Supplements
now browsing by category
Why Herbal Supplements Are Facing Increased Scrutiny Today
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2026/01/17/herbal-supplements-new-compliance-rules.aspx
Analysis by Dr. Joseph Mercola January 17, 2026

Story at-a-glance
- Almost 80% of Americans take supplements — and that number keeps growing. It’s no surprise supplements are everywhere. Herbal products alone bring in more than $12 billion a year
- The U.S. supplement industry is raising safety standards without banning trusted herbs. Experts advocate for clearer rules, improved testing, and consumer protection while maintaining access to beneficial natural products
- Europe is reversing course, with new European Union (EU) rules possibly requiring reformulations, restricting online sales, and limiting access to ingredients like ashwagandha
- Supplements have an exceptional, long-standing safety record, with serious adverse effects being rare compared to many medications
- In contrast to pharmaceuticals, which carry FDA-mandated “black box” warnings for known lethal risks, there has never been a confirmed death recorded as the direct result of taking a dietary supplement as intended
Over 70% of Americans take supplements today, and that number continues to rise.1 This modern trend has deep historical roots: For thousands of years, people have relied on plants and herbs for healing, with evidence stretching back at least 5,000 years in Egyptian medical texts and Ayurvedic traditions.2
Ancient remedies are reemerging in new forms as researchers examine their effects, and companies develop convenient products for daily use. The industry’s growth highlights a renewed interest in natural health. Annual sales of herbal supplements climbed past $15 billion in 2024, according to the American Botanical Council’s 2023 Herb Market Report — a $533 million increase from the previous year.3
As more consumers turn to botanicals, regulators are responding. Some countries are tightening controls, while others focus on improving safety without pulling products from shelves.
What’s Changing in the US Supplement Landscape
A panel of industry leaders featured in Nutritional Industry Executive’s (NIE) Winter 2025 Roundtable discussed the current state of the U.S. supplement industry.4 They shared recent wins, emerging risks, and how regulators and companies are shaping the future of natural health.
• The FDA reversed its nicotinamide mononucleotide (NMN) ruling after industry pushback — In September 2025, the U.S. Food and Drug Administration (FDA) reversed course on NMN, reclassifying it as a lawful dietary supplement after a two-year ban. This landmark decision followed a joint citizen petition from the Natural Products Association (NPA) and Alliance for Natural Health USA.5
“FDA has moved back to accepting NMN as a dietary supplement … NMN is now in great shape to be sold and marketed by reputable brands,” said Jim Emme, CEO of NOW Health Group.
• Industry leaders support clearer rules and guidelines — Across the board, U.S. experts favor firm but fair standards. Dr. Daniel Fabricant, president & CEO of the NPA, commented:6
“NPA is committed to supporting Secretary Kennedy’s goals while remaining wary of proposals with unintended consequences that would stymie dietary ingredient innovation, impose undue burdens on our members, or restrict access to legitimate dietary supplement products.”
• Economic pressure is reshaping ingredient sourcing — Tariffs are driving up costs and complicating long-term supply planning, especially for herbs sourced overseas. Loren Israelsen, president of the United Natural Products Alliance (UNPA), shared her thoughts:7
“It’s not a good situation. The most common concern I hear is the level of uncertainty that the tariff policy has created. We had several problems. Traditionally, the average tariff rate for natural ingredients was between 0 and 6 percent.
Today, we’re now looking at numbers ranging from 35 to 100 percent depending on the country. So, we have a tremendous increase, very suddenly. We also have a policy and procedural question of how the White House is conducting tariff and trade policy. Previously, tariff rates were a long, drawn-out process.”
• FSA and HSA reform could be a game-changer — Leaders also discussed IRS proposals that would let consumers use Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA) to buy supplements without needing a doctor’s note. “It would be the single best thing we could do to help reduce the cost of products,” Israelsen said.8
• MAHA opens the door for natural health expansion — The Make America Healthy Again (MAHA) initiative, led by Secretary Robert F. Kennedy Jr., is elevating national attention to nutrition, clean ingredients, and preventive wellness. Many believe this could lead to better acceptance of natural products — as long as the reforms stay focused on access, not restriction.
• What’s next for the industry? — In the next six months, leaders expect changes to tariffs, clearer guidance from the FDA on Generally Recognized as Safe (GRAS) standards and New Dietary Ingredient (NDI) rules, and updates to ingredient approval pathways.9
Many hope for fewer restrictions to encourage innovation, while others see more scrutiny and a stronger push for clinically proven formulas. Karen Howard, CEO and executive director of the Organic & Natural Health Association (ONHA) said:10
“Realistically, our challenges remain the same, only bolstered with steroids. If the industry wants to affect true change, it needs to listen and learn from what the retailer and the customer want and need, and deliver it in full.”
The U.S. supplement industry is prioritizing quality and self-regulation by investing in testing, sustainability, and third-party verification. Industry leaders are advocating for smarter oversight that protects consumers and preserves access to trusted herbs.
Why Europe Is Taking a Harder Line on Herbal Supplements
Meanwhile, in the European Union (EU), a wave of new regulations is reshaping the supplement market. In her Substack page Einfodemic, Maia Romanowska, an infodemic expert,11 explains how the 2025 changes mark a sharp pivot toward safety-first policies, particularly targeting herbal products and natural health claims.
• Stricter labeling and health claims — Only health claims approved by the European Food Safety Authority (EFSA) can appear on packaging, and traditional herbal claims need to include a clear disclaimer: “This claim is based on traditional use and has not been evaluated by EFSA.” Labels are now required to show full ingredient details, standard dosage, usage warnings, and nutrient reference values to improve transparency and consumer trust.12
• Ingredient bans and restrictions — Several botanicals are under review for safety concerns. Alpha-lipoic acid (ALA) may face a full ban, monacolins from red yeast rice could be heavily restricted, and high-dose green tea extracts and Garcinia cambogia are flagged for liver risk.13
• Tighter oversight of botanicals — National authorities can now demand reformulation or removal of products using high-risk herbs or non-approved claims.14
• Focus on sustainability and novel foods — New ingredient applications are required to include safety, bioavailability, and sustainability data. Plant-based formats like vegan softgels, phytosomes, and eco-friendly formulations are being prioritized as the EU pushes for greener innovation in supplements.15
• Stricter rules for online and cross-border sales — Supplements sold online to EU consumers, even from outside the EU, need to meet safety and labeling laws. Under the Digital Services Act (DSA), platforms like Amazon and eBay are liable for listing banned or non-compliant products, tightening enforcement.16
• Risk of a black market — Critics warn that overly strict rules could push consumers toward unregulated websites and foreign sellers, where products may contain unsafe or mislabeled ingredients. The EU plans to counter this with stronger enforcement, consumer education, and transparency campaigns.17
• Penalties for non-compliance — Products that fail to meet 2025 standards can be recalled, seized at customs, or banned from future sales. Companies may face heavy fines, sanctions, and even legal liability for consumer harm, making compliance a top priority for manufacturers.18
• Impact on traditional systems — Natural remedies from Ayurveda or Traditional Chinese Medicine (TCM) can still be sold in the EU, but they need to comply with all safety, labeling, and claim requirements. Ingredients not used in the EU before 1997 require Novel Food approval, and all traditional-use claims are required to carry the correct disclaimer.19
The EU is moving toward a safety-first, claim-limited model that may block consumer access to popular supplements. While their intent is protection, the result could be over-regulation of low-risk herbs, such as ashwagandha.

Save This Article for Later – Get the PDF Now
How the EU’s Regulatory Crackdown Is Affecting Popular Herbal Remedies
Following these broader shifts, the RegASK 2023 to 2025 Global Regulatory Overview20 shows that Europe is already targeting herbal supplements like ashwagandha with outright bans. The data paints a picture of rising pressure and fragmented enforcement.
