yourself barely breathing when you’re stressed? Quick, shallow breaths don’t give you enough oxygen, leaving you foggy and worn out. But instead of taking deep, vertical breaths that trigger the stress response, practice horizontal breathing.
This means expanding your ribcage sideways rather than lifting your chest upwards. Horizontal breathing promotes relaxation by avoiding the activation of stress pathways in your nervous system.
• Why it matters and what to do — These habits creep in because they’re so normal — slumping in your seat or holding your breath when you’re busy. But they drain your body little by little. Start small: sit less, adjust your chair or set a breathing reminder. You’ll feel stronger soon!
Chaos at Your Desk — How Your Workspace Steals Your Energy
Your work area either keeps you sharp or leaves you fried. These three habits might be tiring you out at your desk — here’s how to take back control.2
• Clutter chaos — A desk covered in papers and knick-knacks scrambles your brain. It’s like cooking in a kitchen with no space — stressful and slow. Clutter pulls your focus, so everything takes longer and tires you out. Take 10 to 15 minutes a day to tidy up — put things away and keep only what you need. A clean desk clears your head too.
• Tab overload — A screen full of open tabs is like juggling too many balls — you’ll drop one eventually. Your brain gets frazzled switching between them, draining your energy quick. Every hour, ask: “Which tabs do I need right now?” Close the rest or save them for later. Fewer tabs mean more focus and less burnout.
• Phone call fatigue — Jumping to answer every call yanks you off track. It’s like someone pulling you around while you walk — you stumble and lose steam. Switching focus fast wears your brain out. Let calls wait unless they’re urgent — pick a time each day to deal with them. Send a quick text to check if it’s a good time, and save yourself the hassle.
• Taming your workspace — A jumbled desk, too many tabs and constant calls turn work into an energy trap. Imagine a calm setup: neat, focused and quiet. Pick one fix to start — like clearing your desk tonight — and watch how much better you feel by day’s end.

Save This Article for Later – Get the PDF Now
Task Trouble — When Your To-Do List Drains You Dry
How you manage tasks can keep you pumped or leave you swamped. These three habits overload your brain — here’s how to lighten up.
• Leaving things half-done — Like pausing a movie before the end — keeps your brain hooked on it. Experts call it “attention residue,” and it tires you out juggling old and new information in your head. Finish what you can before switching, or write down where you stopped. That quick note frees your mind for the next thing.
• Overthinking the future — Planning every detail weeks ahead sounds smart, but it stresses you out. It’s like stuffing a suitcase so full you can’t carry it. A jammed schedule stops fun and rest, draining you dry. Plan the big stuff (work, appointments), but leave some days free for whatever. Less planning means more energy.
• Letting small tasks pile up — Ignoring tiny tasks — like replying to a text or changing a bulb — builds a mental mess. It’s like snow piling on your roof; it gets too heavy to handle. All those “I’ll do it later” thoughts drag you down. Knock out quick jobs (under five minutes) right away, or list them and hit them weekly.
• Getting back in control — Unfinished tasks, overpacked plans and a growing to-do pile weigh your days down. Picture the opposite: finishing tasks, keeping plans loose and clearing small jobs fast. Try one tweak this week — like jotting tasks down — and feel your energy climb.
Everyday Choices That Tire You Out
Your daily routine can sneakily sap your energy. Are these three habits hiding in your life? Let’s dig them out and fix them.3
• TV that wears you out — Love gripping shows? They wear you down with an emotional rollercoaster. It’s like running a feelings marathon — you’re beat after. Big emotions, even fun ones, tire your brain. Switch to lighter shows or save dramas for weekends when you can relax after.
• Bright lights before bed — Bright lights and blue light at night fool your brain into thinking it’s day. It’s like sleeping with the sun in your face — hard to rest! This throws off your sleep and your circadian rhythm, leaving you tired the next day. Block blue light in the evenings by using blue-light blocking glasses, installing blue light filters on your devices and opting for warmer, dimmer lighting in your home as it gets dark.
• Following bad-fit advice — Adopting tips that don’t suit you often backfires. Advice that doesn’t fit wastes your effort. Figure out what works for you — like tweaking your diet or skipping a rule that feels off. Custom fixes save your energy.
• Reclaiming your spark — TV binges, late-night lights and mismatched advice gradually drain. Start with one swap, like dimming lights tonight, and keep going.
Sensory Overload — When Your Senses Steal Your Energy
Your brain is a processing powerhouse, but it has limits. When sensory input overwhelms it, you’re not just tired — you’re truly overstimulated. Here are three habits that lead to sensory overload, and how to reclaim your calm.4
• Ignoring your limits — Pushing through crowded spaces, loud events or visually busy environments without breaks overwhelms your sensory processing. Recognize your triggers and plan breaks in quiet, low-stimulus environments.
• Neglecting your nervous system — Failing to manage stress leaves your nervous system primed for overload. Chronic stress heightens sensitivity to sensory input. Practice stress reduction and slow breathing regularly, even when you’re not feeling overwhelmed.
• Ignoring physical needs — Not eating healthy, or not getting enough sleep, leaves your body less able to cope with sensory input. Focus on proper sleep, healthy carbs and daily exercise to build up your resilience.
• Taming your sensory overload — A constant barrage of sights, sounds and stimuli turn daily life into a sensory minefield. Start by identifying your triggers and implementing simple strategies to manage your sensory input. Even small changes, like taking regular breaks, make a significant difference in your overall well-being.
Breaking Free from Harmful Habits
Remember, feeling tired all the time isn’t your fate. Whether your desk stresses you out, tasks stack up or your routine throws you off, small changes flip the script. You don’t have to fix it all now — start with one or two that feel familiar. Little steps add up quick. Look at your day: which habits ring a bell? Write them down and pick one to tackle this week. You’ll be shocked how much pep you get back.
FAQs — Common Questions About Energy-Draining Habits
Q: What’s the best way to stop feeling tired all the time?
A: Check your habits first. Sitting tall, decluttering your environment and proper breathing lift you fast. Try tidying your desk and dimming lights at night — small wins work. Remember, consistency with these small adjustments is key to sustained energy improvements.
Q: How does a messy desk affect my energy?
A: Clutter messes with your focus, making tasks harder and longer. A clean desk keeps your brain calm and saves energy. Therefore, regularly dedicating short periods to organization significantly enhances your focus and reduces mental fatigue.
Q: Why do I feel drained after binge-watching shows?
A: Intense shows stir big emotions, tiring your brain out. Go for lighter options or save dramas for when you can rest after. Consider balancing screen time with activities that promote relaxation, such as reading or gentle stretching.
Q: Can bright lights really make me tired?
A: Yes, nighttime bright light and blue light trick your brain into staying up, ruining sleep. Dim lights at sunset and avoid blue light from screens at night for better rest and energy. Implementing a consistent evening routine with dimmed lighting helps regulate your circadian rhythm and promote better sleep quality.
Q: How can I manage tasks without getting overwhelmed?
A: Finish what you start and do small tasks fast. A quick list or note keeps your head clear. Prioritizing tasks and breaking larger projects into smaller, manageable steps prevents feelings of being overwhelmed.
Why Proper Breathing Is the Key to Optimal Health
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/07/proper-breathing.aspx
Analysis by Dr. Joseph Mercola April 07, 2024
STORY AT-A-GLANCE
- Dysfunctional breathing habits are typically developed in response to some type of emotional trauma. The trauma gets embedded in your brain circuits, and when you encounter triggers, they activate specific breathing habits, some of which may significantly lower your carbon dioxide (CO2) concentration level
- The higher the CO2 concentration you can maintain while remaining within the biologically normal CO2 concentration range, the greater the likelihood that your breathing is supporting your health and performance
- Breathing techniques such as belly breathing, deep breathing and Buteyko breathing may not address breathing triggers or why you developed an inappropriate breathing habit in the first place
- When you overventilate you get numerous physiological changes. As a result, overbreathing can trigger a wide variety of physical and psychological changes, which can be reversed by implementing breathing behavior analysis learning techniques
- Breathing behavior analysts help you become conscious of your breathing habits, what’s triggering them and how to resolve them. This is important, as improper breathing habits can unconsciously sabotage your health
The interview above features Peter Litchfield, Ph.D., who is, in my view, one of the best breathing experts in the world. I’ve taken his breathing course, which gave me a deep appreciation for what he’s teaching. None of the breathing experts I’ve interviewed before compare to Litchfield when it comes to understanding respiratory physiology and its impact on your health.
Many of you who read this article may react in fear because the information may challenge your understanding of what others have told you to be true and you struggle trusting yourself to guide this new belief process. I strongly encourage you to watch the interview in its entirety. I believe it will alleviate most of these fears as Dr. Litchfield is an excellent teacher in helping people trust themselves. It would be easy to react negatively to this information and choose not view the interview, but I believe that would be a major mistake. I sincerely hope you avoid making that choice.
According to Litchfield — who has decades of clinical training in both respiratory physiology and behavioral psychology — dysfunctional breathing habits are typically developed in response to some type of emotional trauma. It gets embedded in your brain circuits, and when you encounter this trigger, it activates them and lowers your carbon dioxide (CO2) level.
You may have been getting a hint over the last few months that I really value CO2. It’s probably one of the most important molecules in your body. I’m going to go deep into this in the coming year, as strategies to increase your CO2 are probably some of the best things you can do to optimize your health.
The higher the level you can get within the biological normal optimal range, the better. Most of us are not even close to that. And, if you think you’re already breathing well because you’re belly breathing, deep breathing, or doing Buteyko breathing, you’re in for a surprise, because there’s a lot more to optimal breathing than learning to slow down, lessen or deepen your breathing.
Behavioral Physiology
Litchfield has a long and varied professional history, but his primary interest is behavioral physiology, a field in which physiology is viewed as a programmable system. As he explains, your physiology self-regulates:
“It learns, in essence. It does something and there’s a consequence, and based on that consequence it changes what it does. Physiology collects information, stores information. It uses information on all levels, not just on the level of the brain, but even on a cellular level. It’s collecting and using data. That’s what we call learning, ultimately; that is, physiology is behavioral, it’s psychology in action.
Physiology really is psychophysiological because it’s a learning system … One of the things that’s important in the work that we do in breathing behavior analysis, based on this, is that people need to learn to form a working partnership with their bodies …
The body is a learning, living system. The day the first cell came into existence, psychology was born. That is really such an important thing to understand. It’s not just ‘you’ who’s doing the breathing. Your body is doing the breathing. These aren’t just genetic or organic considerations. The body gets programmed constantly by virtue of what it does, and what results from what it does, and breathing is no exception.
Look at the habits we learn in our lives. Look at my hands. I’m moving my hands right now. Look at my head and how I move it. I learned this unconsciously. I’m a whole collection of amazing habits, thousands of habits that come into play at just precisely the right place and time.
So, the right thing happens at the right time, and I don’t even have to think about it. That’s the nature of a habit. But they don’t always go well, they can go very wrong.”
Habits Serve a Purpose
As explained by Litchfield, habits always serve a purpose. You don’t engage in a habit unless it serves you or your physiology in some way. This is why it’s so important to form a partnership with your body, to explore your habits, and how or why you learned them in the first place.
In a sense, you could say that your physiological system is part of your unconscious or subconscious mind, or an expression thereof. The task is to become conscious of what’s going on because your breathing habits may be unconsciously sabotaging your health.
“So, what we’re really focused on in our work is observing and learning about breathing as a behavior,” Litchfield says. “We’re not using breathing as a technique where you manipulate breathing so you can relax, or you manipulate breathing to achieve some otherworldly experience where you dissociate.
There are all kinds of reasons that people implement breathing techniques for presumed positive outcomes … Our work isn’t about breathing techniques.
Another thing that’s very important, is that there is a trigger for every habit. Triggers are not there all the time. They show up at specific times. For example, in the statistics pointing the larger cities of the United States, like New York City, Chicago, Los Angeles, where surveys suggest that about 60% of the ambulance runs are a result of symptoms brought on by dysfunctional breathing.
And it’s not as if this person is breathing dysfunctionally all the time. It’s that at that particular moment, they breathe this way, that then precipitates these symptoms.
They don’t understand where these symptoms and deficits are coming from. They don’t think of their breathing. They call 911, if you’re in the United States, and they end up in [the] emergency [room] … A lot of what our work is about is identifying these habits.”

Save This Article for Later – Get the PDF Now
What Is a Breathing Habit?
So, how do you identify a breathing habit? There are many components to look at, including the following:
• Motivation — Behavior is motivated by something. There’s motivation behind all habits, and any one of them can be tied up with your breathing.
• Behaviors — You need to identify the exact behavior involved. For example, you may be aborting the breath, meaning you inhale before you’ve fully exhaled.
In most cases, it’s rooted in a subconscious fear about not getting enough air. Whatever the cause, there’s motivation embedded in the behavior. Aborting the breath and inhaling early may serve the breather by reducing worry or anxiety about not getting enough air.
However, when you inhale too soon, air hunger sets in — a feeling like you can’t get enough air — and that can trigger the very anxiety the habit is trying to avoid.
“It’s nothing to do with oxygen,” Litchfield says. “It’s about claustrophobia. So, this person then develops a kind of claustrophobia that’s now embedded in the breath.
You’ll find some people constantly reaching, trying to get that one good breath. They may suffer with air hunger for an extended period of time. As they breathe out, they abort [the breath] constantly, trying to get a satisfying breath as soon as possible.”
• Outcomes — What are the outcomes of your learned breathing behavior, and how are those outcomes serving you? For example, when you start taking larger breaths, you may think you’re going to get more air.
You may feel like you’re in charge and in control, and that keeps you going. But what happens is you lose CO2 without realizing it. You may experience symptoms that you and your healthcare providers may misinterpret and attribute to unrelated causes.
In reality, you need far less air than you think. For every liter of blood you can move through your lungs, you can move 20 liters of air. But you only need 1 liter of air. So optimal breathing is usually not about getting enough oxygen. It’s about regulating the CO2 concentrations in your extracellular body fluids, like blood plasma.
What Deep Breathing Does to Your Body
Contrary to popular belief, deep breathing does not improve oxygenation. When you’re deep breathing, blood flow to your brain actually decreases as a result of a tightening of the blood vessels (vasoconstriction) in the brain.
Additionally, the cytoplasm in your red blood cells can become too alkaline and the hemoglobin carried by the red blood cells can become unfriendly, that is, less willing to give up the oxygen it carries to the tissues that need it. So, deep breathing actually contributes to an oxygen deficit already in progress as a result of vasoconstriction.
The vasoconstriction occurs because the primary vascular purpose of CO2 is vasodilation. When you have sufficient CO2 in your system, it will open your blood vessels much more effectively than nitric oxide, because nitric oxide has a dark side. It binds to Complex IV in your mitochondria and shuts down the electron transport chain. So, ideally, you want the vasodilation to be done by CO2 rather than nitric oxide.
So, the outcome of overbreathing is loss of blood in the brain, loss of oxygen, loss of glucose and electrolyte changes in the brain that then lead to setting the stage for lactic acidosis in neurons (brain cells). “Most people, lay or professional, have no idea that this is going on,” Litchfield says.
These brain changes, in turn, tend to trigger disinhibition where emotions — oftentimes anger or fear — are discharged. This release of emotions can serve you by allowing you to cope with a challenging situation or environment. Overbreathing (breathing that results in a CO2 deficit) leads to an outcome (a reinforcement) that serves you and is thus a “solution” to a perceived problem, a successful coping mechanism.
“Maybe they’ve come from a very traumatic kind of a background, and the only way they could really cope with it is to get angry,” Litchfield says. “But usually there is fear operating in the background …
There are things like this that, when you overbreathe, you get a symptom, a physiological change, and people have learned to respond to that change in their own unique ways. Some people, for example, when they get dizzy because they lose oxygen in the brain, when they overventilate, feel like they’re losing control and freak out. They can’t understand what’s going on.
They can’t focus. They don’t remember what’s happening. They feel unable to function. They’re on the verge of a panic attack. The next person goes, ‘Hey, this is kind of cool. I really like this.’ They have a whole different response to it. So, one of the things we’re always looking at are how people relate to the physiological changes brought on by breathing.”
Automatic Reflexes Regulate Your CO2 Level
As explained by Litchfield, your CO2 level is regulated by automatic reflexes. There are receptors in the brain and in the arterial system that are sensitive to CO2 concentration and to the pH of various extracellular fluids, such as blood plasma and interstitial fluids (surrounding cells). There are receptor sites in the arterial system which are sensitive to oxygen concentration but, surprisingly, not in the brain.
This system wasn’t designed to get out of whack just because you get stressed. Provided you haven’t learned bad breathing habits, your breathing optimizes respiration regardless of most circumstances., e.g., while talking.
As explained by Litchfield, breathing regulates acid-based physiology1 in extracellular body fluids. Your body must have the capacity to change your pH rapidly, almost immediately, because if it didn’t, you would be in serious trouble and in could even die. Although bad breathing habits can quickly bring on fainting, for example, there are safety mechanisms that protect us.
“There’s a simple little equation … that addresses how blood pH is regulated by the relationship of carbon dioxide concentration with bicarbonate concentration; ‘together they regulate acid-based balance from breath to breath.’
The carbon dioxide is controlled by the way you breathe. So as soon as you start to take over breathing, you take the control away from the reflexes, the result of which can be determined by doing a breathing behavior analysis.
You might be OK because in the background breathing and respiration are being coordinated properly, but maybe not, like when I’m eating and talking, I’m breathing. They have to be coordinated and linked. This is behavior. They get linked.
Sometimes they get out of sync and then people are really in trouble. They’re struggling whenever they eat. Their breathing is all wrong. When they’re talking, the breathing goes wrong.
They get real lightheaded when they’re talking because they’re overventilating. They’re constantly trying to take another breath while they’re talking to people … What’s happening is that they’re losing carbon dioxide. They’re getting completely disoriented, can’t function …”
Do You Overbreathe?
Symptoms of low CO2 (hypocapnia), caused by overbreathing, include but are not limited to:
| Headache | Nausea and vomiting |
| Abdominal symptoms and bloating | Fatigue |
| Muscle pain and weakness, tetany, hyperreflexia, spasm, tingling in the hands and lips, numbness, trembling and difficulty swallowing | Cardiovascular changes like palpitations, tachycardia, arrhythmias, angina, ECG abnormalities |
| Cognitive changes, including attention deficit, difficulty learning, poor memory and brain fog | Symptoms involving consciousness, such as dissociation, disconnecting from your environment, disconnecting from people, fainting and hallucinations |
| Emotional changes associated with the reduction of blood flow in the brain | Personality and self-esteem changes |
If you frequently suffer any of these symptoms, it is possible that you may be struggling with hypocapnia, meaning low CO2 levels, and the No. 1 reason for hypocapnia is a poor breathing habit in response to all kinds of habit triggers, such as stress. The solution in this case is to identify the faulty habitual breathing behaviors and then correct them.
Optimizing Your CO2 by Relearning Better Breathing Habits
You can very accurately measure your CO2 concentration with a tool called a capnometer, the wellness-educational version of it known as a CapnoTrainer:
“Being able to measure carbon dioxide is obviously the best of all worlds. There are ways you can look at overbreathing without a capnometer, but it’s quite limited. It may be that you’re not aware of how you’re being influenced, so it’s very difficult without a capnometer or CapnoTrainer.