• Denmark lit the fuse in 2023 — In April 2023, Denmark became the first EU country to ban ashwagandha outright, forcing all products off shelves after a risk review flagged hormonal and reproductive concerns.21
Within months, other nations began weighing restrictions. France issued warnings for vulnerable groups, Germany launched ongoing safety evaluations, and Sweden and Finland signaled possible action. The U.K. took a “wait-and-see” approach, demanding more data instead of an immediate ban.22
• Poland chose limits, not bans — While Denmark pulled the plug, Poland opted for a science-based compromise: capping ashwagandha at 3 grams (g) per day for root powder and 10 milligrams (mg) per day for standardized extracts.23
• Ashwagandha isn’t alone — Regulators are also targeting kratom, Tongkat Ali, and high-dose green tea extracts, citing liver toxicity and hormonal risks. Menopause herbs such as black cohosh, red clover, and dong quai are also under review.24
• Why the crackdown? — Ashwagandha’s popularity led to bans due to complex chemistry and reports of adverse events, often from contaminated products. Critics say these bans ignore the root issue: adulteration and poor-quality manufacturing.25
• Business impact is brutal — Companies face recalls, reformulation costs, and the nightmare of managing multiple product versions for different countries. One regulatory executive summed it up: “We went from managing one European formula to juggling eight different versions. The complexity alone nearly broke our operations team.”26
• How to stay ahead — Experts recommend three strategies: build bulletproof safety documentation, use real-time regulatory intelligence to anticipate changes, and diversify formulations so you’re not dependent on a single “hero” ingredient.27
What You Need to Know About Ashwagandha
Ashwagandha (Withania somnifera) is often talked about as a stress supplement, but that label barely scratches the surface. This herb affects multiple systems in the body, which is why it shows up in research on stress, hormones, brain health, inflammation, and recovery. To understand why ashwagandha has become so popular and remains a focus of scientific research, it’s helpful to consider its actual effects within the body.
• Ashwagandha has a 3,000-year medical track record — Ashwagandha translates to “smells like a horse” — a nod to its ability to promote stamina, vigor, and strength. But its other name, somnifera, meaning “sleep-inducing,” hints at its calming, sedative effects.28
In Ayurvedic medicine, ashwagandha is classified as a rasayana, an elixir used to promote health and longevity.29 It’s been used for everything from infertility and arthritis to cognitive decline and adrenal exhaustion.30
• This adaptogen helps your body normalize stress — Unlike synthetic stimulants or sedatives, ashwagandha supports the body’s stress response by stabilizing cortisol, balancing hormones, and modulating inflammation.31
• Its traditional uses cover a wide range of health concerns — In countries where Ayurveda is widely practiced — such as India, Nepal, and Malaysia — ashwagandha is used to treat inflammation, weakness,32 and sexual health issues in both men and women. Some texts even call it beneficial for “almost all disorders that affect human health.”33 Below are just a few of its most common applications:
◦ Improving stamina and energy levels
◦ Gastric ulcers and digestive issues
◦ Parkinson’s, Huntington’s, and Alzheimer’s disease
◦ Mitochondrial health and cellular repair
◦ Chronic inflammation
◦ Rheumatoid and osteoarthritis
◦ Muscle strength and physical recovery
◦ Lowering blood sugar levels
Additional uses recorded by herbal groups like the American Botanical Council include support for:34
◦ Memory loss and brain fog
◦ Childhood emaciation and fever
◦ Nervous exhaustion
◦ Impotence, seminal debility, and uterine tone
◦ Emphysematous dysphonia
◦ Colds and chills
If you want to know more about Ashwagandha’s great benefits, check out “Ashwagandha for Cognitive Function.”
Nutritional Supplements Have a Remarkable Safety Profile
Although a balanced diet is still the best way to maintain optimal wellness, many people, especially those dealing with stress, chronic conditions, or limited diets, often need help meeting their daily nutrient requirements.35 This is where supplements come in handy.
Nutritional supplements, which include vitamins, minerals, herbs, enzymes, amino acids, and probiotics, help fill nutritional gaps or support the body during stressful and busy times. They’re available in many forms (capsules, powders, teas, and gummies)36 and, when used thoughtfully, can contribute to healthier habits and better overall well-being.
Supplements are often portrayed as risky or loosely regulated. But when you look at the actual safety data, a very different picture emerges.
• They’re linked to far fewer deaths than prescription drugs — Despite frequent warnings about supplement risks, deaths associated with dietary supplements are extraordinarily rare37,38 when compared to pharmaceutical drugs. According to a 2012 analysis by the UK-based Alliance for Natural Health International (ANHI):39
“Nutritional supplements are the safest foodstuffs available; adverse reactions to pharmaceutical drugs are 62,000 times more likely to kill you than nutritional supplements.”
The ANHI calculated that the lifetime risk of dying from an herbal product or dietary supplement is less than 1 in 10 million — roughly the same odds as being struck by lightning. By contrast, prescription medications are consistently listed among the leading causes of death in developed countries.
• There is no confirmed record of deaths caused directly by supplements — In contrast to pharmaceuticals, which carry FDA-mandated “black box” warnings40 for known lethal risks, there has never been a confirmed death recorded as the direct result of taking a dietary supplement as intended.
• Media scares about supplements have repeatedly fallen apart — One high-profile example occurred in 2015, when CBC News aired a Marketplace report41 claiming that several supplement companies failed to meet label claims. Within two months, CBC was forced to issue a retraction after independent verification showed the testing methods were flawed and unreliable.42
• Supplements are regulated like food, not drugs — A common misconception is that dietary supplements are “unregulated.”43 In reality, they are regulated under a different framework. In the U.S., the FDA oversees both supplement ingredients and finished products, while the Federal Trade Commission44 (FTC) governs marketing and advertising claims.
Supplements are classified as foods, which is why they don’t need to undergo drug-style clinical safety trials before entering the market. Supplements don’t bypass regulation; they are regulated appropriately for what they are.
If you want to gain more awareness on how the pharmaceutical industry undermines the small wins of natural supplements, read “Big Pharma Wants to Put an End to Vitamins and Supplements.”
You shouldn’t have to fight for access to something that supports your health and well-being. In a time when helpful herbs are being banned instead of being better understood, there’s real value in keeping an open mind. Exploring natural alternatives gives you more options for feeling better without drugs, harsh side effects, or invasive interventions.
Instead of restrictions, it’s time to focus on smarter regulations, the kind that protect your safety and your choices. You deserve options, clarity, and above all, the chance to care for your health in a way that feels right for you.
Frequently Asked Questions (FAQs) About Supplement Regulations
Q: Why are more people turning to supplements nowadays?
A: Nearly 80% of Americans now take supplements — and it’s not just a trend. People are looking for natural ways to manage stress, improve sleep, and boost energy. With herbal products alone generating over $12 billion a year, it’s clear that more folks are turning to nature for real, lasting support.
Q: What is the U.S. doing to regulate herbs and supplements?
A: U.S. experts prefer improving safety data, labeling, and FDA regulations over banning ingredients. Their goal is to safeguard consumers while maintaining access to trusted herbs such as ashwagandha. The consensus among leaders is that it’s about reform rather than restriction.
Q: Why is Europe trying to restrict herbal supplements?
A: European regulators are tightening rules around health claims and herbal ingredients. Ashwagandha may be limited by a lack of EU-approved data, despite its strong safety record and long history of use.
Q: Can supplements aid in achieving a healthier lifestyle?
A: Even with a balanced diet, some people need extra support — especially during stress, illness, pregnancy, or aging. Supplements offer targeted nutrients to help fill common nutritional gaps and keep you feeling your best.
Q: Do supplements have a strong safety record compared to medications?
A: Yes. Dietary supplements have one of the strongest safety profiles in health care. When used as intended, serious adverse effects are far less common than with prescription drugs, making supplements a low-risk option for long-term wellness support.