But ultimately, the idea is not to need technology. The idea is you understand that you’ve learned habits and that you identify what those habits are, their components, their motivation, their outcomes, your belief systems and all kinds of things around it so that you can learn about who you are from a breathing perspective.
It’s not about a breathing technique. This is about learning techniques, about how you become a different being when it comes to the way that you breathe, and your habits optimize respiration, your habits optimize acid-based physiology.
If you want to have your CO2 looked at from a perspective of habits that you may have learned, you can rent a device, which makes it affordable for many people. A CapnoTrainer is different in a certain way than a capnometer. A capnometer technically is used in medicine, in surgery and in critical care, emergency medicine and so on.
But a CapnoTrainer is used to learn about your breathing. How are you breathing? How is it affecting you? What habits do you have? How can you learn new habits? That kind of thing. So you can rent these devices and you can also buy them. There are different versions of them.
There are professional, basic and personal versions of them. They’re all software-based, and you can operate these instruments on your cell phone and on tablets and Apple computers, PC computers, whatever, and really get to know your breathing in detail …
What breathing behavior analysts do is they help you do that. Now, however, you can learn to do it on your own. We have a book out that can walk you through that … The idea is to try to help you optimize your functioning. So many people just don’t realize that they’re breathing dysfunctionally and they attribute their symptoms to all kinds of other sources completely unrelated to breathing.
And so do the health care professionals because they don’t know about it either. They’re trying to figure out where these symptoms are coming from, but they don’t think about the breathing …
The breathing techniques out there generally don’t address habits. They may, by accident, address a habit and then give credit to the technique rather than understanding it’s about some kind of embedded learning that has occurred in the process — that fear was addressed, for example.
But they may think, well, it’s the slowness of breathing. Breathing slow is really good. And so it’s [about the] parasympathetic nervous system, and that’s why it worked, when in reality what it was about was that you lost your fear associated with the end of the exhale, for example, because of the technique they were using.
But people aren’t focusing on it that way … They aren’t looking at the experiential side of it, which is key to understanding breathing behavior.”
Trust Your Body
Again, your body knows how to breathe. The only time you get into problems is when you unconsciously override it with a learned breathing habit that throws the system out of whack. So, trust your body.
“That’s totally fundamental,” Litchfield says. “That’s what we work on — helping people build trust in that system. And that’s what I was talking about at the very beginning about partnering with your body. That partnership is vital.
You’re not a victim of your body. You’re in the body. This is who you are. You own this. You own your breathing. You’re not a victim of your breathing. And that’s often a problem. People think they’re a victim of all of this.”
Why Most Breathing Techniques Don’t Address Your Health Problems
While we’ve already mentioned this, it bears repeating. What Litchfield is talking about is not learning a specific set of breathing techniques. It’s not about the technique per se. It’s about understanding why your breath gets dysregulated and how new habits can be learned. In regard to the Buteyko technique, for example, he comments:
“Most issues around breathing, when it comes to hypocapnia, are acute. It isn’t chronic. Buteyko [breathing] is really limited to [chronic overbreathing]. Secondly, you have to ask yourself, where did that hypocapnia come from in the first place? Why is this person breathing like that, that you now have to train them to habituate to a higher level of CO2? How did that happen? What’s the history of that?
And if the history is that this is a way I can control my wife, if you’re overventilating so you can get angry to control your environment, what good is Buteyko [breathing] going to do? That person isn’t going to raise their CO2 level. They want it down so they can get angry.
So you have to address the motivation behind the behavior and what the outcomes are that sustain it. Just because you can habituate to a higher level of CO2 doesn’t mean you’ve addressed the problem. The problem is the habit. You want to identify the habit, help the person through it, help them understand where it came from and what they can do about it.
And that may have a significant philosophical impact on them as well, their belief system about their physiology, the trust in their system and so on. So the [Buteyko breathing technique is] limited because you’re not addressing history of the breathing. You’re not addressing any of these various factors that we’ve been talking about. You’re just looking at the CO2 level — ‘My god, it’s too low. We need to raise it.’
Another problem with Buteyko is that they don’t measure it. Some do, but it’s not part of their curriculum. We have a lot of people who graduated from our program who are Buteyko workers and they measure it. When you think you’ve been successful with your client, you need to see that the CO2 actually went up.
If it didn’t go up, you weren’t successful. So it’s very important to be able to assess it right from the start because Buteyko, when they do their assessment, they’re looking at correlational findings …
On the other hand, they really do a great job because when people get … comfortable with allowing the breath to sit out there for long periods of time, they can build trust, and they may find the reflex in it. Identifying the reflex is what ultimately builds trust because you can feel it kick in.
If you can find that reflex, then you’ve won a significant part of the battle. And there’s a good chance that can happen because of what the Buteyko people do. Desensitization to the transition time eliminates anxiety and air hunger during the transition time by doing Buteyko, so that’s helpful.”
The Breathing Behavior Analysis Procedure
In the course I took with Litchfield, he provided many impressive practical examples. One was of a young woman, about 19 years old, whose CO2 level dramatically decreased when they began her breathing interview. Among the symptoms she’d indicated on the checklist was that she would get dizzy a lot, and when she gets these dizzy spells, she’d become frightened.
“So, we’re talking and I see her CO2 level go down. I say, ‘Are you feeling dizzy right now?’ And she says, ‘Yeah, as a matter of fact, this is exactly how I feel in these kinds of situations.’ ‘Well, look at your CO2 level. Look what happened here.’
This is what we call transactional psychophysiology. We’re interacting with the person around their physiology, and they’re seeing what’s happening while they’re behaving in the way they are. So, we explore that together. And then we do all kinds of testing together depending on who the person is and what the issues are.
A good example might be, we’ll have them overbreathe on purpose. Now, this isn’t as simple as it sounds. You need to do it the right way. There’s a real right way to do it, and there are wrong ways to do it. We have someone overventilate on purpose. And what happens when you do that, they start to get symptoms, and they start to get deficits, and they’re there and they’re focusing on their experience.
They’re not talking. I’m the one who’s doing the talking. I’m asking them questions to think about the answers, not to interact with me, but just to think about the answers to the questions.
I’ll ask questions like, ‘Are there any emotions coming up right now? Are there any memories that are being triggered right now? Does this remind you of anything in your current life circumstances? Does this remind you of something that happened to you in the past?’
And I have a lot of information before I do this. I have this form. So they’re not just random questions. They’re really specific. They’re about that person and their lives and what we’ve uncovered together. And then what often happens is, they’re trapped. They can’t get out. They’re breathing that way and the CO2 level simply does not come up no matter what they do. And this is what happens in their real life situation when they get trapped …
As I work with them, I use certain kinds of experiential paradigms that I implement so they can raise the CO2 level. The symptoms go away and they’re amazed. Someone will say something like … ‘My God, it seemed like I wasn’t even breathing. I feel so much better and I was hardly breathing at all. How can that be?’
It’s because their belief system was that they weren’t getting enough oxygen and couldn’t possibly be OK breathing with these very small kinds of breaths.
In fact, this is what allowed the trap to break open so they could allow those reflexes to operate, to trust the system so they get to where they need to be from a respiratory point of view. And this may all happen in one short session, if you know what you’re doing.”
A Quick Rescue Method
A good test that can tell you if your symptoms are due to a CO2 deficiency is to breathe into a paper bag. If the symptoms disappear, you know hypocapnia and hence overbreathing is the problem. Never use a plastic bag, as it can cause suffocation. Always use a paper bag, about 6 inches by 15 inches. If it’s too small or too large, it won’t work.
Place the paper bag over your nose and mouth and hold it in place with your hands as you breathe into it. The CO2 will accumulate in the bag, thereby raising your CO2 level as you breathe it in.
“I remember a woman we met in Georgia, in the United States, my partner Sandra and I. She had this irritable bowel syndrome kind of problem with major anxiety around it, so she wanted some advice. There wasn’t much I could offer her, but one of them was a paper bag.
About four months later she wrote back and said her whole life had completely changed. She no longer had to suffer with these episodes. She hadn’t had any for months, and she couldn’t believe it. But of course, she was dependent on the bag. She wasn’t learning a new habit. She just grabbed the bag when she needed it, unfortunately.”
Negative Practice
Another simple technique, which is part of the core of Litchfield’s program, is something called “negative practice.” Litchfield explains:
“What you do is you become an expert at performing the bad habit. So you’re not a victim of the bad habit. You own it. You take ownership of it because you can do it whenever you want to. And if you can do it whenever you want to, you can disengage it.
So you learn to do it, disengage it, do it, disengage it. And there are specific ways of doing this. We use biofeedback in this whole process. That’s an important part of it. So, then you’re not afraid anymore of the symptoms because you can turn them on, you can turn them off, you don’t really care. It’s not a big deal.
In that process, you get highly reinforced. Again, that’s how physiology works. The outcome of what it does determines what it can do within the potential it has. The idea is that there’s a positive outcome for restoring good respiration.
On the other hand, it can be much more challenging because if someone is overbreathing to get angry at their husband, that’s a more complex issue. You have to address that. So it can be very simple or it can be quite complex, but nevertheless, it works wonders for people.”
More Information
To learn more, visit:
- Better Physiology Ltd. at betterphysiology.com for information about and purchase of CapnoTrainer instrumentation for personal and professional applications
- RespiMatters at www.CapnoLearning.org for information regarding online breathing behavior analysis services available worldwide
- Professional School of Behavioral Health Sciences at www.bp.edu and www.e-campus.bp.edu for information regarding professional training in breathing behavior analysis
- Breathing Science Inc., a nonprofit publisher, at www.theBSJ.org, where you can purchase the book “CapnoLearning: An Introductory Guide
Average Person Asleep by 10 but Still Wakes Up Tired
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/04/average-bedtime-irregular-sleep.aspx
Analysis by Dr. Joseph Mercola April 04, 2024

Story at-a-glance
- According to a poll of 2,000 adults, the average time most people go to bed is before 10 p.m. — 9:54 p.m. to be exact
- Despite this reasonable bedtime, many still wake up feeling tired; this may be because your night’s rest is only restorative if you’re able to fall asleep and stay asleep
- Among adults, 4 in 10 say they’re bad sleepers, while another 60% say their nighttime routine needs work
- People with the most irregular sleep had the highest dementia risk and were 53% more likely to develop the condition than those with more regular sleep patterns
- The glymphatic system, which your brain uses for detoxification, is particularly active during sleep, which may actually serve to kickstart the system
Getting to bed too late is often blamed for feeling groggy the next morning. But according to a poll of 2,000 adults, the average time most people go to bed is before 10 p.m. — 9:54 p.m. to be exact.1
Despite this reasonable bedtime, many still wake up feeling tired. This may be because your night’s rest is only restorative if you’re able to fall asleep and stay asleep. It turns out, however, that regardless of bedtime, 4 in 10 say they’re bad sleepers, while another 60% say their nighttime routine needs work.
Further, only 24% said they sleep better when they go to bed earlier. A spokesperson for furniture retailer DFS, which commissioned the poll, explained, “Our study has shown how the actual time we go to bed can have a real impact on our sleeping routine as a whole. The hours of sleep we get is of course important, but the way we prepare ourselves and get ‘into the zone’ of sleep is also vital.”2
This isn’t just a matter of waking up feeling energized, either. Proper sleep is essential to your physical and mental health, and if you skimp on it enough, a number of diseases can result.
Irregular Sleep Increases Dementia Risk by 53%
Going to bed and waking up around the same times each day is a key part of healthy sleep hygiene. It may also be important for protecting your health, according to research published in Neurology.3
“Sleep health recommendations often focus on getting the recommended amount of sleep, which is seven to nine hours a night, but there is less emphasis on maintaining regular sleep schedules,” study author Matthew Paul Pase of Monash University in Melbourne, Australia said in a news release. “Our findings suggest the regularity of a person’s sleep is an important factor when considering a person’s risk of dementia.”4
The study involved 88,094 participants with an average age of 62 years and looked into how sleeping patterns, specifically how regular they are, might be connected to the risk of developing dementia. Researchers tracked sleep patterns using a special method that measures if they were asleep or awake at the same times across several days.
Over about 7.2 years, 480 people developed dementia. It turned out that both very irregular sleep patterns and overly consistent sleep patterns (sleeping and waking up at exactly the same times every day) were linked to a higher risk of dementia compared to those with moderately regular sleep patterns. This relationship was U-shaped, meaning both extremes were associated with increased dementia risk.
Further, in a smaller group who had brain scans, those at the extremes of sleep regularity tended to have smaller amounts of brain gray matter and hippocampal (a part of the brain important for memory) volume. That said, people with the most irregular sleep had the highest dementia risk and were 53% more likely to develop the condition than those in the middle.5
Those with the most regular sleep, meanwhile, did not have a reduced dementia risk compared to the middle group, suggesting even moderate improvements in sleep regularity may benefit brain health.
“Effective sleep health education combined with behavioral therapies can improve irregular sleep patterns,” Pase said. “Based on our findings, people with irregular sleep may only need to improve their sleep regularity to average levels, compared to very high levels, to prevent dementia. Future research is needed to confirm our findings.”6
Sleep Jump-Starts Nightly Brain Detoxification
It’s worth nothing that your brain uses sleep as its time to flush out toxins and metabolic waste — compounds that could otherwise accumulate and contribute to neurodegenerative disease. Most of your body uses the lymphatic system for this purpose. As Forbes explains:7
“In short, a specialized ‘sewerage’ infrastructure called the lymphatic system. This is made up of various vessels and channels that, like our circulatory system, spread across the entire body. These vessels are filled with a fluid called lymph, which flows through tissues and organs, washing up and collecting debris as it goes.
Dirty lymph is eventually drained into the blood vessels, where it is carried to the kidneys and liver for final filtration and removal.”
In your brain, however, it’s the glymphatic system that removes waste products, acting as a “brain-wide metabolite clearance system.”8 By pumping cerebrospinal fluid through your brain’s tissues, your glymphatic system flushes waste from your brain back into your circulatory system and liver for elimination.
It operates similarly to the lymphatic system in the rest of your body but is specialized for the unique environment of your brain and central nervous system. The term “glymphatic” combines “glial cells,” which are cells in your brain that bring nutrients to neurons, and “lymphatic,” reflecting its similarity to the body’s lymphatic system.
The glymphatic system facilitates the removal of metabolic waste products from the central nervous system via a network that involves the perivascular space — the space surrounding blood vessels — cerebrospinal fluid and glial cells.
The glymphatic system is particularly active during sleep, which may actually serve to “kickstart” the system,9 highlighting the importance of a good night’s sleep for brain health. Scientists with Washington University School of Medicine in St. Louis10 also revealed that during sleep, neurons generate electrical signals that trigger rhythmic brain waves, propelling cerebrospinal fluid through the brain
These electrical waves may boost the function of the glymphatic system, helping cerebrospinal fluid penetrate deeper into the brain and pick up waste, enhancing the cleaning process.

Save This Article for Later – Get the PDF Now
Your Heart Also Needs Proper Sleep
Your heart, like your brain and overall health, needs at least seven, if not eight, hours of sleep to function optimally. In fact, getting enough sleep each night, and quality sleep at that, is associated with cardiovascular risk and research also found that sleep is connected with subclinical atherosclerosis,11 the early stages of hardening and narrowing of the arteries.
Researchers with the National Center for Cardiovascular Research in Madrid, Spain used coronary ultrasound and CT scans to measure the artery health of close to 4,000 middle-aged adults and analyzed it according to their sleep duration and quality.
Those who slept for less than six hours a night (very short sleep duration) were 27% more likely to have subclinical atherosclerosis than those who slept for seven or eight hours a night.
While atherosclerosis is often associated with heart disease, it can occur in any of your body’s arteries, with symptoms depending on which arteries are affected. Atherosclerosis in your brain can lead to stroke, for instance, while the condition in your kidneys can lead to high blood pressure or kidney failure, and atherosclerosis in the arteries in your arms and legs may lead to peripheral artery disease.
This implies, then, that proper sleep could play a major role in disease prevention via its role in preventing atherosclerosis alone. The effect is so significant that an accompanying editorial noted that, with additional trials to confirm, sleep could be placed “alongside diet and exercise as a key pillar of a healthy lifestyle.”12
A Simple Way to Fall Asleep Faster
Anxiety and racing thoughts can make it difficult to fall asleep, even if you’re already in bed. When you become stressed, your breathing pattern and rate change naturally, but it’s important to be conscious of how triggers like this change your breathing habits — and what to do to resolve them.
The 4-7-8 breathing method, known for relaxation and promoting restful sleep,13 may help. Also known as “relaxing breath,” the 4-7-8 breathing method involves a specific pattern of breath control developed by Dr. Andrew Weil, based on ancient yogic techniques, including pranayama.14
Using this breathing method before sleep may trigger a relaxation response in your body, shifting you from a state of heightened stress — sympathetic nervous system activation — to a state of calm, or parasympathetic nervous system activation. This transition helps reduce stress and anxiety, which are common culprits behind sleep disturbances.
Focusing on the breathing pattern also encourages mindfulness, which involves being present in the moment and can help quiet your mind. This focus can distract you from the day’s stresses and worries that might interfere with sleep.
This specific pattern of breath control may also improve the balance of oxygen and carbon dioxide in your blood. Further, slowing down your breath can lead to deeper, more restful sleep by promoting physiological changes conducive to sleep, such as reduced heart rate and muscle relaxation.
It’s important to understand, however, that most breathing exercises, or techniques, aren’t a long-term solution because they don’t address the habits contributing to dysfunctional breathing in the first place. To get to the root of the problem and learn proper breathing, breathing behavior analysis learning techniques are typically necessary. If you’d like to try the 4-7-8 breathing method, however, it’s straightforward, as follows:
1. Prepare — Sit or lie down in a comfortable position. Close your eyes and take a moment to relax your body. Place the tip of your tongue against the tissue behind your upper front teeth and keep it there throughout the practice.
2. Inhale — Breathe in quietly through your nose for a count of 4 seconds.
3. Hold — Hold your breath for a count of 7 seconds.
4. Exhale — Exhale completely through your mouth, making a whoosh sound, for a count of 8 seconds.
This breathing cycle is repeated for four full breaths, but you can work your way up to eight repetitions over time.
How to Get a Good Night’s Rest
As mentioned, maintaining a regular bedtime and wake time is useful for brain health and overall sleep hygiene. But it’s just one piece of the puzzle to getting a good night’s sleep. I’ve compiled 50 top sleep tips you can use to fall asleep faster and stay asleep longer, which include sleeping in complete darkness.
Light (even that from a night light or alarm clock) can disrupt your internal clock and your production of melatonin, thereby interfering with your sleep. Also, keep the temperature in your bedroom cool, between 60 to 68 degrees F, and eliminate electromagnetic fields. Ideally, shut down the electricity to your bedroom by pulling your circuit breaker before bed and turning off your Wi-Fi at night.
Establishing a relaxing bedtime routine is also useful. This may include meditation, aromatherapy, essential oils, journaling or a massage from your partner. The key is to find something that makes you feel relaxed, then repeat it each night to help you release the tensions of the day and prepare for restful slumber.
- 1, 2 StudyFinds July 8, 2022
- 3 Neurology. 2024 Jan 23;102(2):e208029. doi: 10.1212/WNL.0000000000208029. Epub 2023 Dec 13
- 4, 5, 6 EurekAlert! December 13, 2023
- 7, 9 Forbes March 8, 2024
- 8 Scientific Reports February 2, 2018
- 10 Nature February 28, 2024
- 11 J Am Coll Cardiol. 2019 Jan 22;73(2):134-144
- 12 Journal of the American College of Cardiology January 2019, Volume 73, Issue 2
- 13 CNN September 16, 2022
- 14 Pocket January 3, 2022
The Underappreciated Role of Carbon Dioxide in Health
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/03/03/co2-benefits.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola March 03, 2024
STORY AT-A-GLANCE
- CO2 is typically thought of as nothing more than a harmful waste product of respiration, but it’s actually a driver of mitochondrial energy production, and it improves the delivery of oxygen into your cells
- One of the simplest ways to optimize your CO2 is by breathing properly. Most people tend to over-breathe, which causes you to expel too much CO2. Proper breathing involves breathing less and breathing slower. Both of these allow CO2 to build up, and that appears to be part of why breathwork has such wide-ranging benefits
- To have sufficient CO2 production, you need healthy mitochondria because CO2 is produced exclusively in the Krebs cycle in the mitochondria. If you have mitochondrial dysfunction, if you’re hypothyroid or have high levels of inflammation, then you will not be producing enough CO2
- When your CO2 is too low, your body reverts to an “emergency” vasodilator, nitric oxide (NO). Drawbacks of elevated NO include peroxynitrite species formation and pseudohypoxia. NO also damages the polyunsaturated fats (PUFAs) in your cells, and inhibits energy production
- CO2 combats cancer development by lowering the pH of the cell, thereby allowing extra water to be excreted. This is the opposite of linoleic acid (LA) and estrogen, both of which suck water in and cause the cell to swell. Cellular swelling is a feature of cancer cells
In this interview, repeat guest Georgi Dinkov reviews the role of carbon dioxide (CO2) in health. CO2 is typically thought of as nothing more than a harmful waste product of respiration, but it’s actually a driver of mitochondrial energy production, and it improves the delivery of oxygen into your cells.
While this may come as a shock to most people, of all the strategies I know of to increase life extension, CO2 is one of the most effective longevity interventions available. There really isn’t anything that comes close, other than a low linoleic acid diet and reducing estrogen dominance.
Unfortunately, virtually no doctors understand this. The now deceased Ray Peat, a biologist and physiologist who developed the bioenergetic theory of health,1 was one of the few who understood it inside and out, and actually recommended its clinical use.
I wrote an article about this that featured his lecture on CO2, which I watched six times as it catalyzed my interest in the topic. At the time I found his video there were fewer than 2,000 views on YouTube. You can find it by going to YouTube and typing in Ray Peat CO2.
Proper Breathing Is Important for Optimal CO2 Levels
One of the simplest ways to optimize your CO2 is by breathing properly. Unfortunately, bad advice is rampant in the breathing arena as well. The problem is that most people tend to over-breathe, which causes them to expel (breathe out) too much CO2, resulting in respiratory alkalosis. Chronic CO2 deficiency will also contribute to premature death.
In a nutshell, “proper” or life-extending breathing involves breathing less and breathing slower. Both of these allow CO2 to build up, and that appears to be part of why breathwork has such wide-ranging benefits.
“As it turns out, carbon dioxide, even though medically it’s mostly viewed as a waste product of respiration, is actually the thing that protects us from oxygen’s well-known toxicity,” Dinkov explains.
“In fact, if you speak to people who work in trauma or in the intensive care unit, when they have to revive people that are in shock or have suffered some kind of ischemic attack, they will tell you that the premature delivery of oxygen, or delivering too much oxygen … is actually what kills most patients after they come out of the initial shock stage.
The introduction of too much oxygen too quickly creates this massive cytokine storm and inflammatory reaction, and one of the reasons [for that] is that the cells are hypermetabolic — they’re not producing sufficient carbon dioxide, so they’re not able to utilize the oxygen properly.”
Forgotten Truths
It’s rather surprising that the benefits of CO2 have become forgotten considering its historical use. Asian cultures, for example, have a long history of using carbonated water for its health benefits.
The Romans recommended taking baths in naturally carbonated water for all kinds of ailments but especially arthritis, infertility and psychiatric ailments, and this practice extended well into the Middle Ages when monks prescribed it. To this day many visit natural hot springs, and the likely benefit in many of these springs is the CO2 content of the water.
In the 20th century, Russian scientists did loads of research on CO2, and to this day, many Russian clinics offer CO2 baths and other CO2 treatments. There’s even a suit that can be filled up with CO2, which then diffuses into your tissues. You’ll start feeling hot very rapidly and this is a sign of vasodilation, which is one of the cardiovascular effects of CO2.
It’s been shown that CO2 can, over the long term, even reverse arterial calcification. It can also reverse many other signs of and damage caused by the aging process.

Download this Article Before it Disappears
Mitochondrial Dysfunction Inhibits CO2 Production
The key, though, is that in order to have sufficient CO2 production, you need healthy mitochondria, because CO2 is produced exclusively in the Krebs cycle in the mitochondria. If you have mitochondrial dysfunction, if you’re hypothyroid or have high levels of inflammation, then you will not be producing enough CO2.
When your CO2 is too low, your body reverts to an “emergency” vasodilator, nitric oxide (NO). There are three types of nitric oxide:2 neuronal nitric oxide synthases (nNOS); endothelial NOS (eNOS); and inducible NOS (iNOS). Low CO2 triggers iNOS. The problem with that is that now you’re overproducing NO, which is not ideal. Dinkov explains:
“Most of the eNOS … stays in the actual blood vessel. iNOS also spills into the blood. That’s kind of the purpose of iNOS because the primary purpose of nitric oxide in the body is to fight pathogens. It’s a reactive nitrogen species.
It’s produced for only two reasons, either as an emergency vasodilator, or if the immune system senses an invasion from pathogens, specifically bacteria and viruses, in which case iNOS is activated.
The reason iNOS is bad is because the nitric oxide does not stay localized. It’s made available systemically because you want to affect all blood vessels, and that’s what happens when you don’t have sufficient amounts of carbon dioxide production. So, if you don’t have [enough] CO2, you will have elevated NO.
But with NO, nitric oxide, you have a lot of other bad things happening. It’s a highly reactive molecule. It can form peroxynitrite species. It can damage the polyunsaturated fats (PUFAs) in the cells, no matter where they are.
Nitric oxide itself can form a covalent bond with something called cytochrome c oxidase [Complex 4 in the electron transport chain], which is the rate limiting step of the oxidative phosphorylation …
You want to break that bond because otherwise your oxidative phosphorylation is inhibited. Methylene blue can do it, magnesium can do it, carbon dioxide can do it, near-infrared light and some quinols.”
Another significant problem associated with elevated NO is pseudohypoxia, because you have oxygen in the cells but it cannot be utilized because No impairs Complex IV in the electron transport chain.
CO2 prevents this by dissociating the covalent bond between NO and Complex IV. Hence, oxygenation is optimized when sufficient CO2 is present. So, to summarize, CO2 keeps your blood vessels supple without the drawback of blocking Complex IV.
The Bohr Effect
Needless to say, optimal delivery of oxygen is crucial for good health. Oxygen from the air binds to hemoglobin when you inhale and enter your blood circulation. This bond is relatively strong. To break that bond and deliver the oxygen where it’s needed, you need CO2. This is known as the Bohr Effect.
Basically, the Bohr Effect describes the process in which CO2 weakens the bond between oxygen and hemoglobin so that the oxygen can separate and enter into the tissues.
As the hemoglobin releases the oxygen, it binds to the CO2 instead. The CO2 is then expelled through your outbreath. Without enough CO2, you will not be able to liberate sufficient amounts of oxygen from hemoglobin.
A Note on Oxygen Saturation
On a side note, a pulse oximeter measures the amount of oxygen in your blood. However, if your CO2 is extremely low, it could still read 100% saturation because you’re not dissociating the oxygen. It’s circulating in your bloodstream but cannot be used.
The major factor that determines your tissue oxygenation is how much CO2 you’re producing. If you’re hypermetabolic, if your mitochondria are not working, then you’re oxidizing mostly fats, which produces less CO2 per molecule, so you’ll be deficient in CO2.
In the past (going back 100 years ago or so), the test for seizure susceptibility was hyperventilating. The doctor would instruct you to breathe through your mouth very quickly for 30 seconds, and if seizure symptoms emerged, it was a sign that you have insufficient CO2, as that’s what’s causes the seizure activity.
How CO2 Can Combat Cancer
Another important aspect of CO2 is that it lowers the pH of your cells, thereby allowing extra water to be excreted. This is the exact opposite of linoleic acid (LA) and estrogen, both of which suck water into your cells which causes the cells to swell. Cellular swelling, aside from being the cause of edema, is also a feature of cancer cells. So, you don’t want your cells to retain excess fluids. Dinkov explains:
“Because carbon dioxide is a Lewis acid, it’s an electron withdrawing agent, even though it doesn’t directly bind them like a quinol. If you look at the structure, it’s very similar to a quinol. It’s a carbon atom with two carbonyl groups, and the quinol is very similar. They usually have a ring and two or more carbonyl groups.
Lewis acids drop the pH of the cell, which automatically decreases the cell’s affinity for water. Which means you’re going to be excreting some of that extra water of the cell.
It’s not a coincidence that linoleic acid has multiple double bonds. It’s much more hydrophilic than the saturated fats, which lack the double bonds. Any time you have an increase of intracellular pH, you have increased affinity for water. The moment water streams in, that’s a signal for de-differentiation and metosis (division). If this process continues uncontrollably, we basically get cancer.
Conversely, when you excrete water, the cell becomes acidified and a little bit dehydrated, so to speak. Then you’re getting high amounts of differentiation. You’re also increasing the affinity of the intracellular proteins for potassium and magnesium, while decreasing their affinity for sodium and calcium. In fact, when carbon dioxide is produced and streams out of the cell, it draws calcium and sodium with it.
If you’re not producing sufficient amounts of carbon dioxide, you’re also probably not producing sufficient amounts of ATP, because carbon dioxide and ATP go hand in hand; they’re signs of good mitochondrial function. ATP has affinity for magnesium, but if you don’t have sufficient amounts of ATP, you’ll have more ADP, which is the degraded version.
ADP has an affinity for calcium. So low metabolic rate, by definition, means cellular excitotoxicity, cellular alkalinity and cellular division, because of the lack of carbon dioxide and the lack of the ATP. ATP always exists in the body in a complex with magnesium. So, if you’re taking magnesium but not producing sufficient amounts of ATP, it will not become bioavailable. But the production of ATP is tied to the production of carbon dioxide.
Carbon dioxide also increases the uptake of serotonin into the platelets, so producing sufficient amounts of carbon dioxide will lower your extracellular levels of serotonin.
It also increases the uptake of histamine, a very highly inflammatory mediator. Its transport also depends on carbon dioxide and on sodium as well, just like the serotonin … So, almost everything that you do metabolically, in terms of health, depends on the production of CO2. It’s not a waste product.”
Respiratory Alkalosis and Cancer
Cells can only produce a certain amount of CO2 per unit of time, so when you breathe too fast, you overwhelm your cells’ ability to maintain an appropriate level of CO2. As a result, you’ll have excess oxygen circulating in your blood stream, but because the CO2 production cannot keep up with the amount of CO2 you exhale, you end up with respiratory alkalosis.
Respiratory alkalosis also increases intracellular water uptake, as just described, and as the pH of the cell increases, it causes overproduction of several inflammatory mediators, including lactate, which is another hallmark of cancer cells.
“Cancer cells are highly alkaline, they’re overproducing a lot of lactate and they have a very high uptake of water,” Dinkov says. “In fact, I think the word tumor is a Latin word which meant swelling.
You can reduce the swelling of the tumor to a tremendous degree simply by either increasing delivery of CO2 around the tumor, if it’s on the surface, or increasing uptake of CO2 through a CO2 bath or drugs that increase the levels of CO2 in the blood.”
Drugs that increase CO2 include carbonic and hydrate inhibitors such as acetazolamide, which decrease the degradation of CO2, allowing more CO2 to build up in your blood.
CO2 Benefits Your Entire Body
A nearly 150-year-old medical book describes the many uses and health benefits of CO2 that were known at the time. It basically included the entire body, and an extensive list of ailments of the day, including:
| Dementia | Psychiatric disorders like mania |
| Dysentery | Fistulas |
| Fibrotic conditions | Whooping cough |
| Tuberculosis | Rhinitis |
“Really, every condition you can think of, both physiological and mental, can be remediated, and in many cases cured, by increasing endogenous CO2 production and decreasing degradation,” Dinkov says. Migraines, are another common ailment that can be addressed with CO2. In many cases migraines are due to overbreathing causing a lack of CO2 that constricts the blood vessels in your brain.
Exogenous CO2 Delivery Methods
While it’s obviously important to optimize your endogenous (internal) production of CO2, exogenous delivery or supplementation will definitely produce the greatest benefits, as you can deliver far greater amounts than your body can produce. Such strategies include:
| Breathing into a paper bag | Drinking carbonated water and other carbonated beverages |
| CO2 baths | A special suit into which CO2 is pumped |
| Hyperbaric administration | Taking small amounts of baking soda in your drinking water |
One of our readers, LSquare, shared their experience with bag breathing in treating their hypertension a few days ago and I thought you would enjoy their story in case you did not see it in the comment section.
“Exercise, regular walking, and upping my potassium helped to lower my hypertension to the 120-130’s. However, I started doing the paper bag breathing when Dr M first mentioned it last month, and the results could not be more amazing. My systolic readings now are regularly now less than 110, and my diastolic ones are in the 50s.
I just had my annual physical 2 weeks ago, and my Dr. REMOVED hypertension from my records. Bad things are almost never removed from your ‘permanent record’. And I’d only done the CO2 breathing for several days before that appt. I implore you to try it if you suffer from High BP. It’s free, and it only costs you 4-6 minutes a day.”
A book written in 1905 by Achilles Rose, M.D. discusses various methods of delivery including inhalation, irrigation and rectal insufflation. It contains case reports of it being used for asthma, whooping cough, dysentery, colitis, rectal fistulas, rhinitis and ear infections. It is a fascinating read.
The Biology of Carbon Dioxide
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/11/18/carbon-dioxide-biology.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola November 18, 202
STORY AT-A-GLANCE
- Carbon dioxide (CO2) is a driver of energy production, as it improves the delivery of oxygen into your cells. CO2 also helps protect against the harmful effects of lipid peroxidation
- CO2 and lactate have opposing effects. Lactate is the byproduct of metabolizing glucose without oxygen in the cytoplasm. So, where lactate causes problems, CO2 has beneficial effects
- Elevated lactate production is a common theme in diabetes, Alzheimer’s, heart failure, shock and general aging. It promotes inflammation and degrades mitochondrial function. Conversely, low CO2 concentrations have been linked to epileptic seizures, muscle spasms, inflammation, hypothyroidism, stroke and clotting disorders
- All these issues, whether caused by elevated lactate or low CO2, can be successfully treated with CO2 therapies of various kinds, such as CO2 baths (where CO2 is pumped into the tub, much like bathing in carbonated mineral water) or adding CO2 into standard hyperbaric treatment
- Simpler ways to raise your tissue content of CO2 include breathing into a paper bag, having an adequate supply of calcium, and supplementing with salt, baking soda or carbonated beverages
In this 2010 interview, the late Ray Peat, a biologist and physiologist who specialized in the bioenergetic theory of health,1 reviewed some of the key benefits of CO2 and how it works within the human body. This article is a summary of the key points made in that interview.
I apologize for the video quality. The video was recorded 13 years ago, and appears to have been shot on a cell phone. In 2010 the cameras were not very good. However, the audio is fine, and more importantly, this information is really hard to come by since Peat is no longer with us. Only 2,000 people had viewed it when I first saw it.
I watched it four times as it is so good. I’m convinced optimizing your carbon dioxide (CO2) level is one of the most important strategies you can do to slow down degeneration due to aging.
On that point, I will be interviewing one of the leading breathing experts in the world, Peter Litchfield, Ph.D., who will educate us on why most breathing techniques don’t work, as they don’t address the underlying triggered breathing habits that lower CO2.
CO2 Is Crucial for Optimal Health
CO2 is typically thought of as nothing more than a harmful waste product of respiration, and a “pollutant” that endangers the earth by raising global temperatures.
The reality is that CO2 is a driver of mitochondrial energy production, and it improves the delivery of oxygen into your cells. It’s also essential for most life on Earth, plants in particular. In fact, CO2 appears to be a more fundamental component of living matter than oxygen.2 All of this was well-known in decades past, but somehow knowledge about the beneficial effects of CO2 has been suppressed over time.
Importantly, CO2 allows for more efficient energy production in your mitochondria, which is why people who live or spend time at higher altitudes tend to be healthier and have fewer chronic health problems such as asthma. The reason for this is because the pressure of CO2 relative to oxygen is greater at higher altitudes.
A Simple Biohack to Boost CO2
According to Forbes Health, biohacking is “a term used to describe various tips and tricks for enhancing the body’s ability to function at peak performance — and maybe even extend one’s lifespan.”
A biohack for mimicking being at a higher altitude in order to boost CO2 is to breathe into a paper lunch bag for a minute or two. The bag should not be too small or too large (an ideal size is 6 inches by 15 inches, or 15 centimeters by 38 centimeters). Breathe into the bag with your mouth and nose covered until you feel better.
With each exhale, you expel carbon dioxide. By rebreathing the carbon dioxide inside the paper bag, you effectively raise your carbon dioxide level. According to Peat, breathing into a paper bag a few times a day has been shown to bring blood pressure down by as much as 30 points, and stabilize it there after a few days of repetition.

Download this Article Before it Disappears
CO2 and Lactate Have Opposing Effects
As explained by Peat, CO2 and lactate have opposing effects.3,4,5 So, where lactate causes problems, CO2 has beneficial effects.
For example, elevated lactate production is a common theme in diabetes, Alzheimer’s, heart failure, shock and general aging. It promotes inflammation and degrades mitochondrial function. Conversely, low CO2 concentrations have been linked to epileptic seizures, muscle spasms, inflammation, hypothyroidism, stroke, and clotting disorders.
According to Peat, all these issues, whether caused by elevated lactate or low CO2, can be successfully treated with CO2 therapies of various kinds, such as CO2 baths (where CO2 is pumped into the tub, much like bathing in carbonated mineral water) or adding CO2 into standard hyperbaric treatment.
Simpler ways to raise your tissue content of CO2 include breathing into a small paper lunch bag a few times a day as detailed above, having an adequate supply of calcium, and supplementing with salt, baking soda or carbonated beverages.6
Peat tells the story of how he told an individual suffering from transient ischemic attacks who’d gone to the emergency room with stroke symptoms and paralysis on several occasions to drink a soda or carbonated water when the attacks occurred, as the bubbles in carbonated drinks are CO2 gas. “That worked for him,” he said.
CO2 Promotes Efficient Energy Production
Lactate is the byproduct of glycolysis, or nonaerobic respiration. It occurs when your mitochondria are compromised and are unable to metabolize glucose. Instead of pyruvate going to the mitochondria to be burned, it is oxidized to lactate in the cell’s cytoplasm. When this occurs in the presence of oxygen it is called the Warburg Effect, which is major pathway that cancer cells use.