- 1 Council for Responsible Nutrition, October 5, 2023
- 2 Res. J. Pharmacognosy and Phytochem. 2021; 13(2):101-102
- 3 Nutraceuticals World, September 16, 2024
- 4, 5, 6, 7, 8, 9, 10 Nutrition Industry Executive, December 1, 2025
- 11, 12, 13, 14, 15, 16, 17, 18, 19 Einfodemic, June 21, 2025
- 20, 21, 22, 23, 24, 25, 26, 27 RegASK, December 12, 2025
- 28, 30, 32, 34 American Botanical Council, 2013 (Archived)
- 29, 31 Cent Nerv Syst Agents Med Chem. 2010 Sep 1;10(3):238-46
- 33 Prog Neuropsychopharmacol Biol Psychiatry. 2008 Jul 1;32(5):1093-105
- 35, 36 Healthline, August 1, 2025
- 37 Alliance for Natural Health USA, October 15, 2015
- 38 New Hope Network, January 20, 2016 (Archived)
- 39 NutraIngredients, July 11, 2012
- 40 UPMC HealthBeat, May 26, 2025
- 41 CBC News, November 20, 2015
- 42 CBC News, January 21, 2016
- 43 U.S. Food and Drug Administration, October 1, 2024
- 44 Federal Trade Commission, December 20, 2022
Taking Melatonin Does Not Increase Your Risk of Heart Failure
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/12/19/melatonin-heart-failure-study-analysis.aspx
Analysis by Dr. Joseph Mercola December 19, 2025

Story at-a-glance
- A preliminary American Heart Association (AHA) study linked long-term melatonin use to increased heart failure risk, but a closer analysis shows serious flaws, including lack of peer review and failure to account for confounding variables
- The study found melatonin users had 90% higher heart failure rates, but data mixed together prescription-only countries with over-the-counter markets, misclassifying many actual users as non-users
- Moreover, the study failed to account for insomnia severity, psychiatric conditions, other medications, and dosing details, making it impossible to determine if melatonin caused the observed outcomes
- Decades of peer-reviewed research demonstrates melatonin’s cardioprotective effects, including reducing blood pressure, protecting heart tissue, and mitigating oxidative damage, contradicting the study’s alarming headlines
- While supplementation is unlikely to pose serious risks, there are natural ways to optimize your melatonin production, such as getting morning sunlight exposure, keeping a consistent sleep schedule, limiting evening blue light, eating earlier, and practicing stress-reduction techniques
Sleep deprivation among Americans is growing at a concerning rate. According to the latest data from the U.S. Centers for Disease Control and Prevention (CDC), 39% of adults aren’t getting enough sleep (around seven hours each day).1 Proper high-quality sleep is important because it allows your body to rest and repair, and having irregular sleep patterns increases your risk of a whopping 172 diseases.
In an effort to curb sleep deprivation, experts started recommending the public to take melatonin supplements. In fact, consumers have become so reliant on them that the industry for melatonin supplements was valued at $2.84 billion in 2024.2
Now, a preliminary study throws a wrench at the longstanding belief that taking melatonin supplements helps improve sleep quality. According to the findings, which were presented at the American Heart Association’s (AHA) Scientific Sessions 2025, long-term use of melatonin supplements was linked to an increased risk in heart failure.3 But is there any truth to this?
Does Melatonin Truly Increase Heart Risk?
According to these preliminary findings, adults with chronic insomnia who used melatonin for at least a year had worse long-term heart outcomes than those who never had melatonin listed anywhere in their medical records. However, there are problems with this research that need to be taken into account.
• How the researchers defined melatonin users vs. nonusers — The research team pulled five years of electronic health records from the TriNetX Global Research Network, covering 130,828 adults.4 The melatonin group included people whose medical charts documented at least 12 consecutive months of melatonin use. The control group had insomnia but no record of melatonin in their files. Patients with a history of heart failure or any recorded prescription for other sleep drugs were excluded.
• Why the initial results raised concern about heart failure risk — Adults with chronic insomnia who had documented long-term melatonin use showed about a 90% higher rate of new heart failure diagnoses over five years compared to nonusers (4.6% versus 2.7%).
A secondary analysis also suggested that long-term melatonin users were nearly 3.5 times more likely to be hospitalized for heart failure compared to insomnia patients who never had melatonin listed in their medical records (19.0% versus 6.6%). The study also noted an increased likelihood of death from any cause in the melatonin-recorded group compared with nonusers.
• What happened when the team used a stricter definition of long-term melatonin use — They also created a second definition of long-term use — people who had at least two melatonin prescriptions written 90 days apart. This detail matters because melatonin is only available by prescription in countries like the United Kingdom.
When the data was re-analyzed with this stricter definition, the increased risk persisted — this time with an 82% higher chance of developing heart failure over five years compared to the matched nonuser group.
• Why the dataset’s structure may have distorted the comparison — The dataset mixed countries where melatonin requires a prescription with countries, like the United States, where most people buy it over the counter (OTC). Because the research counted only people whose melatonin use appeared inside an electronic medical record, anyone using OTC melatonin in the U.S. automatically got classified as a nonuser.
If you think about it, the analysis creates a strange situation. Documented melatonin users in this dataset were officially sicker, more medicated, or more doctor-dependent than the average person who casually takes melatonin at home. This is where the cracks in the study begin to show.
• Key limitations that weaken confidence in the findings — They didn’t have access to insomnia severity, psychiatric conditions like depression or anxiety, alcohol intake, shift-work patterns, or use of other sleep-enhancing substances.
As lead author Dr. Ekenedilichukwu Nnadi explained, “Worse insomnia, depression/anxiety or the use of other sleep-enhancing medicines might be linked to both melatonin use and heart risk.”5 This means the melatonin users in the study may not have been harmed by melatonin at all — they may simply have been the sicker group at baseline.
• How hospital coding practices may have exaggerated heart failure numbers — The AHA press release noted that hospitalization codes often include a wide range of related heart-failure-like entries, which inflate hospitalization counts beyond true new heart failure episodes.
This means the 3.5-fold hospitalization increase mentioned earlier possibly reflects how hospitals enter codes, not how the heart responds to melatonin. When you’re trying to understand whether your supplement choices are safe, it’s important to dig deep into the data to discern the truth.
• What the study failed to report about melatonin dose and timing — Your melatonin experience depends heavily on dose and timing, but none of this was highlighted in the press release. A person taking 1 milligram (mg) occasionally at night is wildly different from someone taking 10 mg nightly for years, yet the database treated them as identical. This lack of detail leaves you without a clear picture of what level of use the associations reflect.
A Clearer Breakdown and Critique of the AHA Study
The press release by the AHA has grabbed the attention of many health advocates, most notably GreenMedInfo founder Sayer Ji. In a Substack post, Ji corrects the narrative created by media coverage of the AHA study.6
Ji investigates how headlines distorted the conference presentation and why this matters for consumers. Ultimately, he wants to highlight that the fear triggered by the AHA press release was the result of scientific misunderstanding — not evidence that melatonin damages the heart.
• Ji’s critique hinges on a single point — The AHA abstract was not a peer-reviewed study. He reiterates the AHA’s own words, saying “the findings are considered preliminary until published in a peer-reviewed journal.” However, mainstream media outlets treated the announcement as if it proved melatonin causes heart failure. Just look at the headlines he compiled in his Substack article:

This is an important distinction to make because preliminary abstracts are often incomplete, lack key variables, and serve as early scientific conversations, not final answers. Ji stresses that when journalists treat preliminary research as settled science, you are left with distorted health guidance.
• Mainstream media intentionally leaves out key details — Ji describes how numerous news platforms repeated the AHA’s claims verbatim, without any independent evaluation. He argues that this “media echo chamber” created widespread panic about a supplement with decades of research supporting its safety (shown later).
• Another key detail involves the way melatonin use was measured — Ji also pointed out how the AHA dataset only counted melatonin when it appeared as a prescription or documented medication in an electronic health record. It overlooks the fact that the majority of Americans buy melatonin over the counter, therefore making them invisible in the dataset.
This means the comparison between users and nonusers was fundamentally flawed — the so-called “nonuser” group almost certainly contained millions of real melatonin consumers whose use was unrecorded.
• Ji’s analysis also raises concerns about confounding variables — Specifically, he refers to factors that influence both insomnia and heart disease risk. He highlights that the AHA abstract excluded people taking benzodiazepines but did not adjust for other common sleep medications such as zolpidem (Ambien), eszopiclone (Lunesta), or trazodone. Ji notes that these drugs “carry well-documented cardiometabolic risks,” yet the abstract treated their use as irrelevant.
For anyone trying to understand whether melatonin itself is worrisome, this distinction matters. When a study fails to separate melatonin use from riskier sleep drugs, the results cannot tell you which factor caused the observed outcomes.
• Another overlooked layer involves other medications common in people with insomnia — Continuing the point above, Ji noted that the study did not account for the use of statins, selective serotonin reuptake inhibitors (SSRIs), or antihypertensives, even though all three drug classes influence cardiovascular pathology and sleep patterns.
This strengthens the argument that the data reflects the health status of medically complicated patients rather than the effects of melatonin. Once you realize this, the fearmongering generated by mainstream media makes far less sense.
• Ji brings evidence showing melatonin’s long-established cardioprotective effects — His article points to decades of peer-reviewed research demonstrating that melatonin provides three key benefits:
◦ Reduces blood pressure and improves endothelial function
◦ Protects mitochondria and heart tissue after ischemic injury
◦ Mitigates oxidative damage and inflammation across numerous organs
These points are essential. If melatonin had a track record of harming the heart, it would show up consistently in the scientific literature. Instead, we see the opposite.
• The AHA needs to be held accountable — Ji closes his critique with an argument that if the AHA wants to repair its reputation, they need to stop pushing unreviewed findings into the public without context. He emphasizes:7
“If the AHA wishes to reclaim credibility, it should insist that findings of this magnitude be fully peer-reviewed, transparently replicated, and contextualized within the broader body of evidence — rather than rushed into public consciousness as a fear-inducing soundbite.”

Save This Article for Later – Get the PDF Now
How to Address Your Melatonin Production Naturally
Ji’s arguments are sound. The AHA study is only observational — based on a deeply flawed data set — and does not show causation. Moreover, there’s plenty of evidence supporting the cardioprotective benefits of melatonin. Having said that, supplemental melatonin isn’t the ideal solution for sleeplessness as it does not address the root of the problem, which is a disrupted circadian rhythm.
If you’re having trouble sleeping properly, getting sun exposure at the right time of the day is the best way to optimize melatonin production and restore your body clock. Here are helpful recommendations to get you started:
1. Sun exposure triggers your mitochondria to make melatonin — Most of the melatonin in your body forms inside your mitochondria as part of your built-in antioxidant system. Direct sunlight on your skin — especially the near-infrared wavelengths that pass through tissue — activates the signals your cells rely on to produce mitochondrial melatonin.
Window glass blocks key wavelengths and sunscreen blocks UV, so inadequate sun exposure leaves your mitochondria without the cue they need to maintain this protective melatonin supply.
2. Calibrate your internal clock — Your body depends on early daylight to recalibrate its internal clock every morning. Make it part of your routine to go outdoors shortly after you wake up, ideally within the first hour. Aim for 10 to 15 minutes of direct sunlight each morning (skip the sunglasses during this time).
3. Stick to a steady sleep-wake routine — Try settling into a consistent pattern by going to bed and waking up around the same time daily, weekends included. If shifting your schedule feels tough, move your bedtime earlier in slow increments — about 15 minutes every few days — until it aligns with your natural rhythm. To help improve your overall sleep quality, read “Top 33 Tips to Optimize Your Sleep Routine.”
4. Minimize exposure to artificial light two hours before bedtime — Bright indoor lighting, especially blue-light from screens and light-emitting diodes (LEDs), signals your brain that it’s still daytime, shutting down melatonin production.
To support your nightly wind-down routine, dim your lights after sunset and keep screen time to a minimum as bedtime approaches. If you need to use a device, switch on night mode or wear blue-blocking glasses.
5. Align your eating pattern with daylight — Your metabolism follows daily, consistent rhythms tied to daylight, and irregular eating habits can disrupt your body clock. Try to have your main meals earlier in the day and finish dinner at least three hours before going to sleep.
6. Incorporate mindfulness practices — Your circadian rhythm is tightly linked to how your body handles stress. Techniques such as meditation, yoga, breathwork, or other mindful practices help calm the stress-response system, making it easier for your internal clock to stay in sync.
Frequently Asked Questions (FAQs) About the Connection Between Melatonin and Heart Failure
Q: Does long-term melatonin use actually increase the risk of heart failure?
A: In a preliminary study by the American Heart Association (AHA), researchers linked long-term melatonin use to a higher rate of heart failure diagnoses, hospitalizations, and all-cause mortality.
However, the data only tracked melatonin recorded in medical records. This means almost all over the counter melatonin users in the U.S. were labeled as “nonusers,” making the comparison deeply flawed. Researchers also lacked information about insomnia severity, psychiatric conditions, alcohol intake, other sleep drugs, or lifestyle factors — all of which directly influence heart risk.
Q: Why did the study show such alarming numbers if melatonin itself isn’t the problem?
A: The study’s “melatonin users” were not typical healthy supplement users. They were individuals whose melatonin use appeared in medical records, meaning they were sicker, more medicated, and more likely to be treated for complex conditions. This skewed the data, which reflected a high-risk population, not a harmful supplement.
Q: Did the mainstream media accurately report the AHA findings?
A: No. The press release clearly stated the data was “preliminary” and not peer-reviewed, but major news outlets reported it as definitive proof that melatonin causes heart failure. GreenMedInfo founder Sayer Ji highlighted that media outlets copied the AHA talking points without evaluating the study’s limitations. This created an echo chamber of fear-driven headlines despite the study’s weak design and major data gaps.
Q: What important details did the AHA study fail to include?
A: The dataset did not track melatonin dose or timing, so a person taking 1 mg occasionally was treated the same as someone taking 10 mg nightly for years. It also did not adjust for common sleep drugs (like Ambien, Lunesta, and trazodone), statins, SSRIs, or blood pressure medications — all of which influence heart function. Hospitalization counts were inflated due to broad diagnostic coding, further distorting results.
Q: Is melatonin actually harmful to the heart?
A: The broader scientific evidence does not support that conclusion. Decades of research show melatonin lowers blood pressure, protects mitochondria, reduces oxidative damage, improves endothelial function, and supports recovery after cardiac injury.
Aged Garlic Extract for Memory and Acute Stress Support — Here’s What the Research Says
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/12/19/aged-garlic-extract.aspx
Analysis by Dr. Joseph Mercola December 19, 2025

Story at-a-glance
- Aged garlic extract supports healthier memory pathways in aging brains by improving recognition learning and influencing hippocampal proteins tied to focus and recall
- Long-term intake of aged garlic extract lowered stress hormones in animal studies, helping the brain shift out of “high-alert mode” and into a calmer, more resilient state
- Key compounds like S-allyl-L-cysteine and FruArg reduce oxidative stress and inflammation, giving your neurons a cleaner, more efficient environment to function
- Aged garlic extract is easier to tolerate than raw garlic because the aging process transforms strong sulfur compounds into stable, bioavailable forms while increasing the compounds that support brain and stress health
- Aged garlic extract and aged black garlic extract are not the same, and are produced via different processes
Garlic has a long history as both food and medicine, and various cultures have relied on it for centuries as a remedy for fatigue, stress, and infections. Ancient medical systems used garlic to support strength and resilience — it’s been used to help ease digestive issues, arthritis, and even heart disease.1
Today, experts are looking beyond the usual raw, pungent bulb, and are exploring the benefits of aged garlic — a more biologically active form of this whole food that delivers diverse health advantages. Emerging research shows that aged garlic extract benefits memory and emotional regulation in aging adults, offering a promising multi-target approach to support cognitive resilience during the golden years.