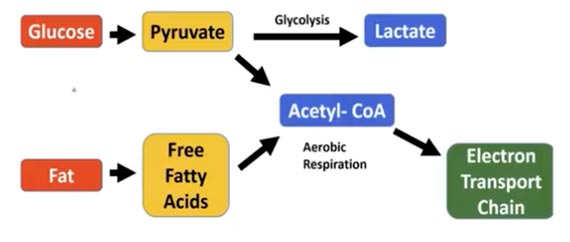
As illustrated in the graph below, glucose can be metabolized in two different ways. When fat intake is too high, glucose is burned though glycolysis, which uses no oxygen and produces lactate. This is a highly inefficient way to produce energy, as it generates only 2 ATP per glucose molecule. And, in the context of this article, no CO2.
When fat intake is in the sweet spot of 15% to 40%, and glucose intake is high enough, it can be burned for fuel in the mitochondria. This generates up to 38 ATP per glucose molecule. In this process, NADH and CO2 are also produced.7
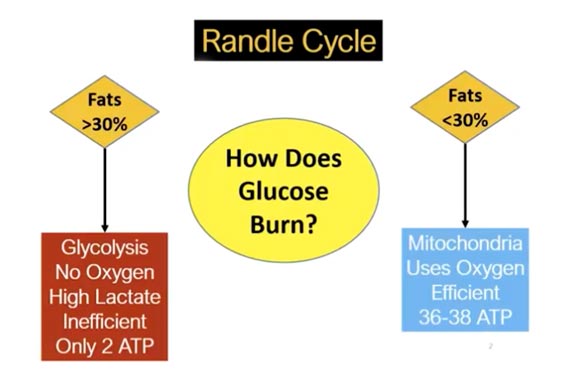
If fat intake is over 40% and the carb intake is below 200 grams per day, the glucose is burned in glycolysis in the cell’s cytoplasm, which produces lactate that suppresses glucose oxidation and shifts metabolism to the burning of fats instead.
Lactate also promotes inflammation and fibrosis. CO2, meanwhile, limits the formation of lactate, increases oxidation of glucose, helps trigger mitochondrial formation (i.e., boosts the number of mitochondria in your cells) and boosts cellular ATP concentrations.8
As explained by Peat, glycolysis products (pyruvate and lactate) compete with CO2 for binding sites inside the mitochondrion. Glycolysis decreases energy production by reducing CO2.
Energy Production Summary
In summary, two key points from all this are:
- 1. The most efficient way to generate cellular energy is to burn glucose in the electron transport chain of your mitochondria (aerobic respiration). In addition to generating up to 38 ATP molecules per glucose molecule (opposed to the two generated through glycolysis), it also generates an estimated 50% more CO2 than fat oxidation.9
In order for glucose to be metabolized in your mitochondria, your dietary fat intake needs to be sufficiently low so as not to inhibit the oxidation of glucose. While there’s no hard evidence on how much fat is too much, I suspect you need to restrict fat to 30% or 40%, depending on your individual needs, to optimize your glucose metabolism. - 2. There are two possible energy states:
- i. A glycolytic stress state in which energy production is reduced by the inhibition of CO2.
- ii. An energy-efficient state in which CO2 is produced and lactate is suppressed.
CO2 Protects Against Lipid Peroxidation
CO2 also helps protect against the harmful effects of lipid peroxidation. Lipid peroxidation10 refers to a process in which free radicals and other harmful oxidants attack lipids (fats) that have carbon-carbon double bonds. Polyunsaturated fats (PUFAs) such as linoleic acid (LA) are particularly prone to this.
The key that many fail to recognize is that lipid peroxidation increases when CO2 levels are low, as CO2 protects the fats from damage. As explained by Peat, when CO2 is low, that’s when PUFAs increase their production of lipid peroxides11 (oxidation products of phospholipids).
Lipid peroxides degrade into reactive aldehydes such as malondialdehyde and 4-hydroxy-2-noneal (4-HNE), which damage DNA and proteins, causing them to malfunction. Lipid peroxidation is known to contribute to conditions such as cancer, atherosclerosis and neurodegenerative conditions, just to name a few.12
Peat cites one experiment in which they showed that when you raise the CO2 in human tissues to three times normal, the amount of lipid peroxides went to zero. So, CO2 has a potent anti-inflammatory effect and effectively protects against lipid peroxidation.
This is an important piece of information, as most people nowadays consume enormously excessive amounts of seed oils that are loaded with PUFAs, and thus have very elevated levels of stored LA in their cells.
As explained in “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” LA is a primary contributor to chronic disease, as it causes mitochondrial dysfunction and promotes inflammation.
Augmenting CO2 in your tissues may be an effective way to limit LA-induced damage while you work to eliminate the excess LA from your tissues and replace it with healthy fats (which can take six or seven years).
How Lactate and CO2 Influence Stress
Peat also goes into an extended discussion involving many separate pieces to explain how lactate and CO2 influence the stress response and other parts of human biology that impact disease, including cancer.
For starters, the cytochrome oxidase enzyme — also known as Complex IV in the mitochondrial electron transport chain, which is what uses oxygen — governs your rate of oxygen consumption.
So, the more cytochrome oxidase you have, and the more active it is, the greater your oxygen consumption. Cytochrome oxidase is also responsible for increasing the total number of mitochondria within the cell as needed to accommodate for increased oxygen consumption.
When you saturate a cell with a very large amount of CO2, you rapidly increase the amount of cytochrome oxidase in the cell, and you boost its activity almost instantly. This shifts the oxidative balance of the cell towards the oxidized state, as electrons are being pulled out of the system. This lowers reductive stress in the cell, which is what you want to do.
In healthy cells, there’s a balance between NAD+ and NADH that is critical for energy production. Conditions like cancer or diabetes disrupt this balance, leading to excess lactate and reduced NAD+. Carbon dioxide is crucial because it prevents excessive lactate production, maintaining a healthy NAD+ to NADH ratio.
CO2 also influences the water balance in cells, supporting an oxidized cellular condition with lowered reductive stress that results in proper oxygen utilization. Hyperventilation, or over-breathing, which reduces CO2, typically leads to overproduction of lactate, contributing to stress and disrupting cellular balance.
CO2 in Emergency Care
Peat also discusses the role of CO2 in emergency care that has the potential to save your life or the life of someone you love. Stroke patients are typically ventilated with pure oxygen to prevent hypoxia-induced brain damage,13 but this isn’t the best way to help these patients.
A ventilation strategy called permissive hypercapnia appears to be far better. Permissive hypercapnia refers to a ventilation strategy employing partial pressures of CO2 that are higher than physiological norms. I have been encouraging those in the hyperbaric oxygen community to explore and adopt this strategy in their hyperbaric chambers. As explained by Peat:
“Quite a few people are now, just in the last few years, starting to talk about permissive hypercapnia … instead of ventilating someone to death [by] giving them pure oxygen. When people aren’t getting enough oxygen to the brain, they’ll give them pure oxygen and then hyperventilate them.
The idea is to shrink their brain by hyperventilating them, because it shuts down the blood circulation of the brain. But if they’re dying of a lack of oxygen to the brain, [that’s] not what you want to do …
I had mentioned [using carbonated beverages during ischemic stroke] in a nutrition class. I had said soda water, meaning carbonated water, but the next week, one of the students said that she had interpreted it as baking soda in water.
Basically, it’s the same idea, but she said she gave a spoonful of baking soda to her mother who had been half-paralyzed for six months, and 15 minutes after drinking just a glass of baking soda water the paralysis lifted and stayed away.”
The reason baking soda worked in this case is probably because CO2 is carried through your bloodstream by sodium bicarbonate (baking soda).14 Peat goes on to discuss how, in the past, firemen used to carry CO2 for the treatment of shock and respiratory arrest.
In the 1920s, Yandell Henderson, director of the Yale Laboratory of Applied Physiology, devised a system using oxygen with 5%, 7% or 10% CO2 added in. Fire departments all over the United States, and many hospitals, were using 5% CO2 to resuscitate babies that had stopped breathing and treat shock cases. It was also used post-operatively to aid in the recovery process.
The Green Agenda’s Flawed View of CO2
In closing, Peat also overturned key arguments of the green agenda by pointing out that during the Carboniferous period of Earth’s history, when plant and animal life was extraordinarily abundant, carbon dioxide levels were some 20 times higher than they are now, and temperatures were relatively stable.
“The expansion of vegetation will reflect infrared rays back into space,” he said, “so it’s sort of like the Earth has a thermostat that will regulate for huge changes in in CO2,” he said.
Even more importantly, nothing thrives in low CO2 environments — not plants, not animals or insects and, as evidenced by everything discussed above, not humans. If anything, the world may actually need a bit more CO2, seeing how CO2-deficiency states are rampant, forests are dying and plants aren’t growing very well. As noted by Peat:
“All animals and even plants suffer from a lack of carbon dioxide. If you lower it, even plants won’t do well … In the 1940s, people experimented with poisoning to death rats or mice with 50% carbon dioxide, keeping them dead for an hour and then reviving them, and they had no brain damage. If they gave them extra CO2, they weren’t damaged by the absence of oxygen. So, for primitive organisms, it’s more essential than oxygen.”
The increasingly erratic weather systems we’re now experiencing likely have little to do with the CO2 content of our atmosphere, and far more to do with a combination of decades-long weather manipulation15 and natural solar cycles.16,17
- 1 Umzu. Who Is Ray Peat?
- 2 Conscious Breathing Carbon Dioxide, Physiology
- 3, 8 Ray Peat, Mitochondria and Mortality
- 4 Skool.com Ray Peat Simplified
- 5 Functional Performance Systems CO2 v. Lactic Acid
- 6 Ray Peat, Protective CO2 and Aging
- 7 StatPearls Biochemistry, Electron Transport Chain
- 9 Ray Peat Forum May 29, 2017
- 10, 12 Toxicological Research March 2011; 27(1): 1-6
- 11 Science Direct Lipid Peroxide
- 13 Stroke October 1, 1999; 30: 2033-2037
- 14 Conscious Breathing Carbon Dioxide
- 15 Geoengineering Watch
- 16 Patreon Adapt2030
- 17 YouTube Adapt2030
Quick Technique Lowers Blood Pressure in Minutes
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/07/03/inspiratory-muscle-strength-training.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked July 03, 2023
STORY AT-A-GLANCE
- Inspiratory muscle strength training can lower blood pressure, improve cardiovascular health and boost cognitive and physical performance in middle-aged adults who do not get the recommended amount of aerobic exercise
- Inspiratory muscle strength training (IMST) involves inhaling through a hand-held device that restricts air flow. By making you work harder to breathe in, you strengthen the muscles used for inhalation
- Most people breathe incorrectly and the ramifications for your health can be significant. One of the most common errors is over breathing, which depletes your carbon dioxide (CO2) reserves, thus lowering tissue oxygenation and causing airway and blood vessel constriction
- Mouth breathing has been linked to an increased risk of snoring, sleep apnea, asthma, abnormal facial development in children, poor oral hygiene, crooked teeth, poor posture, poor sports performance and attention-deficit hyperactivity disorder
- Another near-universal breathing abnormality is breathing vertically rather than horizontally. Correct breathing will cause your midsection to widen while not raising your shoulders or puffing out the upper part of your chest. This is the horizontal breath
Editor’s Note: This article is a reprint. It was originally published April 25, 2019.
The way you breathe has a significant impact on your health, and various breathing exercises have been shown to improve your health and well-being in a number of ways.
Researchers have found inspiratory muscle strength training — a technique that strengthens your respiratory musculature — can improve cardiovascular health, as well as cognitive and physical performance.
Inspiratory muscle strength training (IMST) involves inhaling through a hand-held device that restricts air flow. By making you work harder to breathe in, you strengthen the muscles used for inhalation. The inspiratory muscle trainer device was originally developed for people with respiratory conditions, and to help wean patients off mechanical ventilation.
As you might expect, your breathing muscles, including your diaphragm, will lose strength and atrophy from lack of use, just as other muscles in your body, and research1 shows that strengthening the breathing muscles improves weaning outcome in patients that have become too weak to breathe on their own after being on a ventilator.
How Inspiratory Muscle Strength Training Benefits Your Health
In the featured study, the preliminary results of which were presented at the annual Experimental Biology conference2 in Orlando, Florida, the researchers investigated how IMST might affect vascular, cognitive and physical health in middle-aged adults.
A previous study3 had shown patients with obstructive sleep apnea who used the device to perform 30 inhalations per day for six weeks lowered their systolic blood pressure by an average of 12 millimeters of mercury (mm/Hg).
As reported by Medical News Today,4 “Exercising for the same amount of time usually only lowers blood pressure by half that amount, and the benefits seem to exceed those normally achieved with hypertension medication.”
Intrigued by these findings, the researchers, led by Daniel Craighead, postdoctoral researcher at the University of Colorado Boulder’s Integrative Physiology of Aging Laboratory, decided to investigate whether IMST might be useful for middle-aged adults who resist exercise.5,6,7
Indeed, those who used IMST not only lowered their blood pressure and improved their vascular health, they also improved their exercise tolerance, assessed through treadmill tests, and cognitive performance, assessed through cognitive tests. Craighead commented on the results:8,9
“IMST is something you can do quickly in your home or office, without having to change your clothes, and so far it looks like it is very beneficial to lower blood pressure and possibly boost cognitive and physical performance.
High blood pressure is a major risk factor for cardiovascular disease, which is the number one cause of death in America. Having another option in the toolbox to help prevent it would be a real victory …
I think IMST has slowly evolved from something used only by a very sick population to being something that people can adopt as a part of their everyday lifestyle. Maybe they won’t do 30 minutes of aerobic exercise, but perhaps they’ll do five minutes of this and get some benefits.”
Over Breathing — One of the Most Common Breathing Errors
When it comes to breathing, most people actually do it incorrectly, and the ramifications for your health can be significant. One of the most common errors is over breathing. By breathing more than necessary, you deplete your carbon dioxide (CO2) reserves. While it’s important to remove CO2 from your body, you need a balance of oxygen and CO2 for optimal function.
CO2 is not just a waste product but has actual biological roles, one of which is assisting in oxygen utilization. When your CO2 level is too low, changes in your blood pH impair your hemoglobin’s ability to release oxygen to your cells. This is known as the Bohr effect.10,11
CO2 also helps relax the smooth muscles surrounding your blood vessels and airways, which is why over breathing results in both airway and blood vessel constriction. You can test this by taking five or six big breaths in and out of your mouth.
Most people will begin to experience some light-headedness or dizziness. While you might reason that taking bigger breaths through your mouth allows you to take more oxygen into your body, which should make you feel better, the opposite actually happens.
This is because you’re expelling too much CO2 from your lungs, which causes your blood vessels to constrict — hence the light-headedness. The reality is that the heavier you breathe, the less oxygen is delivered throughout your body due to lack of CO2.

Download this Article Before it Disappears
How Over Breathing Affects Your Health
Typical characteristics of over breathing include mouth breathing, upper chest breathing, sighing, noticeable breathing during rest and taking large breaths before talking. Normal breathing volume is between 4 and 7 liters of air per minute, which translates into 12 to 14 breaths per minute. Breathing more than this is often an indication of poor health.
For example, clinical trials12 involving asthmatics show they breathe between 10 to 15 liters of air per minute and people with chronic heart disease tend to breathe between 15 to 18 liters of air per minute. Mouth breathing in particular is also associated with a number of health problems, including:
| Dehydration |
| Snoring13 |
| Sleep apnea14,15,16,17 |
| Asthma18 — In one study,19 young asthma patients had virtually no exercise-induced asthma after exercising while breathing through their noses. However, they did experience moderate bronchial constriction after exercising while mouth breathing. Research shows mouth breathing may increase asthma morbidity by increasing sensitization to inhaled allergens20 |
| Abnormal facial development21 — Children who breathe through their mouths tend to develop longer faces with altered jaw structures22,23,24,25,26,27 |
| Poor oral hygiene — Loss of moisture dries out your saliva and contributes to poor oral hygiene; dehydration causes your airways to constrict and makes nose breathing even more difficult, creating a vicious cycle |
| Reduced oxygen delivery to your heart, brain and other tissues due to constricted arterial blood flow28 |
| Crooked teeth29 |
| Poor posture30 |
| Poor sports performance31 — This occurs primarily as a side effect of postural changes associated with mouth breathing that decrease muscle strength and inhibits chest expansion.32 Breathing through your nose also boosts air resistance by approximately 50% compared to breathing through your mouth.
As a result, you end up increasing your oxygen intake by 10% to 20% when nose breathing.33 The deeper and more rapid your breath (which is a hallmark of hyperventilation and mouth breathing), the more constricted your blood vessels will be and the less oxygen will be delivered to your tissues,34 and this lack of oxygen will also hamper sports performance |
| Attention-deficit hyperactivity disorder35 |
How to Breathe Properly
To minimize the problems associated with mouth breathing and over breathing, you need to breathe more lightly and through your nose. Ideally, your breath should be so light as to barely move the hairs inside your nose.
Breathing through your nose slows your breathing and makes it more regular, thereby improving oxygenation. Nasal breathing also activates your parasympathetic nervous system, which has a calming and blood pressure lowering effect.36,37
The following steps will help your breath become lighter. While you may feel a slight air shortage at first, this should be tolerable for most people. If it becomes uncomfortable, take a 15-second break and then continue.
- Place one hand on your upper chest and the other on your belly; feel your belly move slightly in and out with each breath, while your chest remains unmoving.
- Close your mouth and breathe in and out through your nose. Focus your attention on the cold air coming into your nose and the slightly warmer air leaving it on the out breath.
- Slowly decrease the volume of each breath, to the point it feels like you’re almost not breathing at all. The crucial thing here is to develop a slight air hunger. This simply means there’s a slight accumulation of carbon dioxide in your blood, which signals your brain to breathe.
After three or four minutes of air hunger, you’ll start experiencing the beneficial effects of CO2 accumulation, such as an increase in body temperature, a sign of improved blood circulation, and an increase in saliva, which is a sign of parasympathetic nervous system activation, which is important for stress reduction.
While mouth breathing tends to lead to over breathing, failure to exhale fully may also be part of the problem that’s causing you to over breathe. Oftentimes, it’s a combination of sucking in excessive air and exhaling incompletely. You’re your exhalation is incomplete, you end up with excess residual air in your lungs, and it is this that makes you feel short of breath.
The answer for this is not to breathe more but to breathe out more fully. You can train yourself to exhale more fully by making sure your exhale is slightly longer than your inhale, and by engaging your diaphragm to really squeeze the air out as you allow your midsection to collapse inward. The vertical breathing exercise below will also help strengthen your diaphragm, which will allow you to exhale more fully.
Vertical Breathing — Another Common Breathing Mistake
Another near-universal breathing abnormality is breathing vertically rather than horizontally. This is something clinical psychologist Belisa Vranich points out in her book “Breathe,” which details her breathing program.
Vertical breathing makes you feel a bit taller on the in-breath, as it raises your chest and shoulders. The problem is that this kind of breathing actually triggers your sympathetic nervous system. In other words, it triggers your stress response, which is the complete opposite of what you want.
Correct breathing will cause your midsection to widen while not raising your shoulders or puffing out the upper part of your chest. This is the horizontal breath. At first, you may find it difficult to take a proper breath, as your midsection and diaphragm may be tight. To relearn proper horizontal breathing, Vranich suggests the following exercise. In time, this exercise will teach your body to use the diaphragm to breathe.