Does Aged Garlic Extract Improve Memory?
Findings from a recent animal study published in Biomedical Reports, conducted by researchers at the University of Missouri, looked at whether consuming aged garlic extract (AGE) improved long-term brain and behavioral outcomes in the test subjects.2,3
• Raw garlic vs. aged garlic extract: What’s the difference? Before we go into the specifics of the study, it’s best to understand what sets aged garlic extract apart from the garlic you see in markets and groceries. While both offer antioxidant and anti-inflammatory advantages, aged garlic extract takes it a notch higher. This is because the valuable sulfur compounds in garlic like S-allyl-L-cysteine (SAC) are more abundant and bioavailable in aged garlic than raw garlic.
• How is aged garlic extract made? Basically, this extract is made through a slow aging process in an alcohol-water solution, which converts its nutrients into stable, water-soluble compounds. Aside from SAC, this also includes fructosyl arginine or FruArg (more on this later). Aged garlic extract is colorless, odorless, and does not have the pungent nature of raw garlic, making it easier to consume.
• Conducting the study — The featured study involved 48 male mice that were placed under controlled environmental conditions. Following a one-week acclimation period, they were randomly assigned to receive either a standard diet or the same diet supplemented with aged garlic extract. During the course of the 40-week study, their food intake and body weight were regularly monitored.
• Evaluating the subjects — After the feeding phase, the mice were shifted to a reverse light-dark cycle and subjected to tests that assessed their sensorimotor performance, exploratory activity, response to anxiety, social interaction, recognition memory, and spatial learning abilities. Afterward, 10 mice were humanely euthanized so the researchers could study their brain proteins.
• Results show aged garlic extract benefits the brain — The researchers found that the mice that received the aged garlic extract demonstrated better thinking and memory skills. In the novel object recognition test, these mice were better at telling the difference between familiar and new objects and spent more time exploring the new one. This suggests improvements in learning and memory.
In the Barnes maze, the mice that received the extract not only found the escape box, but when the maze was changed for the reversal learning part of the test, they also identified the new location faster, especially during the early training sessions.
• These results are promising, especially for those in their senior years — Cognitive decline and neurodegenerative disorders such as Alzheimer’s disease are now common among aging populations, and these challenges stem from age-related brain changes, including hippocampal shrinkage, oxidative stress driven by reactive oxygen species, and ongoing inflammation.
The rise of natural nutraceuticals like aged garlic extract offers hope for addressing age-related brain deterioration, helping support longevity in aging adults.
“[T]he present study revealed the neuroprotective effects of dietary supplementation of AGE in improving age-related cognitive decline and anxiety-like behaviors in aging mice.
Proteomic analysis highlighted the increase in synaptogenesis and reduction in apoptotic signaling, supporting the notion of AGE supplementation as a nutraceutical to mitigate age-related cognitive decline,” the authors concluded.4
Can Aged Garlic Extract Relieve Acute Stress or Anxiety?
In the featured study, the mice that ate aged garlic extract showed no differences in how much they ate, how much they weighed, their survival, or their overall health compared with mice that did not get the supplement. Their coordination and grip strength also stayed the same. However, they did show clear improvements in fear- and anxiety-related behaviors.
For example, in the light-dark test, the mice that received the extract entered the dark area less often and spent more time in the light area, suggesting they felt less anxious. A so-called emergence test showed similar effects. Mice given the supplement not only spent less time hiding, but also explored the space more and traveled a greater distance.
They were less likely to stay still, which is a sign that they were less fearful of new environments. Previous research has also shown the benefits of garlic extract for stress:5,6
• Aged garlic affects the acute stress response — Published in the Journal of the Chinese Medical Association, the team of researchers looked at how aged garlic extract, specifically a low-temperature aged form, influences the body’s acute stress response. The mice were divided into three groups — the first group was given raw garlic, the second was given low-temperature aged garlic (LTAG) extract and the third was the control group.
The mice in this study were exposed to an acute restraint test where they were briefly but firmly restrained to trigger stress-related hormonal and neurochemical changes. Afterward, the researchers measured the mice’s stress hormones, brain monoamines (like serotonin and dopamine), and antioxidant markers.
• Mice that received either LTAG or raw garlic extract had noticeably lower levels of stress hormones — In particular, they had significantly lower levels of corticotropin-releasing factor (CRF), corticosterone, and cortisol. By lowering these hormones, garlic extract appears to help blunt the body’s stress response through the hypothalamic-pituitary-adrenal (HPA axis), the central system controlling stress.
• Garlic extract also restored neurotransmitter balance and improved antioxidant markers — Acute stress usually depletes key neurotransmitters, which are essential for mood regulation and mental clarity, in the brain. Having low levels of these brain chemicals are associated with anxiety and depression. The researchers found that both raw garlic and LTAG restored these neurotransmitters to healthier levels, suggesting that this nutraceutical may have antidepressant-like effects.
Lastly, the researchers found that LTAG improved antioxidant enzyme expression and reduced oxidative markers. This means it helps protect the brain from stress-induced damage, enhancing resilience on a cellular level.
In an editorial commentary written by Shih-Jen Tsai, chairman of the Department of Psychiatry in Taipei Veterans General Hospital, he highlights the broader significance of these findings, stressing that future research needs to explore whether LTAG also influences brain-derived neurotrophic factor (BDNF).
“[T]he protein brain-derived neurotrophic factor (BDNF), one of the major neurotrophic factors in the brain, is a main contributor for the link between stress and depression. It would be of interest to test whether LTAG can restore decreased brain BDNF levels after restraint stress. Study also needs to test whether LTAG has similar stress relief effect as anxiolytics during stress test,” he writes.

Save This Article for Later – Get the PDF Now
How Does Aged Garlic Extract Work in the Brain?
As previously mentioned, the benefits of aged garlic extract for memory and brain health lie in its sulfur-containing compounds, discussed below. Although also found in raw garlic, the aging process transforms these nutrients and makes them more bioavailable, so your body puts them to better use.
• S-allyl-L-cysteine (SAC) — S-allyl cysteine is one of the most stable compounds created through the garlic-aging process. It supports antioxidant activity, reduces oxidative stress, and influences nitric oxide pathways that aid in healthy blood flow. The researchers have also highlighted its potential in improving heart health, saying:
“AGE and its active components, such as diallyl trisulfide and SAC, could offer cardioprotective effects, including reducing myocardial damage and supporting glyco- and lipo-metabolism.”7
• Fructosyl arginine (FruArg) — FruArg is a carbohydrate that forms in garlic via the Maillard reaction during the aging process. It plays a role in lowering inflammation and oxidative injury. According to the researchers, FruArg can cross the blood-brain barrier, further contributing to its brain health benefits. It also helps calm down inflammatory pathways inside the brain.
• Aged garlic affects brain regions and pathways involved in memory formation and learning — The hippocampus, in particular, is the region most consistently affected in the aged mice that received the extract. In the featured study, broader molecular shifts were observed in this area, including changes tied to synaptic plasticity and apoptosis regulation. If you have ever experienced brain fog, sluggish thinking, or trouble recalling information, the hippocampus is often involved.
The cortex showed additional pathway shifts, though less pronounced than the hippocampus. These predicted pathway adjustments included synaptogenesis and 14-3-3 signaling.
• The researchers also linked their findings to reductions in oxidative stress and neuroinflammation — When oxidative pressure increases, brain neurons lose their efficiency and resilience. Neuroinflammation interferes with synaptic communication, neurotransmitter balance, and mitochondrial energy production.
Aged garlic extract’s compounds counter these stressors. By helping regulate redox balance and inflammatory signaling, SAC and FruArg support healthier neuroplasticity — the brain’s ability to form, reorganize, and strengthen neural connections.