- Begin by relaxing and unbracing your midsection.
- Take a deep breath in and actually feel the middle of your body get wider. Let your belly go.
- On the exhale, roll backward, tipping your hips underneath you while pressing your fingers gently into your belly, giving it a little squeeze.
As mentioned earlier, feeling short of breath is often caused by insufficient exhalation. Engaging your diaphragm and intercostals — the muscles that run between your ribs, allowing your chest wall to move — will allow you to take more complete in and out breaths.
The Link Between Athletic Endurance and CO2 Tolerance
While breathing through your mouth may be particularly tempting during physical exertion, try to avoid this tendency as it will actually diminish your fitness and endurance. Ideally, you would exercise only to the extent that you can continue breathing through your nose the vast majority of the time.
If you feel the need to open your mouth, then slow down and recover. This helps your body to gradually develop a tolerance for increased CO2. Dr. Konstantin Pavlovich Buteyko38 — the Russian physician after whom the Buteyko Breathing Method is named — discovered that the level of CO2 in your lungs correlates to your ability to hold your breath after normal exhalation.
This breath-holding capacity is known as your control pause or CP number. To identify your CP, which will give you an estimate of your CO2 tolerance, perform the following self-test.
1. Sit straight without crossing your legs and breathe comfortably and steadily.
2. Take a small, silent breath in and out through your nose. After exhaling, pinch your nose to keep air from entering.
3. Start your stopwatch and hold your breath until you feel the first definite desire to breathe.
4. When you feel the first urge to breathe, resume breathing and note the time. This is your CP. The urge to breathe may come in the form of involuntary movements of your breathing muscles, or your tummy may jerk or your throat may contract.
Your inhalation should be calm and controlled, through your nose. If you feel like you must take a big breath, then you held your breath too long.
The following criteria are used to evaluate your CP result:
• CP 40 to 60 seconds — Indicates a normal, healthy breathing pattern and excellent physical endurance.
• CP 20 to 40 seconds — Indicates mild breathing impairment, moderate tolerance to physical exercise and potential for health problems in the future (most folks fall into this category).
To increase your CP from 20 to 40, physical exercise is necessary. You might begin by simply walking with one nostril occluded. As your CP increases, begin incorporating jogging, cycling, swimming, weightlifting or anything else to build up an air shortage.
• CP 10 to 20 seconds — Indicates significant breathing impairment and poor tolerance to physical exercise; nasal breath training and lifestyle modifications are recommended. If your CP is less than 20 seconds, never have your mouth open during exercise, as your breathing is too unstable. This is particularly important if you have asthma.
• CP under 10 seconds — Serious breathing impairment, very poor exercise tolerance and chronic health problems.
Short CP times correlate with low tolerance to CO2 and chronically depleted CO2 levels. As a result, the shorter your CP, the more easily you’ll get breathless. The good news is that you will feel better and improve your exercise endurance with each five-second increase in your CP.
How to Increase Your CP and Boost Exercise Endurance
The following breath hold exercise will help increase your CP over time. While this exercise is perfectly safe for most, if you have any cardiac problems, high blood pressure, are pregnant, have Type 1 diabetes, panic attacks or any serious health concern, then do not hold your breath beyond the first urges to breathe.
Repeat this exercise several times in succession, waiting 30 to 60 seconds between rounds. Also, be sure to do it on a regular basis, ideally daily.
- Sitting up straight, take a small breath in through your nose and a small breath out. If your nose is quite blocked, take a tiny breath in through the corner of your mouth.
- Pinch your nose with your fingers and hold your breath. Keep your mouth closed.
- Gently nod your head or sway your body until you feel that you cannot hold your breath any longer.
- When you need to breathe in, let go of your nose and breathe gently through it, in and out, with your mouth closed. Calm your breathing as soon as possible.
For Optimal Health, Learn to Breathe Properly
As mentioned, a normal breathing volume is around 12 to 14 breaths per minute, but research39 published in the medical journal Breathe suggests an optimal respiration rate is in the range of just six to 10 breaths per minute, and done in a way that activates your diaphragm.
Slowing your breathing to 10 breaths per minute or less has been shown to beneficially impact your respiratory, cardiovascular, cardiorespiratory and autonomic nervous systems.40 As noted in the Breathe study:41
“Controlled, slow breathing appears to be an effective means of maximizing HRV [heart rate variability] and preserving autonomic function, both of which have been associated with decreased mortality in pathological states and longevity in the general population.”
Aside from the breathing techniques already mentioned, there are many others that can be equally helpful. Following is a short list of a few additional breathing methods you can try, all of which are backed by scientific evidence42 showing their beneficial influence on human health.
| Nadi Shodhana/Nadi Shuddhi (alternate nostril breathing) — With your right thumb, close the right nostril and inhale through your left nostril. Closing the left nostril, exhale through the right, following which, inhalation should be done through the right nostril. Closing the right nostril, breathe out through your left nostril. This is one round. The procedure is repeated for the desired number of rounds. |
| Surya Anuloma Viloma (right uninostril breathing) — Closing the left nostril, both inhalation and exhalation should be done through your right nostril, without altering the normal pace of breathing. |
| Chandra Anuloma Viloma (left uninostril breathing) — Similar to Surya Anuloma Viloma, breathing is done through your left nostril alone, by closing the right nostril. |
| Surya Bhedana (right nostril initiated breathing) — Closing the left nostril, inhalation should be done through your right nostril. At the end of inhalation, close the right nostril and exhale through the left nostril. This is one round. The procedure is repeated for the desired number of rounds. |
| Ujjayi (psychic breath) — Inhalation and exhalation are done through the nose at a normal pace, with partial contraction of the glottis, which produces a light snoring sound. You should be aware of the passage of breath through your throat during the practice. |
| Bhramari (female honeybee humming breath) — After a full inhalation, closing the ears using your index fingers, you should exhale making a soft humming sound similar to that of a honeybee. |
- 1 Critical Care 2011; 15(2): R84
- 2 Experimental Biology Conference Program, April 6-9, 2019
- 3 Sleep 2016 Jun 1;39(6):1179-85
- 4, 8 Medical News Today April 10, 2019
- 5 University of Colorado Boulder February 25, 2019
- 6, 9 Inverse.com April 9, 2019
- 7 Science Daily April 8, 2019
- 10 Buteyko.com FAQ
- 11 The Influence of the Carbon Dioxide Content of Blood on its Oxygen Binding
- 12 J Appl Physiol. 1995 Sep; 79(3): 892-901
- 13, 17 Ann Allergy Asthma Immunol. 1998 Oct;81(4):279-87; quiz 287-90
- 14 Eur Arch Otorhinolaryngol. 2011 Apr;268(4):533-9
- 15 Respiration. 2010;80(6):488-94
- 16 Acta Otolaryngol Suppl. 1996;523:228-30
- 18 MedicalNewsToday. What’s Wrong With Breathing Through the Mouth? September 22, 2017
- 19 American Review of Respiratory Disease July 1, 1978; 118(1):65-7
- 20 Allergy 2016 Jul;71(7):1031-6
- 21 Laryngoscope. 2007 Jun;117(6):1102-6
- 22 American Journal of Orthodontics April 1983; 83(4): 334-340
- 23 Angle Orthod 1990 Fall; 60(3): 167- 76
- 24 Laryngoscope 2010 Oct; 120(10): 2089-93
- 25, 32 Braz J Otorhinolaryngol. 2011 Sep-Oct; 77(5):656-62
- 26, 31 Bras Pneumol. 2011 Jul-Aug; 37(4)):471-9
- 27 Journal Pediatrics (Rio J) 2011 Jul-Aug; 87(4)):471-9
- 28 Western Journal of Medicine 1983 May; 138(5): 733–736
- 29 Saacks Orthodontics How Mouth Breathing Causes Crooked Teeth
- 30 Int J Orofacial Myology. 2000 Nov;26:13-23
- 33 Breathing and Sleep Center. The Benefits of Breathing Through Your Nose
- 34 American Journal of Psychiatry 1992 Nov;149(11):1589-91
- 35 Neuroreport 2013 Dec 4; 24(17): 935–940
- 36 Conf Proc IEEE Eng Med Biol Soc. 2007: 5323-5325
- 37 Indian J Med Research 2004 Aug;120(2):115-2
- 38 Buteyko.com
- 39, 40, 41 Breathe (Sheff). 2017 Dec; 13(4): 298–309
- 42 J Ayurveda Integr Med. 2018 Jan 30. pii: S0975-9476(17)30322-4
Daily Breathing Exercises Could Reduce Heart Attack Risk
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/06/22/daily-breathing-exercises-heart-attack-risk.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked June 22, 2023

STORY AT-A-GLANCE
- Using slow breathing methods to help you relax can lower your blood pressure, thereby reducing your risk of related heart attack, stroke and heart disease
- Engaging in slow, deep breathing for just two minutes lowers systolic blood pressure by 8.6 mmHg and diastolic blood pressure by 4.9 mmHg among people with high blood pressure
- Slow breathing refers to 10 breaths per minute or less “with prolonged, rhythmic, slow and deep expiratory periods”
- Spending just five minutes on focused breath training can also help lower blood pressure
- Slow breathing causes biochemical changes that induce relaxation, including increasing endorphins and lowering adrenaline and blood acidity, while deepening the volume of inspiration and expiration, maximizing the amount of oxygen entering the bloodstream
Using slow breathing methods to help you relax can lower your blood pressure, thereby reducing your risk of related heart attack, stroke and heart disease. Breathing exercises offer a non-pharmacological method for reducing high blood pressure,1 making them useful for the 1.28 billion people affected by this condition worldwide.2
Among them, about half are unaware that their blood pressure is high. This is why high blood pressure is often referred to as the “silent killer.” Often, people don’t know their blood pressure is in an unhealthy range until complications occur. Fortunately, breathing exercises can be practiced by anyone, any time, providing a simple way to help manage the condition.
Further, there’s no downside to trying them, so there’s good reason to give breathing exercises a chance, even if you haven’t been diagnosed with high blood pressure.
Reduce Blood Pressure With Slow Breathing
Engaging in slow, deep breathing for just two minutes lowers systolic blood pressure (SBP) by 8.6 mmHg and diastolic blood pressure (DBP) by 4.9 mmHg among people with high blood pressure, according to a 2005 study.3 Slow breathing refers to 10 breaths per minute or less “with prolonged, rhythmic, slow and deep expiratory periods.”
This causes biochemical changes that induce relaxation, including increasing endorphins and lowering adrenaline and blood acidity. Slow breathing “increases the length of the diaphragm contraction, minimizes the respiratory rate, and deepens the volume of inspiration and expiration, thus maximizing the amount of oxygen entering the bloodstream,” researchers wrote in Frontiers in Physiology, and this is only the beginning.4
The team conducted a scoping review of 20 studies, which also revealed slow breathing’s blood pressure benefits. They found systolic blood pressure declined by 4 to 54.22 mmHg, while diastolic blood pressure decreased by 3 to 17 mmHg among study participants aged from 18 to 75.5
One way slow breathing works is via its effect on the autonomic nervous system (ANS). Your ANS controls both your body’s sympathetic nervous system (SNS) — the part that triggers your “fight-or-flight” response — as well as its parasympathetic nervous system (PNS), which triggers the relaxation response.
Any type of external stressor — everything from an argument with a loved one to a night of lost sleep — will prompt a reaction from the ANS, which signals to your brain’s hypothalamus to either ramp up into overdrive or calm down.6
An imbalanced ANS — specifically increased SNS activity and decreased PNS activity, plays a role in the development of high blood pressure,7 but slow breathing helps remedy this. The Frontiers in Physiology team explained:8
“According to research, slow breathing lowers sympathetic tone and raises parasympathetic tone. This could be partially mediated by alterations in intrathoracic pressure, stimulation of arterial and cardiopulmonary baroreceptors and pulmonary afferent stretch receptors or by central interactions between respiratory and cardiovascular centers in brainstem modulation of vagal activity during breathing.”
Five-Minute Breathing ‘Workout’ for Blood Pressure Health
Spending just five minutes on focused breath training can also help lower blood pressure, according to a separate study by researchers from the University of Colorado Boulder and the University of Arizona.
The team split 128 adults aged 18 to 82 years into two groups. One group did high-resistance inspiratory muscle strength training (IMST) training consisting of 30 breaths a day for six weeks. The other group did a low-resistance sham breathing exercise for the same period.9
IMST is used for recovery in people who have been on a ventilator, as well as to support breathing in those with asthma, chronic obstructive pulmonary disease and other breathing disorders.10 While no changes in SBP or DBP occurred in the placebo group, those doing the high-resistance breathing exercise had an average reduction of 9 mmHg in systolic blood pressure.11
According to study author Daniel Craighead, the reduction is similar to what may be achieved with medication and potentially more effective than weight loss or reducing sodium in your diet. He told Insider, “People can expect fairly rapid results. We would expect that if you went longer, blood pressure would go down even more.” He recommended the technique for those with high blood pressure and those hoping to prevent it:12
“What’s really exciting about this is that it’s helpful for a wide range of adults. People with blood pressure at an unhealthy level could stand to benefit from adding this to their routine now. But someone could start in their thirties and stick to it for years to help delay or prevent hypertension.”
The breathing exercise takes just five to 10 minutes a day, with benefits noticeable within two weeks. It involves the use of an inhaler-like device, which provides resistance as you take a breath, causing your respiratory muscles to get a workout. While the trial used a $500 device, less expensive models are commercially available.13
According to the study, “These compiled findings from multiple independent trials provide the strongest evidence to date that high-resistance IMST evokes clinically significant reductions in SBP and DBP.”14
Also noteworthy, the participants did the breathing exercises for six weeks, then took a six-week break. When their blood pressure was tested after the break, it was nearly as low as it was immediately after the exercise session ended. The researchers are also looking into whether a “maintenance dose” of the breathing exercise could help extend the blood pressure reductions even longer.15

Download this Article Before it Disappears
Stress Raises Blood Sugar Levels — Can Breathing Help?
Stress and anxiety activate the SNS response that plays a role in high blood pressure as well as blood sugar levels. When you’re stressed, it causes the SNS to release hormones such as norepinephrine and epinephrine, which stimulate glucose produce and reduce insulin, affecting your blood sugar levels.16
Stress is another factor in high blood pressure and relieving it may offer some relief. This is another mechanism by which controlled breathing may help blood pressure. The way you breathe — whether fast or slow, shallow or deep — is intricately tied to your body as a whole, sending messages that affect your mood, your stress levels and even your immune system.
In early 2017, researchers discovered breathing may directly affect your brain activity, including your state of arousal and higher-order brain function.17 As such, controlled breathing exercises may modify stress coping behaviors and initiate appropriate balance in cardiac autonomic tone, which is a term that describes your heart’s ability to respond to and recover from stressors.18
By lowering stress levels, breathing exercises could therefore help not only your blood pressure but also potentially your blood sugar levels.
Breathing Exercises Lower Oxidative Stress
Excessive oxidative stress (OS) leads to an accumulation of free radicals and inflammation linked to aging and disease. But breathing exercises are known to improve oxidative stress in healthy young adults as well as those with diabetes, high blood pressure and chronic obstructive pulmonary disease.19
Further, in a systematic review and meta-analysis, breathing exercises increased protective superoxide dismutase (SOD) and glutathione (GSH) activities and decreased malondialdehyde, an oxidation product. The researchers, from Weifang Medical University in China, explained:20
“SOD is converted into hydrogen peroxide by catalyzing oxygen reduction, which is then converted to water by GSH. It can effectively remove oxygen free radicals, protect endothelial cells from damage, relax vascular smooth muscle by increasing NO [nitric oxide] release, thus achieving the purpose of lowering OS.”
Different Types of Breathing Exercises
There are many different types of breathing techniques available. Some, like IMST, involve using a device to assist you in slowing down your breathing. RESPeRATE is another form of device-guided slow breathing found to “significantly lower BP.” According to a scientific statement from the American Heart Association:21
“One device has received US Food and Drug Administration approval for over-the-counter distribution “for use in stress reduction and adjunctive treatment to reduce blood pressure.” This interactive system uses a belt around the thorax to monitor breathing rate, which feeds real-time data into a small battery-operated controller box, which in turn generates musical tones into headphones, corresponding to inspiration and expiration.
Studies support that most people find it easy to use the device and experience a prompt and effortless reduction in respiratory rate as they match their breathing pattern to the musical notes.”
The downside of such devices is they cost hundreds of dollars. But there are other options available that don’t cost anything. At the most basic level, you can start by breathing only through your nose.
This helps you avoid mouth breathing, which tends to promote hyperventilation, decreasing tissue oxygenation. Mouth breathing can also elevate your heart rate and blood pressure, sometimes resulting in fatigue and dizziness.22 The Buteyko Breathing Method is one way to reverse health problems associated with improper breathing, the most common of which include over-breathing and mouth breathing.
When you stop mouth breathing and learn to bring your breathing volume toward normal, you have better oxygenation of your tissues and organs. The Buteyko Breathing Method allows you to retain and gently accumulate CO2, which calms breathing and reduces anxiety:
- Take a small breath into your nose, followed by a small breath out
- Hold your nose for five seconds in order to hold your breath, and then release your nose to resume breathing
- Breathe normally for 10 seconds
- Repeat the sequence
More Simple Breathing Techniques
There are other options you can try as well. Box breathing is one such technique that triggers the parasympathetic nervous system to help manage stress. This technique, also called square breathing or four-square breathing, is used by Navy SEALS to help reduce stress in high-pressure situations.
It involves nose breathing to slow over-breathing and raise CO2 levels to balance oxygenation. To begin practicing box breathing, get in a quiet place where you can concentrate and maintain good posture. Work up to using the technique for five-minute increments:23
- Step 1 — Begin by exhaling the air out of your lungs to a slow count of four. Some recommend exhaling through your mouth, others through your nose.
- Step 2 — Hold your breath for a slow count of four.
- Step 3 — Inhale slowly to a slow count of four through your nose, keeping your back straight and breathing through your abdomen so your shoulders do not rise.
- Step 4 — Hold your breath for a slow count of four and return to step 1.
You can also try the 4-7-8 method, known for relaxation and promoting restful sleep.24 First, exhale all your breath. Then inhale through your nose to a count of four. Hold your breath for seven seconds, then exhale, making a whoosh sound, for a count of eight. Repeat the process three times.
There are also specialized forms of yogic breathing, such as nadi shodhana, or alternate nostril breathing.25 To try it, use your right thumb to close the right nostril, then inhale through your left nostril. Next, close the left nostril and exhale through the right. The next inhalation should be done through right nostril. Then, close the right nostril and breath out through your left nostril. This is one round. You can repeat the procedure for the desired number of rounds.
As noted by the Frontiers in Physiology team, “Slow deep breathing is easy for people of all ages and does not have to be expensive.”26 This is what makes it such a useful tool to embrace, not only for lowering blood pressure and related heart attack risk but also for general relaxation, stress relief and well-being.
- 1 Front Physiol. 2023; 14: 1048338
- 2 Front Physiol. 2023; 14: 1048338., Intro
- 3, 4, 7, 8 Front Physiol. 2023; 14: 1048338., Discussion
- 5 Front Physiol. 2023; 14: 1048338., Results
- 6 Harvard Health Blog December 1, 2021
- 9, 14 Journal of Applied Physiology September 15, 2022
- 10 UCLA Health January 28, 2022
- 11, 12, 13, 15 Insider September 24, 2022
- 16 Cureus. 2019 Aug; 11(8): e5474
- 17 Science March 31, 2017
- 18 Indian J Physiol Pharmacol. 2014 Jul-Sep;58(3):211-21
- 19 Front Med (Lausanne). 2023; 10: 1121036., Intro
- 20 Front Med (Lausanne). 2023; 10: 1121036., Discussion
- 21 Hypertension June 2013, Vol 61, Issue 6
- 22 Biol Psychol. 1998 Sep;49(1-2):83-94
- 23 Time Magazine, May 4, 2016
- 24 CNN September 16, 2022
- 25 J Ayurveda Integr Med. 2018 Jan 30., Table 1
- 26 Front Physiol. 2023; 14: 1048338., Conclusions
What Does the ‘Best Evidence’ Say About Antidepressants?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2022/07/28/antidepressants-health-risks.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate, and will not be bullied into removing it.
Analysis by Dr. Joseph Mercola Fact Checked July 28, 2022

STORY AT-A-GLANCE
- In June 2022, 22.4% of American adults reported symptoms of depression, compared to 7.1% in 2017. When the numbers were broken down in April 2022, half of young adults ages 18 to 24 reported feeling depressed; 22% ages 45 to 64 had depression symptoms; 9% of people age 65 or over reported feeling depressed
- Antidepressant drugs — the most widely used therapy for depression — are also among the least effective, and often make the situation worse, especially in the long term
- Studies have repeatedly shown antidepressants work no better than placebo for mild to moderate depression
- A 2017 systematic review of 131 placebo-controlled studies found that “all trials were at high risk of bias” and that clinical significance was questionable
- Antidepressants are neurotoxic and possible side effects include worsening depression, self-harm, violence and suicide, increased risk for diabetes, heart disease, heart attack, stroke and dementia, and depletion of various nutrients (depending on the type of drug you take)
This article was previously published April 4, 2019, and has been updated with new information.
In June 2022, 22.4% of American adults reported symptoms of depression, compared to 7.1% in 2017.1 When the numbers were broken down in April 2022, half of young adults ages 18 to 24 reported feeling depressed; 22% ages 45 to 64 had depression symptoms; 9% of people age 65 or over reported feeling depressed.2 While the rapid rise in depression has been attributed to the COVID-19 pandemic, the symptoms of depression have not changed.
Depression can interfere with personal and work relationships, reduce work or academic performance and affect physical health by impairing your ability to properly care for yourself and make good health decisions, including decisions about nutrition and sleep. Imbalances in nutrition, weight fluctuations and poor sleep habits may in turn compromise your immune function.3
The condition can also be lethal, as depression is a contributing factor in up to 70% of all suicides.4 In 2016, 44,965 Americans committed suicide.5 In 2020, 45,959 Americans died by suicide.6 Depression can also lead to self-harming behaviors such as drug or alcohol abuse,7 and 90% of people who struggle with suicidal thoughts experience a combination of depression and substance abuse.8
Unfortunately, antidepressant drugs — the most widely used therapy for depression — are also among the least effective. In fact, statistics suggest that far from being helpful, psychiatric drugs are making the situation worse.
According to research9,10 published in February 2017, 16.7% of the 242 million U.S. adults (aged 18 to 85) included in the survey reported filling at least one prescription for a psychiatric drug in 2013.
Twelve percent reported using an antidepressant; 8.3% used anxiolytics, sedatives and hypnotics; and 1.6% used antipsychotics. With nearly 17% of the adult population in the U.S. taking psychiatric drugs, it would be prudent to evaluate the larger ramifications of these types of medications.
In 2022, more than 24% of Americans (about 50 million) are taking a prescription mental health drug.11 And, while prescription rates for antidepressants and anxiolytics increased early during pandemic in 2020, they decreased near the end of that year, with researchers speculating that the decrease may have been due to fewer in-person doctor visits.12
Sadly, no matter what the prescription numbers are, statistics overwhelmingly fail to support the use of these drugs, yet they continue to be the leading form of treatment.
Medication Madness — A Psychiatrist Speaks Out
In a segment of Full Measure (above), award-winning investigative journalist Sharyl Attkisson interviewed psychiatrist and director of the International Center for Patient-Oriented Psychiatry, Dr. Peter Breggin. He is known to many as “the conscience of psychiatry,” as he was instrumental in preventing the return of lobotomy as a psychiatric treatment in the early 1970s.
Breggin is also the author of “Medication Madness,” in which he details the many hazards of psychiatric drugs. In his 50 years of practice, he has never placed a patient on drugs. In fact, he specializes in getting people off them, and wrote a book on psychiatric drug withdrawal, “Psychiatric Drug Withdrawal: A Guide for Prescribers, Therapists, Patients and Their Families.”13
When asked what he thinks people don’t know about psychiatric treatment, and ought to, Breggin responds, “They don’t know that all psychiatric drugs are neurotoxins. They don’t know that they aren’t correcting biochemical imbalances, they are causing biochemical imbalances.”
Prozac was the first selective serotonin reuptake inhibitor (SSRI), approved by the U.S. Food and Drug Administration (FDA) in 1987.14 Over the years, Prozac became the target of a number of lawsuits, as patients suffered all sorts of ill effects, from birth defects to suicide and serotonin syndrome, a condition caused by excess serotonin in the brain, leading to agitation, confusion, high blood pressure and more.15
Already by 1996, 35,000 complaints about the drug had been lodged with the FDA.16 In the early 1990s, Breggin was appointed by a federal court as the medical and scientific expert for the plaintiffs in all combined lawsuits facing Eli Lilly with regard to Prozac, a role that gave him access to corporate records.17 Breggin tells Attkisson:18
“Prozac … had amphetamine affects. The chief investigators said and wrote, ‘this drug has amphetamine like effects. We need to put this into the label. It can make depression worse, can make people agitated, make them angry, might increase the suicide rate,’ but the FDA wouldn’t allow onto the label what it’s chief investigator into adverse effects was telling them.
So, from the beginning, it was all a house of cards. And, as for it’s being useful, I looked it over, carefully analyzed the statistics and said the drug actually doesn’t work. It’s about as good as placebo.
Now, placebo will help anywhere between 40% and 80% of people, so it’s a huge effect and that especially with depression, because depression is not about a biochemical imbalance. It’s about hopelessness. Depression is part of the human experience.”
In Breggin’s view, “There is no promising medical treatment and probably there never can be,” for the simple reason that depression is primarily rooted in the complexity of human emotions and experiences. He believes one needs to avoid numbing and escapist behaviors such as drug and alcohol use, and implement strategies to support healthy brain function instead, in order to “be able to deal with your issues.”
Contrary to Popular Opinion, Antidepressants Don’t Work
In 2010, I interviewed medical journalist and Pulitzer Prize nominee Robert Whitaker about the use of psychiatric drugs, as he has written two books on this topic. I’ve included that interview here for your convenience. In it, Whitaker details the science showing antidepressants don’t work — and what actually does.
The available science has also brought Jacob Stegenga, a philosophy of science lecturer at the University of Cambridge and author of “Medical Nihilism,” to the same conclusion. In a recent essay, he notes:19
“Diving into the details of how antidepressant data are generated, analyzed and reported tells us that these drugs are barely effective, if at all … The best evidence about the effectiveness of antidepressants comes from randomized trials and meta-analyses of these trials.
The vast majority of these studies are funded and controlled by the manufacturers of antidepressants, which is an obvious conflict of interest. These trials often last only weeks — far less than the duration that most people are on antidepressants.
The subjects in these trials are selected carefully, typically excluding patients who are elderly, who have other diseases, or who are on several other drugs — in other words, the very kinds of people who are often prescribed antidepressants — which means that extrapolating the evidence from these trials to real patients is unreliable.
The trials that generate evidence seeming to support antidepressants get published, while trials that generate evidence suggesting that antidepressants are ineffective often remain unpublished …
To give one prominent example, in 2012 the U.K. pharmaceutical company GlaxoSmithKline pleaded guilty to criminal charges for promoting the use of its antidepressant Paxil in children (there was no evidence that it was effective in children), and for misreporting trial data … When analyzed properly, the best evidence indicates that antidepressants are not clinically beneficial.”
What Does the ‘Best Evidence’ Say About Antidepressants?
While some psychiatric drugs may be helpful for a small minority of people with very severe mental health problems, such as schizophrenia, it’s quite clear that a vast majority of people using these drugs do not suffer from the type of psychiatric illnesses that might warrant their prudent use.
Most are struggling with sadness, grief, anxiety, “the blues” and depression, which are in many ways part of your body’s communication system, revealing nutritional or sunlight deficiencies and/or spiritual disconnect, for example.
The underlying reasons for these kinds of troubles are manifold, but you can be sure that, whatever the cause, an antidepressant will not correct it. In fact, as noted by Breggin, studies20,21,22 have repeatedly shown antidepressants work no better than placebo for mild to moderate depression.
Irving Kirsch, associate director of the Program in Placebo Studies at Harvard Medical School, has conducted several meta-analyses of antidepressants in comparison to placebo, concluding there’s virtually no difference in their effectiveness. According to Kirsch, “The difference is so small, it’s not of any clinical importance.”23 For example:
In a 1998 meta-analysis24 that looked at 19 double-blind studies, Kirsch and colleagues noted that:
|
| Research published in 2008 found major discrepancies between published and unpublished research makes antidepressants appear far more beneficial and effective than the sum total of the research actually reveals them to be. Of 74 FDA-registered studies, 31% were never published.
As noted by the authors, “According to the published literature, it appeared that 94% of the trials conducted were positive. By contrast, the FDA analysis showed that 51% were positive … Selective reporting of clinical trial results may have adverse consequences for researchers, study participants, health care professionals and patients.” |
| A 2010 meta-analysis25 concluded that “The magnitude of benefit of antidepressant medication compared with placebo increases with severity of depression symptoms and may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.” |
| In a 2011 paper,26 Kirsch notes that six-week trials have a higher success rate than eight-week trials — 55 versus 42% — which suggests long-term use of antidepressants is likely ineffective. |
| In a 2014 paper,27 Kirsch notes that “analyses of the published data and the unpublished data that were hidden by drug companies reveals that most (if not all) of the benefits are due to the placebo effect.” In this paper, he notes that two of his earlier meta-analyses28,29 actually revealed that when both published and unpublished trials were included, the placebo response accounted for a whopping 82% of the beneficial response to antidepressants.
A major benefit of evaluating FDA trial data was that all of the trials used the same primary measure of depression, which made the drug-to-placebo effects very easy to identify and compare. The primary measure of depression used in these studies was the Hamilton depression scale, a 17-item scale with a possible score of 0 to 53 points. The higher your score, the more severe your depression. Importantly, the mean difference between antidepressants and placebo was less than 2 points (1.8) on this scale. To illustrate just how insignificant of a difference this is, you can score a 6-point difference simply by changing sleep patterns without any reported change in other depressive symptoms. Simply fidgeting less results in a 4-point decrease in your depression score, so as noted by Stegenga in his essay,30 “a drug that simply made people sleep better and fidget less could lower one’s depression score by 10 points.” What’s more, clinical guidelines in the U.K. require antidepressants to lower depression scores by a mere 3 points,31 and this too reveals why and how the benefits of antidepressants have been overestimated and oversold. |
| Most recently, a 2017 systematic review with meta-analysis and trial sequential analysis of 131 placebo-controlled studies found that “all trials were at high risk of bias and the clinical significance seems questionable. SSRIs significantly increase the risk of both serious and non-serious adverse events. The potential small beneficial effects seem to be outweighed by harmful effects.”
None of the trials, even when reporting a positive result, met the threshold for clinical significance of 3 points on the depression score. |
Long-Term, Antidepressant Users Fare Much Worse
What’s more, research has shown that patients who do not take antidepressants fare better in the long term compared to those taking drugs,32 and research33 comparing exercise and drug treatment for depression suggests those not taking drugs have a lower risk of relapse. This risk is also addressed in Kirsch’s 2014 paper34 on antidepressants and the placebo effect.
“The serotonin theory is as close as any theory in the history of science to having been proved wrong. Instead of curing depression, popular antidepressants may induce a biological vulnerability making people more likely to become depressed in the future,” Kirsch writes.
Known Side Effects of Antidepressants
In addition to not working better than placebo, antidepressants also come with a long list of potential side effects, which include but are not limited to:35,36
| Worsening depression |
| Self-harm, violence and suicide |
| Increased risk of developing Type 2 diabetes,37 even after adjusting for risk factors such as body mass index38 |
| Thickening of the greater carotid intima-media (the lining of the main arteries in your neck that feed blood to your brain),39 which could contribute to the risk of heart disease and stroke. This was true both for SSRIs and antidepressants that affect other brain chemicals |
| An increased risk of heart attack, specifically for users of tricyclic antidepressants, who have a 36% increased risk of heart attack40 |
| An increased risk of dementia; as the dose increases, so does the risk for dementia41 |
| Depletion of various nutrients, including coenzyme Q10 and vitamin B12 — in the case of tricyclic antidepressants — which are needed for proper mitochondrial function. SSRIs have been linked to iodine and folate depletion42 |
Depression Treatments That Actually Work
If you’re at all interested in following science-based recommendations, you’d place antidepressants at the very bottom of your list of treatment candidates. Far more effective treatments for depression include:
| Exercise — A number of studies have shown exercise outperforms drug treatment. Exercise helps create new GABA-producing neurons that help induce a natural state of calm, and boosts serotonin, dopamine and norepinephrine, which helps buffer the effects of stress.
Studies have shown there is a strong correlation between improved mood and aerobic capacity, but even gentle forms of exercise can be effective. Yoga, for example, has received particular attention in a number of studies. One study found 90-minute yoga sessions three times a week reduced symptoms of major depression by at least 50%.43 |
| Nutritional intervention — Keeping inflammation in check is an important part of any effective treatment plan. If you’re gluten sensitive, you will need to remove all gluten from your diet. A food sensitivity test can help ascertain this. Reducing lectins may also be a good idea.
As a general guideline, eating a whole food diet as described in my optimal nutrition plan can go a long way toward lowering your inflammation level. A cornerstone of a healthy diet is limiting sugar of all kinds, ideally to no more than 25 grams a day. In one study,44 men consuming more than 67 grams of sugar per day were 23% more likely to develop anxiety or depression over the course of five years than those whose sugar consumption was less than 40 grams per day. Certain nutritional deficiencies are also notorious contributors to depression, especially:
|
| Vitamin D — Studies have shown vitamin D deficiency can predispose you to depression and that depression can respond favorably to optimizing your vitamin D stores, ideally by getting sensible sun exposure.51,52 In one study,53 people with a vitamin D level below 20 nanograms per milliliter (ng/mL) had an 85% increased risk of depression compared to those with a level greater than 30 ng/mL.
A double-blind randomized trial54 published in 2008 concluded that supplementing with high doses of vitamin D “seems to ameliorate [depression] symptoms indicating a possible causal relationship.” Recent research55 also claims that low vitamin D levels appear to be associated with suicide attempts. For optimal health, make sure your vitamin D level is between 60 and 80 ng/mL year-round. Ideally, get a vitamin D test at least twice a year to monitor your level. |
| Light therapy — Light therapy alone and placebo were both more effective than Prozac for the treatment of moderate to severe depression in an eight-weeklong study.56 Spending time outdoors in broad daylight is the least expensive and likely most effective option. |
| Probiotics — Keeping your gut microbiome healthy also has a significant effect on your moods, emotions and brain. |
| Emotional Freedom Techniques (EFT) — EFT is a form of psychological acupressure that has been shown to be quite effective for depression and anxiety.57,58,59,60 For serious or complex issues, seek out a qualified health care professional who is trained in EFT to guide you through the process.
That said, for most of you with depression symptoms, this is a technique you can learn to do effectively on your own. In the video below, EFT practitioner Julie Schiffman shows you how. |
Other Helpful Treatment Strategies
Here are several additional strategies that can help improve your mental health:
| Minimize electromagnetic field (EMF) exposure — In 2016, Martin Pall, Ph.D., published a review61 in the Journal of Neuroanatomy showing how microwave radiation from cellphones, Wi-Fi routers and computers and tablets not in airplane mode is clearly associated with many neuropsychiatric disorders.
These electromagnetic fields (EMFs) increase intracellular calcium and trigger the production of extremely damaging free radicals by acting on your voltage gated calcium channels (VGCCs), and the tissue with the highest density of VGCCs is your brain. Once these VGCCs are stimulated they also cause the release of neurotransmitters and neuroendocrine hormones, which contribute not only to anxiety and depression but also neurodegenerative diseases like Alzheimer’s. So, if you struggle with anxiety or depression, be sure to limit your exposure to wireless technology. Simple measures include turning your Wi-Fi off at night, not carrying your cellphone on your body unless it’s in airplane mode, and not keeping portable phones, cellphones and other electric devices in your bedroom. |
| Clean up your sleep hygiene — Make sure you’re getting enough high quality sleep, as sleep is essential for optimal mood and mental health. The inability to fall asleep and stay asleep can be due to elevated cortisol levels, so if you have trouble sleeping, you may want to get your saliva cortisol level tested with an Adrenal Stress Index test.
Adaptogens, herbal products that help lower cortisol and adjust your body to stress, can be helpful if your cortisol is running high. There are also other excellent herbs and amino acids that help you to fall asleep and stay asleep. |
| Optimize your gut health — A number of studies have confirmed gastrointestinal inflammation can play a critical role in the development of depression.62 Optimizing your gut microbiome will also help regulate a number of neurotransmitters and mood-related hormones, including GABA and corticosterone, resulting in reduced anxiety and depression-related behavior.63
To nourish your gut microbiome, be sure to eat plenty of fresh vegetables and traditionally fermented foods such as fermented vegetables, lassi, kefir and natto. If you do not eat fermented foods on a regular basis, taking a high-quality probiotic supplement is recommended. Also remember to severely limit sugars and grains, to rebalance your gut flora. |
| Visualization — Visualization and guided imagery have been used for decades by elite athletes before an event, successful business people and cancer patients — all to achieve better results through convincing your mind you have already achieved successful results.64,65 Similar success has been found in people with depression.66 |
| Cognitive behavioral therapy (CBT) — CBT has been used successfully to treat depression.67,68 This therapy assumes mood is related to the pattern of thought. CBT attempts to change mood and reverse depression by directing your thought patterns. |
| Make sure your cholesterol levels aren’t too low for optimal mental health — You may also want to check your cholesterol to make sure it’s not too low. Low cholesterol is linked to dramatically increased rates of suicide, as well as aggression toward others.69
This increased expression of violence toward self and others may be due to the fact that low membrane cholesterol decreases the number of serotonin receptors in the brain, which are approximately 30% cholesterol by weight. Lower serum cholesterol concentrations therefore may contribute to decreasing brain serotonin, which not only contributes to suicidal-associated depression, but prevents the suppression of aggressive behavior and violence toward self and others. |
| Ecotherapy — Studies have confirmed the therapeutic effects of spending time in nature. Ecotherapy has been shown to lower stress, improve mood and significantly reduce symptoms of depression.70 Outdoor activities could be just about anything, from walking a nature trail to gardening, or simply taking your exercise outdoors. |
| Breathing exercises — Breath work such as the Buteyko breathing technique also has enormous psychological benefits and can quickly reduce anxiety by increasing the partial pressure of carbon dioxide in your body. |
Helpful supplements — A number of herbs and supplements can be used in lieu of drugs to reduce symptoms of anxiety and depression. These include:
|
Guidelines for Safe Drug Withdrawal
If you’re currently on an antidepressant and want to get off it, ideally, you’ll want to have the cooperation of your prescribing physician. It would also be wise to do some homework on how to best proceed.