Aged Garlic Extract vs. Aged Black Garlic
Aged garlic extract and aged black garlic extract are often lumped into the same category, but there are certain distinctions between these two. Although they generally offer the same antioxidant and anti-inflammatory effects, they are produced differently.
• How aged black garlic extract is made — To produce the extract, whole bulbs are placed in a warm, humid environment for several weeks, which slowly caramelizes the natural sugars inside the cloves. This turns the garlic jet-black, soft, sweet, and almost jelly-like. The process resembles slow cooking more than true aging.
• Heating at these controlled temperatures triggers the Maillard reaction — This is the same chemical process that browns roasted foods. That reaction changes the flavor, texture, color, and chemical makeup of the garlic, creating unique compounds but also breaking down others.
• How aged garlic extract is made — As opposed to black garlic, aged garlic extract is not heated. Instead, it sits in a water-alcohol solution for months, transforming the strong compounds in raw garlic into more stable, gentle, and bioavailable molecules. This slow aging process produces consistently high levels of S-allyl cysteine and FruArg.
The alcohol-water extraction also removes the strong odor and reduces digestive irritation, which is why aged garlic extract is far easier to tolerate daily than raw garlic.
What Dose Has Been Studied and for How Long?
In the featured study, the researchers delivered aged garlic extract to the mice by incorporating it directly into their daily diet rather than administering a traditional mg/kg oral dose.
• Creating the supplemented diet — The researchers mixed 2 kilograms of a 40% AGE aqueous solution with 25.2 kilograms of standard rodent diet. This produced 26 kilograms of AGE-enriched chow. Because the AGE solution contained 0.8 kilograms of AGE on a dry-weight basis, the final diet provided approximately 3% AGE by dry weight.
The mixture was dried to a 5% moisture level for stability and the mice were allowed to consume as much as they wanted rather than receiving a fixed daily amount.
• Duration of the diet — Mice began receiving this aged garlic extract dosage at 43 weeks of age and continued on this regimen for 40 weeks, allowing the researchers to assess the long-term neurological and behavioral effects of chronic AGE supplementation.
Since the featured study was conducted on animal subjects, the human equivalence cannot be completely verified, as animal metabolism, absorption, and lifespan differ from that of humans. However, there are previous studies on garlic extracts that demonstrated safe doses for people.
• A 2022 study looked at the effects of aged black garlic extract on lowering blood pressure — In this double-blind, crossover, sustained and controlled intervention study, 67 participants all consumed 250 mg per day of a combination of SAC/AGE or a placebo for six weeks. They underwent a three-week washout period and continued for the next six weeks with the opposite intervention.8
If you decide to supplement with aged garlic extract or aged black garlic extract, it’s best to consult with your physician to confirm the safe dose for you. This is particularly important if you have any existing health condition, allergy, or are taking any medication.
Is Aged Garlic Extract Safe? Who Should Avoid It?
Safety is one of the main reasons aged garlic extract attracts so much interest. The aging process breaks down the harsh, irritating sulfur compounds found in raw garlic, which is why so many people tolerate aged preparations far better. You avoid that sharp burn in your stomach, the digestive unpredictability, and the unpleasant odor that sits on your breath after raw garlic. Still, garlic has its own set of cautions that you need to understand.
• Garlic naturally carries antiplatelet effects — This means it reduces the stickiness of your blood cells and makes your blood clot less quickly.9 This can be problematic if you’re taking anticoagulant medications or antiplatelet drugs, or if you have a history of bleeding disorders.
Taking AGE can cause your blood to thin even further, which increases your risk of bleeding more easily or more heavily than expected. If you fall into any of these groups, consult with your doctor before using aged garlic extract.
• If you are preparing for a medical or dental procedure, AGE may not be advisable — During surgery, you want your blood to clot normally to avoid unnecessary bleeding, and garlic’s antiplatelet action might interfere with that.
• Allergies are another area where caution is needed — If you are allergic to garlic or other plants in the Liliaceae family, like onions, leeks, or chives, then aged garlic extract may lead to side effects.10
Aged garlic extract offers you a rare combination of safety, biological potency, and real preclinical evidence that points toward healthier memory, steadier mood, and stronger resilience under stress. While human trials are still needed, these findings provide evidence that this extract has its advantages over raw garlic and even aged black garlic.
If you decide to explore aged garlic extract, treat it as a supportive tool rather than a cure, pay attention to the safety considerations, and work with a practitioner who understands your health history. This gives you the strongest foundation as the science continues to evolve.
Frequently Asked Questions (FAQs) About Aged Garlic Extract
Q: Does aged garlic extract improve memory?
A: In animal research, yes. Mice that consumed aged garlic extract for roughly 40 weeks showed better recognition memory and stronger learning behavior, according to a recent study published in Biomedical Reports. Their brains also showed molecular changes in regions tied to memory, including the hippocampus.
Q: Can AGE help with anxiety or acute stress?
A: Animal data suggest meaningful benefits. A study published in the Journal of the Chinese Medical Association reports that aged garlic preparations lowered stress-related hormones and restored neurotransmitter balance in mice exposed to acute restraint stress. These mice behaved less anxiously and recovered from stress more efficiently. However, no human clinical trials exist, so the real-world impact for you remains unknown until those studies are completed.
Q: How long would it take to see effects?
A: In the featured animal study, improvements in learning, memory, and anxiety-related behavior appeared after long-term intake. The mice consumed the extract for about forty weeks before researchers evaluated their behavior and brain proteins. Because human research has not been done yet, no reliable timeline exists for people. Your response would depend on future human trials.
Q: What’s the active compound?
A: S-allyl-L-cysteine, often shortened to SAC, is the most studied compound in aged garlic extract. It is water-soluble, stable, and predictable in the body, which makes it different from the harsh, inconsistent sulfur compounds in raw garlic. SAC plays a major role in antioxidant activity, nitric oxide-related blood flow support, and cellular protection.
FruArg, another compound formed during the aging process, helps quiet inflammatory pathways inside the brain. Together, they drive many of the effects discussed in the research.
Q: Is aged black garlic the same as AGE?
A: No. Aged black garlic and aged garlic extract are created through entirely different processes and contain different dominant compounds. Aged black garlic is heated for weeks until it turns black and sweet, while aged garlic extract undergoes a slow, controlled aging in water-alcohol that increases SAC and FruArg. Most of the research on memory, stress, and brain pathways involves aged garlic extract — not aged black garlic — so substituting one for the other gives you different outcomes.
Q: Is AGE safe with blood thinners or antidepressants?
A: Aged garlic extract has antiplatelet activity, meaning it reduces how quickly your blood clots. If you take anticoagulants, antiplatelet drugs, or have a bleeding disorder, you need to talk to your healthcare provider before using it. This is especially important before surgery, since altered clotting increases bleeding risk. Interaction data related to antidepressants specifically is limited, so professional oversight is necessary if you take psychiatric medication.
- 1 The Journal of Nutrition, March 2001, Volume 131, Issue 3, Pages 951S-954S
- 2, 4, 7 Biomed Rep. 2025 Oct 27;24(1):2
- 3 News-Medical.net, November 16, 2025
- 5, 6, 10 Journal of the Chinese Medical Association 82(9):p 677-678, September 2019
- 8 Nutrients, 2022, 14(3), 405
- 9 Journal of Chinese Clinical Medicine, January 2009, 4(5):288-294
L-Theanine Helps Calm Your Mind and Improve Focus Naturally
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/12/12/l-theanine-benefits.aspx
Analysis by Dr. Joseph Mercola December 12, 2025

Story at-a-glance
- L-theanine, an amino acid found in tea leaves, helps calm your mind without sedation by balancing neurotransmitters that regulate mood, focus, and sleep
- Studies show that taking 200 to 400 milligrams of L-theanine daily reduces stress, improves concentration, and promotes relaxation within 30 to 60 minutes of use
- Combining L-theanine with magnesium enhances both mental and physical relaxation, helping you fall asleep faster, stay asleep longer, and recover from stress more effectively
- Regular intake of L-theanine increases alpha brain wave activity, creating a state of calm alertness similar to meditation, while supporting steady energy and clear thinking
- Unlike caffeine or sedatives, L-theanine restores balance in your nervous system naturally, helping you manage anxiety, sharpen focus, and sleep more deeply without side effects
Few natural compounds are as well-known for their calming power as L-theanine, the amino acid found in tea leaves. For centuries, tea has been used to quiet the mind and sharpen awareness. Modern research explains why. L-theanine crosses your blood-brain barrier and directly influences neurotransmitters that control mood and focus.1 Unlike sedatives that dull alertness, L-theanine produces a calm, steady state by balancing your brain’s excitatory and inhibitory signals.