Breggin’s book, “Psychiatric Drug Withdrawal: A Guide for Prescribers, Therapists, Patients and Their Families,”75 and/or “The Antidepressant Solution: A Step-by-Step Guide to Overcoming Antidepressant Withdrawal, Dependence, and Addiction”76 by Dr. Joseph Glenmullen can be helpful.
You can also turn to an organization with a referral list of doctors who practice more biologically or naturally, such as the American College for Advancement in Medicine at www.acam.org. A holistic psychiatrist will have a number of treatment options in their tool box that conventional doctors do not, and will typically be familiar with nutritional supplementation.
Once you have the cooperation of your prescribing physician, start lowering the dosage of the medication you’re taking. There are protocols for gradually reducing the dose that your doctor should be well aware of. At the same time, it may be wise to add in a multivitamin and/or other nutritional supplements or herbs. Again, your best bet would be to work with a holistic psychiatrist who is well-versed in the use of nutritional support.
If you have a friend or family member who struggles with depression, perhaps one of the most helpful things you can do is to help guide them toward healthier eating and lifestyle habits, as making changes can be particularly difficult when you’re feeling blue — or worse, suicidal.
Encourage them to unplug and meet you outside for walks. We should not underestimate the power of human connection, and the power of connection with nature. Both, I believe, are essential for mental health and emotional stability.
If you are feeling desperate or have any thoughts of suicide, please call the National Suicide Prevention Lifeline, a toll-free number: 1-800-273-TALK (8255), or call the new, federal suicide and crisis hotline at 988.77 Or, simply go to your nearest hospital emergency department. You cannot make long-term plans for lifestyle changes when you are in the middle of a crisis.
- 1 Statista. June 2022
- 2 Forbes. 50% of Young Adults Report Symptoms of Depression. April 28, 2022
- 3 Family Health Psychiatric & Counseling Center. The Role of Exercise, Nutrition, and Sleep in the Battle Against Depression
- 4 Mental Health America, Suicide Statistics
- 5 National Center for Health Statistics, Depression
- 6 2020 USA General Statistics. Suicide
- 7 All About Depression, Major Depressive Disorder
- 8 Clinical Neuroscience Research, 2001;1(5):310
- 9 Jama Internal Medicine December 12, 2016
- 10 NBC News December 12, 2016
- 11 QuoteWizard Pandemic Fuels Rise in Mental Health Prescriptions. January 6, 2022
- 12 Front. Pharmacol., 27 April 2022
- 13, 75 Psychiatric Drug Withdrawal: A Guide for Prescribers, Therapists, Patients and Their Families by Peter R. Breggin MD
- 14, 15 Injury.findlaw.com, Prozac Lawsuits
- 16 UIA Inadequate Testing of Drugs
- 17 Breggin.com Legal Page
- 18 Full Measure March 17, 2019
- 19, 30, 31 Aeon, Do Antidepressants Work?
- 20 JAMA. 2010;303(1):47-53
- 21 PLOS Medicine February 26, 2008
- 22 Science Translational Medicine January 8, 2014: 6(218):218ra5
- 23 Quartz December 29, 2017
- 24 Prevention & Treatment 1998; 1(2), article ID 2a
- 25 JAMA 2010 Jan 6;303(1):47-53
- 26, 29 J Clin Psychiatry. 2011 Apr;72(4):464-7
- 27 Zeitschrift fur Psychologie 2014; 222(3): 128–134
- 28 PLoS Med. 2008 Feb;5(2):e45
- 32 Psychotherapy and Psychosomatics 2017;86:302-304
- 33 Psychosom Med. 2000 Sep-Oct;62(5):633-8
- 34 Z Psychology 2014; 222(3): 128–134
- 35 Mayo Clinic, Monoamine Oxidase Inhibitors
- 36 Drugs.com, Zoloft Side Effects
- 37 PLOS One July 31, 2017
- 38 Diabetologia. 2012 Jan;55(1):63-72
- 39 Emory April 4, 2011
- 40 Indian J Pharmacol. 2015 May-Jun;47(3):256-62
- 41 J Clin Psychiatry. 2016 Jan;77(1):117-22; quiz 122
- 42 Wellness Resources October 9, 2017
- 43 Journal of Alternative and Complementary Medicine March 1, 2017; 23(3)
- 44 Scientific Reports July 27, 2017; 7, Article Number: 6287
- 45 Translational Psychiatry (2016) 6, e756
- 46 Psychother Psychosom. 2004 Nov-Dec;73(6):334-9
- 47 Nutritionfacts.org March 30, 2017
- 48 American Journal of Psychiatry January 1, 2017; 174(1): 42-50
- 49 Vice August 9, 2017
- 50 PLOS One June 27, 2017
- 51 The Journal of Nutrition, Health & Aging 1999, 3(1):5-7
- 52, 54 Journal of Internal Medicine 264(6); 599-609
- 53, 55 Michigan State University October 7, 2014
- 56 JAMA Psychiatry November 18, 2015. doi:10.1001/jamapsychiatry.2015.2235
- 57 Traumatology September 1, 2012; 18(3)
- 58 Depression Research & Treatment, 2012. doi:10.1155/2012/257172
- 59 Veteran Stress Project, EFT
- 60 Lissa Rankin April 15, 2013
- 61 Journal of Chemical Neuroanatomy September 2016; 75 Part B: 43-51
- 62 Clin Exp Immunol. 2019 Sep; 197(3): 308–318
- 63 Proc Natl Acad Sci U S A. 2011 Sep 20;108(38):16050-5
- 64 Psychology Today, December 3, 2009
- 65 Applied Psychophysiology and Biofeedback 2000;25(2): 117
- 66 Psychology Today, October 26, 2011
- 67 Choosing Therapy. CBT for Depression: How It Works June 21, 2022
- 68 Journal of Human Behavior in the Social Environment 2012; 22:463
- 69 Eur Psychiatry. 2003 Feb;18(1):23-7
- 70 Depressionalliance.org, Ecotherapy
- 71 Neuropsychiatr Dis Treat. 2016; 12: 1715–1723
- 72 NIH. St. John’s Wort and Depression: In Depth. December 2017
- 73 Orvosi Hetilap 2011 Sep 11;152(37):1477-85
- 74 Evid Based Complement Alternat Med. 2021; 2021: 5516525
- 76 The Antidepressant Solution: A Step-by-Step Guide to Overcoming Antidepressant Withdrawal, Dependence, and Addiction by Joseph Glenmullen
- 77 SAMSHA 2022
Exercising Only on Weekends Still Reduces Risk of Death
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2022/07/29/weekend-warriors.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate, and will not be bullied into removing it.
Analysis by Dr. Joseph Mercola Fact Checked July 29, 2022

STORY AT-A-GLANCE
- The benefits of exercise are many, including reducing the risk of death; data show even weekend warriors had reduced all-cause and cause-specific mortality rates when compared to people who did not get 150 minutes of moderate exercise each week
- Exercise also promotes the benefits of quality sleep, stress reduction and improved mental health. It helps boost self-confidence and normalizes glucose, insulin and leptin levels
- The data are helpful for those who can’t exercise every day after work. Other activities that do not take an extended period but also improve longevity are balance exercises, sauna bathing and inspiratory muscle strength training
According to the Centers for Disease Control and Prevention,1 all adults should get at least 150 minutes of aerobic physical activity every week. They recommend 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise. However, according to the American Heart Association,2 only 1 in 5 adults and teenagers is meeting this goal.
Research3 published in July 2022 in JAMA Internal Medicine finds that even weekend warriors who pack 150 minutes of exercise into two days enjoy lower all-cause and cause-specific mortality rates. One study4 published in the European Journal of Preventive Cardiology showed that exercise variables are a powerful predictor of survival, and health care providers could consider using physiological age to motivate patients to exercise more.5
Another study6,7 looked at 8,000 middle-aged older adults and found that physical activity of any intensity or duration cut their risk of early death. The results from these studies are encouraging — exercise promotes longevity. However, it’s also important to remember that you cannot out-exercise your diet.
In other words, a diet based on processed junk food will reduce your chance of getting fit and staying healthy. The good news is that research published in the Journal of the American College of Cardiology8 demonstrates a diet of minimally processed foods markedly blunts an increase in inflammation, glucose and triglycerides after a single meal. Research also demonstrates those who pack their exercise into the weekend also experience benefits.9
Packing Exercise Into the Weekend Reduces Risk of Death
The researchers began by asking the question of whether getting all your physical activity within one to two sessions on the weekend versus getting it more often during the week would influence mortality.10 They gathered data from 350,978 adults, in which they did not find any significant differences in mortality rates.
However, when active groups were compared with physically inactive participants, the data showed that the active participants had lower mortality rates. The participants were adults who reported their physical activity to the U.S. National Health Interview Survey between 1997 and 2013.
They were grouped into those who got less than 150 minutes of exercise per week, classified as physically inactive, and those who were physically active who got more than 150 minutes of moderate or 75 minutes of vigorous activity per week. The active group was then further broken down into those who got all their exercise on the weekend and those who regularly exercised throughout the week.
The main outcome measures were mortality rates, including cardiovascular disease, cancer and all-cause mortality. The research suggests that active individuals have a lower rate of mortality than inactive individuals and that those who were weekend warriors or regularly active did not experience significant differences in all-cause or cause-specific mortality.
Leandro Rezende, adjunct professor of epidemiology in the department of preventive medicine at the Federal University of Sao Paulo in Brazil, wrote in an email to Pittsburgh Action News 4:11
“This is good news considering that the weekend warrior physical activity pattern may be a more convenient option for many people to achieve the recommended levels of physical activity.”
Exercise Does More Than Promote Longevity
While the results of this study identified how exercise promotes longevity, even in those who exercise only on the weekend, research also demonstrates that exercise has other significant benefits in your daily life. For example, sleep is essential to your overall health.
Yet, surveys12 conducted by the National Sleep Foundation found that at least 40 million Americans report experiencing sleep disorders and 60% have had sleep problems for a few nights a week or more.
However, this lack of sleep affects nearly every aspect of your physical and mental functioning, as well as your metabolism and risk for chronic disease.13 Research has found an association between exercise and an individual’s quality of sleep. Exercise increases total sleep time and delayed REM sleep onset.14
An analysis of 34 studies15 found mixed results for young adults and younger. However, in middle-aged and elderly adults, exercise promoted sleep efficiency, especially in populations of individuals with disease. They concluded, “Our review suggests that sleep and exercise exert substantial positive effects on one another.”16
Data has also proven that exercise has mental health benefits, reducing anxiety, stress and depression.17 In one study18 published in 2019, researchers evaluated the effect of exercise in 60 patients with Type 2 diabetes over 12 weeks. They found that regular aerobic training was an effective strategy for improving mental health, improving life quality and self-esteem.
Another study19 published in Frontiers in Pharmacology in 2017 wrote that although academics and health care professionals may view “exercise as medicine” skeptically, randomized controlled trials comparing exercise to antidepressants reported both were equally as effective. Exercise also has benefits for your skin, including promoting wound healing.20 It also may attenuate age-associated skin changes.21
Exercise also benefits those suffering from chronic diseases22 such as osteoarthritis,23 depression, anxiety and cancer.24 Additionally, exercise helps normalize your glucose, insulin and leptin levels,25 and boosts your self-confidence.26
One of the challenges to exercising people encountered throughout the week was a lack of time. CNN fitness contributor and certified strength and conditioning specialist Dana Santas, spoke with Pittsburgh Action News 4, acknowledging this, saying:27
“Understandably, they don’t want to sacrifice much-needed sleep by getting up early or lose invaluable family dinner time by going to the gym right after work. Those are valid concerns as we all need sleep to function. And family dinners not only represent quality time but also increase the odds of eating healthy as opposed to grabbing fast food.”
Practicing Balance Powers Your Independence
While time can be a challenge, there are several strategies you may consider that can easily be integrated into your daily routine and which have impressive benefits. A growing body of research has demonstrated that your balance is directly associated with longevity.28 A study29 published in the British Journal of Sports Medicine found that people who fail a 10-second one-leg stance balance test are nearly twice as likely to die in the following 10 years.
The researchers assessed 1,702 people between the ages of 51 and 75 from 2008 to 2020. During a seven-year median follow-up, the data showed those who could not perform a 10-second one-legged stance had lower survival rates, even after adjusting for body mass index, age, sex and other comorbidities.
The researchers believe that using a 10-second one-legged stance in addition to other prognostic information may offer the primary care provider important information during routine physical examinations of middle-aged and older adults.30 Internal medicine physician Michael Roizen, author of “The Great Age Reboot,” believes that your balance is so closely tied to longevity because of the required neurological connections. He says:31
“Keeping your balance requires more complicated connections than a 60-person family. You have sensors throughout your limbs that interact with position sensors in your ears and others in your eyes, all of which are integrated in an area in the back of your brain called your cerebellum and in motor nerves that send messages to all your skeletal muscles to keep you upright.”
Family-practice physician Dr. Danine Fruge, medical director at Pritikin Longevity Center, believes the one-legged stance test is a better indication of a person’s longevity than their ability to walk well. Three pathways appear to impact how balance is related to your longevity.32 What may be the most obvious connection is physical fitness.
More active people may be more active because they do not have underlying medical conditions. Roizen also believes that the connections that foster good balance are linked to cognitive function. Balance is associated with memory and spatial cognition,33 which may strengthen and boost neuroplasticity.
Finally, balance relies on proprioceptive signals, which are sent from your peripheral nervous system to your brain telling your body where it is in space. A person with poor balance will have lost some of their proprioceptive ability, which can be related to chronic illnesses such as diabetes or transient ischemic attacks (TIA).34
A lack of balance in the elderly can lead to falls associated with broken hips and a higher rate of death. While balance is linked to longevity, it is also practically necessary for older adults to remain independent and live at home.35 A loss of independence can lead to destructive behavior, depression and anger.
The simplest way to improve your balance is to practice balance. As a starting point, consider simply standing on one leg while facing a corner so you can catch yourself if you begin to lose your balance.
As you become more confident, practice while you’re doing other tasks that require upper-body movement, such as washing dishes. Take care to alternate the leg you are balancing on. The key is to keep the exercises challenging and to do them daily. One of the benefits of balance exercises is that you can easily incorporate them into your daily activities.
Sauna Use Mimics Cardiovascular Activity
Sauna bathing is another strategy that mimics exercise and can increase your longevity and health. Data36 show that men who used Finnish-style, dry heat sauna seven times per week had a significantly reduced risk of death from fatal heart problems as compared to those who only used it once a week.
Even after confounding factors were eliminated, such as cholesterol, smoking and high blood pressure, the results held true. Heat stresses your heart and body in a similar way to exercise and thus may prompt similar effects. This could include increasing blood flow to the heart and muscles and increasing muscle mass due to higher levels of heat shock protein and human growth hormone (HGH).37
A study38 published in 2018, looked at stroke risk over 14.9 years and found a dose-dependent effect. In other words, those who used the sauna longer had an increasingly reduced risk of stroke.
Heat stress from sauna bathing has also been shown to lower your risk of high blood pressure. In one study39 with a median follow-up of 24.7 years, data showed “Regular sauna bathing is associated with reduced risk of hypertension, which may be a mechanism underlying the decreased cardiovascular risk associated with sauna use.”
When you don’t have time for a full workout after work, consider popping into a sauna for 20 minutes. There are several different types of saunas from which to choose and different health benefits you receive from Finnish-style wet and dry saunas, near-infrared and far-infrared light sources.
Research has demonstrated that a sauna can modulate your autonomic nervous system,40 which governs your stress responses.41 Using a sauna during the week can go a long way toward improving your health and increasing your lifespan. While there are significant cardiovascular benefits, there are others as well, including pain reduction,42 increased metabolism,43 detoxification44 and stress reduction.45
IMST Promotes Brain and Heart Health
Inspiratory muscle strength training (IMST) is another form of exercise that can help lower blood pressure, improve cardiovascular health and boost cognitive and physical performance without taking more than five minutes each day.46 Researchers know that the way that you breathe has a significant impact on your health.
Inspiratory muscle training is a technique that helps strengthen your respiratory muscles by using a handheld device that restricts airflow. In other words, by breathing through the device, you must work harder to breathe, and this strengthens the muscles used for inhalation.
The trainer was originally developed for people who had respiratory conditions and to help wean patients off mechanical ventilation. As you might expect, any time you do not use your muscles, you lose strength, including your respiratory muscles.
Preliminary results from one study were presented at the Annual Experimental Biology Conference in 2019.47,48 The researchers analyzed how IMST could affect your cognitive, vascular and physical health. The researchers engaged middle-aged adults who were inactive and found those who used the device lowered their blood pressure and improved their vascular health.
The data also showed those using IMST improved their exercise tolerance as assessed on a treadmill test and showed improved cognitive testing as well. Several types of breathing techniques are helpful to improve your cardiovascular, respiratory and autonomic nervous systems.49 As noted in one study:50
“Controlled, slow breathing appears to be an effective means of maximizing HRV [heart rate variability] and preserving autonomic function, both of which have been associated with decreased mortality in pathological states and longevity in the general population.”
These are just a few of the ways that you can integrate activities throughout your day and week that have cardiovascular, respiratory, and cognitive benefits, all of which contribute to increasing your quality of life and longevity.
- 1 Centers for Disease Control and prevention, June 3, 2022
- 2 American Heart association, April 18, 2018
- 3, 9, 10 JAMA Internal Medicine, July 5, 2022; doi.org/1001/jamainternmed.2022.2488
- 4 European Journal of Preventive Cardiology, 2019; doi.org/10.1177/2047487319826400
- 5 Cleveland Health, February 15, 2019
- 6 American Journal of Epidemiology, 2019;188(3)
- 7 EurekAlert! January 14, 2019
- 8 Journal of the American College of Cardiology, 2008; 51(3)
- 11, 27 Pittsburgh Action News 4, July 11, 2022
- 12 American Psychological Association, Why Sleep Is Important
- 13 University of Michigan School of Public health, March 2, 2020
- 14 Sleep medicine reviews, 2000; 4(4)
- 15, 16 Advances in Preventive Medicine, 2017;2017
- 17 Maturitas, 2017;106
- 18 Health Psychology Research, 2019; 7(1)
- 19 Frontiers in Pharmacology, 2017; 8
- 20 Wounds, 2019;31(2)
- 21 Aging Cell, 2015;14(4)
- 22 Sports Medicine and Health Science, 2019;1(1)
- 23 Arthritis Foundation, Benefits of Exercise for Osteoarthritis
- 24 American Cancer Society, Exercise and the Cancer Patient
- 25 BMJ Open Sport and Exercise Medicine, 2016;2(1)
- 26 Neuropsychiatric Disease and Treatment, 2016;12:2617
- 28 NBC News, June 21, 2022
- 29, 30 British Journal of Sports Medicine, 2022; doi.org/10.1136/bjsports-2021-105360
- 31, 32, 34 Well and Good, July 9, 2022
- 33 Scientific Reports, 2017;7
- 35 Vantage, Reasons Independence is Important for Seniors
- 36 JAMA Internal Medicine 2015;175(4):542
- 37 Current Opinion in Endocrine and Metabolic Research, 2020;11
- 38 Neurology, 2018; 90(22)
- 39 American Journal of Hypertension 2017 Nov 1;30(11):1120
- 40 Complementary Therapies in Medicine 2019 Aug;45:190
- 41 Harvard Health Publishing March 2011, Updated May 1, 2018
- 42 Anesthesia and Pain Medicine, 2019;14(4)
- 43 International Journal of Environmental Research and Public Health, 2021;18(3)
- 44 Journal of Environmental and Public Health, 2012;2012
- 45 The Conversation, July 30, 2019
- 46 CU Boulder Today, February 25, 2019
- 47 Science Daily April 8, 2019
- 48 Inverse, April 9, 2019
- 49, 50 Breathe (Sheff). 2017 Dec; 13(4): 298
Top Breathing Techniques for Better Health
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2022/07/29/best-breathing-techniques.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate, and will not be bullied into removing it.