Green and black tea are the main sources of this compound, which works in harmony with your brain’s own rhythm, helping you stay alert without tension. Instead of dulling your senses, it fine-tunes them. Within less than an hour, most people notice a gentle shift — mental chatter slows, concentration sharpens, and your body relaxes without losing energy.
That’s why many people use it to manage anxiety, improve sleep, and stay focused under pressure. Understanding how this natural amino acid influences your brain helps explain why something as simple as a cup of tea restores calm in a chaotic world. In fact, researchers have mapped L-theanine’s pathways inside the brain, revealing why it’s so effective for relaxation and focus.
L-Theanine Rewires Your Brain’s Stress Response
A review published in Food Science and Human Wellness analyzed both animal and human trials to understand how L-theanine buffers anxiety and stress.2 Researchers examined its ability to influence neurotransmitters, your brain’s chemical messengers responsible for mood and emotional regulation. The goal was to explain why tea produces a distinct feeling of relaxation without sedation.
• Healthy adults and animal models both showed significant improvement in stress resilience — In human trials, doses between 200 and 400 milligrams (mg) daily reduced self-reported anxiety, blood pressure during mental tasks, and markers of physiological stress.
In rodent studies, L-theanine not only improved behavior linked to depression and anxiety but also normalized stress hormones controlled by the hypothalamic-pituitary-adrenal (HPA) axis, a major regulator of how your body reacts to stress.
• The benefits appeared within hours and built over time with consistent intake — Human participants experienced calmer alertness within 30 to 60 minutes after ingestion, matching the time it takes L-theanine to cross the blood-brain barrier.
Continued daily use sustained these effects, reducing long-term anxiety and improving overall mood balance. In rats, behavioral markers of depression improved after 21 days of supplementation, confirming both rapid and cumulative benefits.
• L-theanine increased alpha brain waves that promote calm alertness — Tests revealed higher alpha wave activity — brain patterns associated with relaxation and mental clarity — after subjects consumed L-theanine. These results mirror the peaceful focus people often describe after a few cups of tea. This physiological response explains why L-theanine is so effective for maintaining attention under stress without the jitteriness linked to caffeine.
• Neurotransmitter balance improved across several systems linked to mood — L-theanine increased levels of gamma-aminobutyric acid (GABA) and dopamine — key neurotransmitters that help stabilize mood and regulate sleep. It simultaneously decreased glutamate, the brain’s primary excitatory chemical that drives overstimulation.
Because its molecular structure resembles glutamate, L-theanine competes for the same receptor sites on neurons, preventing overactivation that causes tension or irritability. This dual action helps quiet racing thoughts while improving concentration.
• It also encourages your brain to grow new connections — The study described how L-theanine boosts neurogenesis — the formation of new neurons — in the hippocampus, a brain region that’s key for learning, memory, and mood. In animal models exposed to chronic stress, the compound restored brain cell growth and improved markers of resilience. This regeneration helps preserve mental flexibility and emotional balance, even under long-term strain.
L-Theanine Sharpens Focus and Lifts Mood Without Sedation
An article in The Hearty Soul reviewed several clinical studies on L-theanine’s effects on stress, mood, and concentration.3 Unlike prescription antianxiety drugs, which slow brain activity, L-theanine encourages a relaxed state while keeping you mentally sharp.
• Participants in clinical studies reported lower anxiety and better cognitive control — Adults who took 200 to 400 milligrams of L-theanine daily experienced an average 18% reduction in perceived stress and significant improvements in focus during demanding cognitive tasks.
Those struggling with racing thoughts or tension reported feeling “clear but relaxed” — a description that matched EEG data showing enhanced alpha wave activity. These brain waves are the same patterns seen during meditation and deep concentration, explaining why L-theanine feels balancing rather than sedating.
• Immune health improved in those under chronic stress — Health care workers taking daily L-theanine experienced fewer colds and flu-like symptoms compared to a placebo group.4 Stress weakens immune response by suppressing T-cell function, but L-theanine counteracts this by promoting more balanced immune activity. This means that staying calm isn’t just about mental health — it directly affects your body’s ability to fight illness.
• L-theanine improved attention span and accuracy in high-pressure situations — When tested in multitasking environments, subjects taking L-theanine showed faster reaction times and better accuracy than those given caffeine alone. In fact, pairing L-theanine with caffeine created a positive synergistic effect: focus improved without the anxiety spike common with energy drinks or strong coffee.5
• L-theanine helps you fall asleep faster and wake up feeling more refreshed — A 2025 review of 19 clinical trials with 897 people found that those who took L-theanine slept better, felt less groggy during the day, and reported higher overall sleep satisfaction.6 In other words, it helped people drift off more easily, sleep more soundly, and feel more alert in the morning — all without the side effects common with sleep medications.
L-Theanine and Magnesium Work Together to Quiet Your Mind and Restore Rest
Verywell Health summarized current findings from nutritional neuroscience, highlighting that combining L-theanine and magnesium amplifies their effects on stress, anxiety, and sleep.7 Magnesium supports more than 600 biochemical reactions in your body, including muscle relaxation and nerve transmission.8 Together, they address both the mental and physical sides of stress, giving your brain the signal to slow down and your body permission to rest.
• A clinically supported dosage range for L-theanine is 200 to 400 milligrams (mg) daily — This amount, taken for four to eight weeks, consistently reduces anxiety and stress without causing drowsiness. Each cup of green tea contains only 8 to 46 mg of L-theanine, so supplements are often used to reach therapeutic levels. Taking it during the day helps manage anxious thoughts, while nighttime use supports restful sleep.
• Magnesium complements L-theanine by calming your body’s stress response — When taken together, L-theanine and magnesium balance your brain’s excitatory and inhibitory systems — L-theanine relaxes your mind, and magnesium relaxes your body.
• Early evidence suggests a synergistic relationship — A 2022 animal study found that combining L-theanine and magnesium reduced the time it took to fall asleep and lengthened sleep duration more than either nutrient alone.9 Another small human study using a blend of L-theanine, magnesium, B vitamins, and rhodiola showed modest reductions in anxiety within two weeks.10
• L-theanine is well-tolerated and considered safe for daily use — The U.S. Food and Drug Administration classifies it as “generally recognized as safe,” and studies report minimal to no side effects at standard dosages.
Because it acts on GABA receptors, L-theanine enhances the calming effects of medications like benzodiazepines, so awareness of overlap is important. Magnesium is also safe within normal intake limits, and together, the two form a simple, low-risk strategy for easing anxiety naturally.
Simple Steps to Calm Your Mind and Strengthen Your Focus
Stress doesn’t just live in your head — it leaves fingerprints across your entire body. When your mind races, your muscles tense, your breathing quickens, and your sleep quality drops. The real solution isn’t to sedate yourself or drown your nerves in caffeine; it’s to rebalance how your brain and body communicate.
L-theanine and magnesium do exactly that. By regulating neurotransmitters, lowering cortisol, and improving brain wave patterns, they help restore equilibrium from the inside out. Here’s how you can start turning that science into everyday relief.
1. Start your day with tea — If your mornings feel chaotic, try swapping your usual coffee for a cup of matcha, green or black tea. Each cup provides a gentle dose of L-theanine that calms your nervous system while still allowing mental clarity. You’ll feel alert without the anxious buzz, and over time, your body’s stress response will grow steadier.