Analysis by Dr. Joseph Mercola Fact Checked July 29, 2022

STORY AT-A-GLANCE
- The way you breathe — fast or slow, shallow or deep — sends messages to your body that affect your mood, stress level, blood pressure, immune function and more
- One of the most basic of all breathing techniques is to make sure you’re always breathing through your nose. Mouth breathing decreases tissue oxygenation, elevates your heart rate and blood pressure and has many other adverse health effects
- Most people chronically over breathe. Breathing less is a sign of better health. Conversely, the more you breathe, the more likely you are to experience significant health problems
- Another near-universal breathing abnormality is breathing vertically rather than horizontally, which triggers your sympathetic nervous system and makes you feel stressed
- Several breathing techniques are reviewed, including proper breathing basics, a technique to improve your body’s tolerance to carbon dioxide, the 4-7-8 breathing method to improve sleep, the Buteyko Breathing Method to ease stress and anxiety, and many more
This article was previously published January 31, 2019, and has been updated with new information.
Breathing wields incredible power over your health, as it supplies your body with oxygen and removes excess carbon dioxide (CO2) to keep you alive. However, the way you breathe — whether fast or slow, shallow or deep — also sends messages to your body that affect your mood, stress level, blood pressure, immune function and more.
What’s interesting about breathing is that it’s both a voluntary and an involuntary process. While your body breathes automatically, you also have the ability to consciously control your breathing — the speed, the depth and whether you breathe through your mouth or your nose.
So, simply by changing the way you breathe, you can actually influence your health in a variety of ways. Here, I review some of the most important basics of proper breathing, and share several effective controlled breathing techniques shown to have a positive impact on health and psychological well-being.
Always Breathe Through Your Nose — Even During Exercise
Perhaps the most basic of all breathing techniques is to make sure you’re always breathing through your nose. Mouth breathing tends to promote hyperventilation, which actually decreases tissue oxygenation. Mouth breathing also results in diminished levels of CO2 in your body and a decreased ability to filter toxic pollutants from the air.
Your body needs a balance of oxygen and CO2 for optimal function. CO2 is not just a waste product but has actual biological roles, one of which is assisting in oxygen utilization. When your CO2 level is too low, changes in your blood pH impair your hemoglobin’s ability to release oxygen to your cells (the Bohr effect).1,2
Mouth breathing can also elevate your heart rate and blood pressure, sometimes resulting in fatigue and dizziness.3 The elasticity of your lungs also depends on nasal resistance, which you only get from nasal breathing due to the smaller diameter of your nasal passages.4 Poor breathing is even associated with poor posture.
So, breathing through your nose helps maintain your health in a number of important ways. While huffing and puffing through your mouth may be particularly tempting during physical exertion, really try to avoid this tendency. You should be exercising only to the extent that you can continue breathing through your nose the vast majority of the time.
If this means backing off on intensity, then that’s what you need to do, realizing that it’s only temporary until your body begins to adjust to your slightly increased CO2 levels, which will happen fairly quickly. You just have to get used to “air hunger” (an admittedly uncomfortable feeling of mild suffocation), and realize it’s normal and safe.
So, the rule of thumb is to not push yourself to the point where you are unable to maintain nasal breathing. If you feel the need to open your mouth, then slow down and recover. This helps your body to gradually develop a tolerance for increased CO2.
Assess Your CO2 Tolerance
There’s a simple self-test for estimating your body’s tolerance to CO2. Dr. Konstantin Pavlovich Buteyko,5 a Russian physician, discovered that the level of CO2 in your lungs correlates to your ability to hold your breath after normal exhalation. You can use a stopwatch or simply count the number of seconds to yourself. Here is the process:
- Sit straight without crossing your legs and breathe comfortably and steadily.
- Take a small, silent breath in and out through your nose. After exhaling, pinch your nose to keep air from entering.
- Start your stopwatch and hold your breath until you feel the first definite desire to breathe.
- When you feel the first urge to breathe, resume breathing and note the time. The urge to breathe may come in the form of involuntary movements of your breathing muscles, or your tummy may jerk or your throat may contract.
- Your inhalation should be calm and controlled, through your nose. If you feel like you must take a big breath, then you held your breath too long.
The time you just measured is called the “control pause” or CP, which reflects the tolerance of your body to carbon dioxide. Here are the criteria for evaluating your CP:
• CP 40 to 60 seconds — Indicates a normal, healthy breathing pattern and excellent physical endurance.
• CP 20 to 40 seconds — Indicates mild breathing impairment, moderate tolerance to physical exercise and potential for health problems in the future (most folks fall into this category).
To increase your CP from 20 to 40, physical exercise is necessary. You might begin by simply walking with one nostril occluded. As your CP increases, begin incorporating jogging, cycling, swimming, weightlifting or anything else to build up an air shortage.
• CP 10 to 20 seconds — Indicates significant breathing impairment and poor tolerance to physical exercise; nasal breath training and lifestyle modifications are recommended. If your CP is less than 20 seconds, never have your mouth open during exercise, as your breathing is too unstable. This is particularly important if you have asthma.
• CP under 10 seconds — Serious breathing impairment, very poor exercise tolerance and chronic health problems.
Short CP times correlate with low tolerance to CO2 and chronically depleted CO2 levels. As a result, the shorter your CP, the more easily you’ll get breathless. The good news is that you will feel better and improve your exercise endurance with each five-second increase in your CP.
Improve Fitness and Endurance by Raising Your CO2 Tolerance
The first step to increase your CP is to learn how to unblock your nose with the following breath hold exercise. While this exercise is perfectly safe for most, if you have any cardiac problems, high blood pressure, are pregnant, have Type 1 diabetes, panic attacks or any serious health concern, then do not hold your breath beyond the first urges to breathe.
- Sitting up straight, take a small breath in through your nose and a small breath out. If your nose is quite blocked, take a tiny breath in through the corner of your mouth.
- Pinch your nose with your fingers and hold your breath. Keep your mouth closed.
- Gently nod your head or sway your body until you feel that you cannot hold your breath any longer.
- When you need to breathe in, let go of your nose and breathe gently through it, in and out, with your mouth closed.
- Calm your breathing as soon as possible. Repeat this exercise several times in succession, waiting 30 to 60 seconds between rounds. Also, be sure to do it on a regular basis, ideally daily.
Breathe Less and More Lightly
While “breathe less” might sound like a terrible recommendation, most people chronically over breathe, meaning they breathe more than is needed, which depletes their carbon dioxide reserves. Typical characteristics of over breathing include mouth breathing, upper chest breathing, sighing, noticeable breathing during rest, and taking large breaths prior to talking.
Clinical trials6 involving asthmatics show they breathe between 10 to 15 liters of air per minute and people with chronic heart disease tend to breathe between 15 to 18 liters of air per minute. On the other hand, normal breathing volume is between 4 and 7 liters of air per minute, which translates into 12 to 14 breaths.
This suggests breathing less is a sign of better health. Conversely, the more you breathe, the more likely you are to experience significant health problems. What’s more, if you are breathing through your mouth during the day, odds are you’re also doing so at night, which can lead to health problems such as dehydration, snoring and sleep apnea.7,8,9,10,11,12 Mouth breathing is associated with several other health problems, including:
- Bronchial asthma and exercise-induced asthma — In one study,13 asthma patients had remarkably reduced asthma after exercising while breathing through their noses. However, they did experience moderate bronchial constriction after exercising while mouth breathing.
- Abnormal facial development — Children who breathe through their mouths tend to develop longer faces with altered jaw structures.14,15,16,17,18,19
- Poor oral hygiene — Loss of moisture dries out your saliva and contributes to poor oral hygiene; dehydration causes your airways to constrict and makes nose breathing even more difficult, creating a vicious cycle.
- Reduced oxygen delivery to your heart, brain and other tissues due to constricted arterial blood flow.20
- Crooked teeth, poor concentration, allergies, poor sports performance and ADHD have also been linked with mouth breathing.
The trick to minimize these problems is to breathe more lightly, and this happens automatically when you shift from breathing through your mouth to your nose. Remember, the deeper and more quickly you breathe, the more constricted your blood vessels will be and the less oxygen will be delivered to your tissues.21
Breathing through the nose, on the other hand, slows down and regularizes your breathing, thereby improving oxygenation. Nasal breathing also has a calming effect because it activates your parasympathetic nervous system.22,23
Three Steps to Proper Breathing
The following steps will help your breath become lighter, such that the hairs in your nose barely move. Again, this type of light breathing helps you to enter and remain in a calm, meditative state while lowering your blood pressure and reducing nasal congestion for easier breathing.
You may feel a slight air shortage at first, but this should be tolerable. If it becomes uncomfortable, take a 15-second break and then continue.
- Place one hand on your upper chest and the other on your belly; feel your belly move slightly in and out with each breath, while your chest remains unmoving.
- Close your mouth and breathe in and out through your nose. Focus your attention on the cold air coming into your nose and the slightly warmer air leaving it on the out breath.
- Slowly decrease the volume of each breath, to the point it feels like you’re almost not breathing at all (you’ll notice your breath getting very quiet at this point). The crucial thing here is to develop a slight air hunger. This simply means there’s a slight accumulation of carbon dioxide in your blood, which signals your brain to breathe.
After three or four minutes of air hunger, you’ll start experiencing the beneficial effects of CO2 accumulation, such as an increase in body temperature and an increase in saliva. The former is a sign of improved blood circulation, the latter a sign that your parasympathetic nervous system has been activated, which is important for stress reduction.
Breathe Horizontally, Not Vertically
Another near-universal breathing abnormality is breathing vertically rather than horizontally. This is something clinical psychologist Belisa Vranich points out in her book “Breathe,” which details her breathing program.
Vertical breathing makes you feel a bit taller on the in-breath, as it raises your chest and shoulders. The problem is that this kind of breathing actually triggers your sympathetic nervous system, basically signaling your body that you’re stressed.
Correct breathing will cause your midsection to widen, while not raising your shoulders or puffing out the upper part of your chest. This is the horizontal breath. At first, you may find it difficult to take a proper breath, as your midsection and diaphragm may be tight. To relearn proper horizontal breathing, Vranich suggests the following exercise:
- Begin by relaxing and unbracing your midsection.
- Take a deep breath in and actually feel the middle of your body get wider. Let your belly go.
- On the exhale, roll backward, tipping your hips underneath you while pressing your fingers gently into your belly, giving it a little squeeze.
Eventually, this exercise will teach your body to use the diaphragm to breathe. A related problem here is feeling short of breath, which is caused by insufficient exhalation that leaves excess residual air in your lungs.
Engaging your diaphragm and intercostals — the muscles that run between your ribs, allowing your chest wall to move — will allow you to take more complete in and out breaths. You can also train yourself to exhale more fully by making sure your exhale is slightly longer than your inhale, and by engaging your diaphragm to really squeeze the air out as you allow your midsection to collapse inward.
In the 4-7-8 exercise below, for example, your exhale is twice as long as your inhale. The condensed version of Vranich’s interview is included above for your convenience.
Improve Sleep With the 4-7-8 Breathing Exercise
Deep breathing activates your parasympathetic nervous system, which induces the relaxation response.24 There are many different breathing practices that will accomplish this, but the following is both powerful and easy to perform.
I first learned this exercise when I attended a presentation by Dr. Andrew Weil at the 2009 Expo West in California. Here’s a quick summary of the process.25 Weil also demonstrates the technique in the video above.
- Sit up straight.
- Place the tip of your tongue up against the back of your front teeth. Keep it there through the entire breathing process.
- Breathe in silently through your nose to the count of four.
- Hold your breath to the count of seven.
- Exhale through your mouth to the count of eight, making an audible “whoosh” sound.
- That completes one full breath. Repeat the cycle another three times, for a total of four breaths.
You can do this 4-7-8 exercise as frequently as you want throughout the day, but it’s recommended you don’t do more than four full breaths during the first month or so of practice. Later you may work your way up to eight full breath cycles at a time. The benefits of this simple practice are enormous and work as a natural tranquilizer for your nervous system.
Ease Stress and Anxiety With Controlled Breathing
Another powerful technique is the Buteyko Breathing Method, which will help reverse health problems associated with improper breathing, the most common of which are overbreathing and mouthbreathing. When you stop mouthbreathing and learn to bring your breathing volume toward normal, you have better oxygenation of your tissues and organs, including your brain.
The Buteyko Breathing Method and many other controlled breathing methods are also very effective for controlling anxiety and quelling panic attacks. As reported by Scientific American:26
“[R]espiratory techniques do not work only for acute stresses or sleep problems; they can also relieve chronic anxiety. They are particularly effective in people with psychiatric disorders such as phobias, depression and post-traumatic stress disorder …
Breathing exercises also help to counter the accumulation of minor physical tension associated with stress. Therapists recommend doing them regularly during the day, during breaks or at moments of transition between two activities: you simply stop to adjust your posture and allow yourself a few minutes of quiet breathing.
Therapists often suggest the ‘365 method’: at least three times a day, breathe at a rhythm of six cycles per minute (five seconds inhaling, five seconds exhaling) for five minutes. And do it every day, 365 days a year.
Some studies even suggest that, in addition to providing immediate relief, regular breathing exercises can make people less vulnerable to stress, by permanently modifying brain circuits.”
Research27 also shows the relaxation response enhances “expression of genes associated with energy metabolism, mitochondrial function, insulin secretion and telomere maintenance,” and reduces “expression of genes linked to inflammatory response and stress-related pathways.”
Scientific American lists six breathing techniques shown to relieve stress, anxiety and panic attacks, including alternate nostril breathing and abdominal breathing. The Buteyko Breathing Method is also indicated for this, as it allows you to retain and gently accumulate CO2, which calms breathing and reduces anxiety:
- Take a small breath into your nose, followed by a small breath out
- Hold your nose for five seconds in order to hold your breath, and then release your nose to resume breathing
- Breathe normally for 10 seconds
- Repeat the sequence
For Better Health, Control Your Breath
Typically, the respiratory rate of humans is about 10 to 20 breaths per minute. Slowing your breathing down to a rate of four to 10 breaths per minute appears to offer many benefits, however, including effects on the respiratory, cardiovascular, cardiorespiratory and autonomic nervous systems.28
Further, according to research29 published in the medical journal Breathe, optimized respiration in humans may be in the range of six to 10 breaths per minute, done in a way that activates your diaphragm. The researchers also note that nasal breathing (such as taught by the Buteyko method) “is also considered an important component of optimized respiration,” and that:
“Controlled, slow breathing appears to be an effective means of maximizing HRV [heart rate variability] and preserving autonomic function, both of which have been associated with decreased mortality in pathological states and longevity in the general population …
This is easily achievable in most individuals with simple practice and there is yet to appear in the literature any documented adverse effects of respiration in the 6 to 10 breaths per minute range.”
Aside from the techniques already mentioned, there are many others. Following is a short list of a few additional breathing methods you can try, all of which are backed by scientific evidence30 showing their beneficial influence on human health.
| Nadi Shodhana/Nadi Shuddhi (alternate nostril breathing) — With your right thumb, close the right nostril and inhale through your left nostril. Closing the left nostril, exhale through the right, following which, inhalation should be done through the right nostril. Closing the right nostril, breathe out through your left nostril. This is one round. The procedure is repeated for the desired number of rounds. |
| Surya Anuloma Viloma (right uninostril breathing) — Closing the left nostril, both inhalation and exhalation should be done through your right nostril, without altering the normal pace of breathing. |
| Chandra Anuloma Viloma (left uninostril breathing) — Similar to Surya Anuloma Viloma, breathing is done through your left nostril alone, by closing the right nostril. |
| Surya Bhedana (right nostril initiated breathing) — Closing the left nostril, inhalation should be done through your right nostril. At the end of inhalation, close the right nostril and exhale through the left nostril. This is one round. The procedure is repeated for the desired number of rounds. |
| Ujjayi (psychic breath) — Inhalation and exhalation are done through the nose at a normal pace, with partial contraction of the glottis, which produces a light snoring sound. You should be aware of the passage of breath through your throat during the practice. |
| Bhramari (female honeybee humming breath) — After a full inhalation, closing the ears using your index fingers, you should exhale making a soft humming sound similar to that of a honeybee. |
- 1 Buteyko.com FAQ
- 2 Concerning a Biologically Important Relationship – The Influence of the Carbon Dioxide Content of Blood on its Oxygen Binding
- 3 Biol Psychol. 1998 Sep;49(1-2):83-94
- 4 NIH STAT Pearls. Physiology, Airflow Resistance April 28, 2022
- 5 Buteyko.com
- 6 J Appl Physiol. 1995 Sep; 79(3): 892-901
- 7 Eur Arch Otorhinolaryngol. 2011 Apr;268(4):533-9
- 8 Respiration. 2010;80(6):488-94
- 9 Acta Otolaryngol Suppl. 1996;523:228-30
- 10, 11 Laryngoscope. 2007 Jun;117(6):1102-6
- 12 Ann Allergy Asthma Immunol. 1998 Oct;81(4):279-87; quiz 287-90
- 13 Clin Allergy 1981 Sep;11(5):433-9
- 14 American Journal of Orthodontics April 1983; 83(4): 334-340
- 15 Angle Orthod 1990 Fall; 60(3): 167- 76
- 16 Laryngoscope 2010 Oct; 120(10): 2089-93
- 17 Braz J Otorhinolaryngol. 2011 Sep-Oct; 77(5):656-62
- 18 J Bras Pneumol. 2011 Jul-Aug; 37(4)):471-9
- 19 Journal Pediatrics (Rio J) 2011 Jul-Aug; 87(4)):471-9
- 20 Western Journal of Medicine 1983 May; 138(5): 733–736
- 21 American Journal of Psychiatry 1992 Nov;149(11):1589-91
- 22 Conf Proc IEEE Eng Med Biol Soc. 2007: 5323-5325
- 23 Indian J Med Research 2004 Aug;120(2):115-2
- 24, 26 Scientific American January 15, 2019
- 25 Drweil.com, Breathing Exercises: 4-7-8 Breath
- 27 PLOS One May 1, 2013
- 28, 29 Breathe (Sheff). 2017 Dec; 13(4): 298–309.
- 30 J Ayurveda Integr Med. 2018 Jan 30. pii: S0975-9476(17)30322-4