2. Add an L-theanine supplement when stress peaks — When you feel tension creeping in — before a presentation, after a long commute, or during an emotionally charged day — take 200 to 400 mg of L-theanine. This dosage helps lower anxiety and promote focus within an hour, helping your brain stay centered even under pressure.
3. Pair L-theanine with magnesium at night for deep rest — If racing thoughts keep you awake, combine L-theanine with magnesium about an hour before bed. Magnesium helps your muscles relax, while L-theanine quiets mental noise by stabilizing dopamine and GABA. Together they help you drift into restorative sleep and wake up clear-headed rather than groggy.
To find your ideal magnesium dose, start with magnesium citrate — it’s well absorbed but will trigger loose stools when you’ve taken too much. Slowly raise your dose until that happens, then back off slightly. That’s your personal threshold. Once you know it, switch to forms that give you the benefits without upsetting your digestion, like glycinate, malate, or L-threonate.
4. Train your body to respond calmly through breathing and timing — Your nervous system thrives on consistency. Try pairing your L-theanine or tea intake with slow, rhythmic breathing — four counts in, six counts out. This teaches your body to associate that supplement or ritual with calm focus. Over time, your brain learns to shift gears faster when you need composure.
5. Support your calm state with movement and light exposure — Your brain’s stress circuits respond to more than supplements — they’re shaped by daily rhythms. Step outside for morning sunlight and take short movement breaks throughout the day. Gentle activity such as stretching, walking, or yoga helps regulate cortisol and enhances the relaxing effects of L-theanine and magnesium.
This combination of natural light, motion, and mindful supplementation keeps your nervous system balanced and resilient.
When you give your brain the right inputs — nutrients, rest, and rhythm — it rewards you with balance. L-theanine and magnesium don’t just mask symptoms; they teach your body how to recover naturally, keeping your thoughts focused and your mood steady, even when life gets loud.
FAQs About L-Theanine
Q: What does L-theanine do for your brain and mood?
A: L-theanine promotes calm alertness by balancing neurotransmitters like GABA and dopamine — the same brain chemicals that influence mood, focus, and sleep. It lowers stress without causing drowsiness and helps you stay clear-headed under pressure.
Q: How much L-theanine should I take for anxiety or stress?
A: Many studies show benefits at doses between 200 and 400 mg per day for four to eight weeks. That’s the amount shown to reduce anxiety, improve focus, and support better sleep. For comparison, a cup of green tea provides roughly 8 to 46 mg, depending on the variety and brewing time.
Q: Can I take L-theanine and magnesium together?
A: Yes. Combining L-theanine and magnesium offers greater relaxation and sleep benefits than either alone. Magnesium relaxes your muscles and steadies your heartbeat, while L-theanine calms your mind and improves focus. Together, they help you manage stress, sleep deeply, and feel more balanced throughout the day.
Q: How long does it take to feel the effects of L-theanine?
A: You’ll typically notice a calmer, more focused state within 30 to 60 minutes of taking L-theanine. Its effects build with consistent use — daily intake via supplementation or tea strengthens stress resilience and supports long-term mood balance.
Q: Is L-theanine safe for everyday use?
A: Yes. The U.S. Food and Drug Administration classifies L-theanine as “generally recognized as safe.” It’s well tolerated at normal doses and doesn’t cause dependence or sedation. Most people find it a gentle, effective way to manage stress and improve focus naturally.
Cocoa Extract Supplement Reduces Key Marker of Inflammation and Aging, Study Finds
Reproduced from original article:https://articles.mercola.com/sites/articles/archive/2025/12/08/cocoa-extract-inflammation.aspx
Analysis by Dr. Joseph Mercola December 08, 2025

Story at-a-glance
- A new clinical analysis based on the COcoa Supplement and Multivitamin Outcomes Study (COSMOS) found that older adults taking a daily cocoa extract supplement saw an 8.4% annual drop in high-sensitivity C-reactive protein (hs-CRP), a key marker of chronic inflammation
- The supplement provided 500 milligrams of cocoa flavanols daily, including 80 milligrams of (-)-epicatechin, which is the same bioactive compound found naturally in cacao
- Researchers said this anti-inflammatory effect may help explain a 27% lower risk of cardiovascular mortality previously observed in the larger COSMOS trial
- Taking a cocoa flavanol supplement appears to support vascular and immune health by calming NF-κB signaling and improving endothelial function
- Unlike dark chocolate, standardized cocoa extract supplements are free of sugar and fat, delivering clinically studied doses in capsule form
Humanity’s connection to cacao runs deep — nearly 5,000 years deep. Long before it became the base for chocolate, cacao was revered in ancient civilizations as a “drink of the gods” and was worth more than gold.1
Today, modern science is circling back to what those early civilizations might have sensed all along: that cacao’s bitter heart carries more than flavor. It holds clues to how the body ages and heals.2
What Did the New Study Reveal About Cocoa Extract and Inflammation?
Chronic, low-grade inflammation accelerates conditions like heart disease, stroke, and diabetes. A major clinical trial called the COcoa Supplement and Multivitamin Outcomes Study (COSMOS) set out to answer a critical question: Does cocoa extract have any effects on the body’s inflammatory processes?3
• Study design and participants — Researchers from Mass General Brigham and Brigham and Women’s Hospital led a randomized, double-blind, placebo-controlled trial involving 598 adults with an average age of 70. For two years, participants received either a placebo or 500 mg of cocoa flavanols daily, including 80 mg of (−)-epicatechin, the compound believed to drive cocoa’s benefits.4
• Measured biomarkers and their roles — To understand how cocoa extract might influence inflammation and immune balance, researchers tracked five blood markers:5
◦ High-sensitivity C-reactive protein (hs-CRP) — Indicates the overall level of inflammation in the body. Elevated hs-CRP is strongly linked to heart disease and other chronic illnesses.6
◦ Interleukin-6 (IL-6) — A signaling molecule that promotes inflammation. Persistently high IL-6 levels are tied to arthritis, diabetes, and cardiovascular problems.7
◦ Tumor necrosis factor-alpha (TNF-α) — Another pro-inflammatory cytokine that can damage tissues when chronically elevated.
◦ Interleukin-10 (IL-10) — An anti-inflammatory cytokine that helps calm the immune response and prevent excessive inflammation.8
◦ Interferon-gamma (IFN-γ) — Regulates immune function and helps the body respond to infections; higher levels may reflect immune activation or modulation.
• Key findings of the study — Participants who took the cocoa extract supplement experienced an 8.4% annual reduction in hs-CRP compared with the placebo group. The other markers remained relatively stable overall, though interferon-gamma increased by about 6.8% per year, suggesting a subtle immune-modulating effect rather than broad suppression. Howard D. Sesso, ScD, MPH, one of the study authors, said:9
“Because of that, we wanted to see whether multi-year cocoa extract supplementation versus a placebo could modulate inflammaging — and the data suggests it does.”
• Broader cardiovascular link — The decrease in hs-CRP may help explain the 27% lower cardiovascular mortality previously observed in the full COSMOS trial. This connection supports the idea that cocoa flavanols could help lower long-term inflammation and improve heart health in older adults. Dr. Yanbin Dong, director of the Georgia Prevention Institute at the Medical College of Georgia and senior author of the study, said:10
“While cocoa extract is not a replacement for a healthy lifestyle, these results are encouraging and highlight its potential role in modulating inflammation as we age.”
• Why hs-CRP matters — High-sensitivity CRP is one of the most widely used tests for detecting silent, body-wide inflammation. Elevated levels can indicate a higher risk for heart disease even in people who appear healthy. A steady decline, like the one seen in this study, is considered a meaningful sign of reduced inflammatory stress.11
• Study takeaway — The findings suggest that standardized cocoa extract supplements, taken consistently over time, may help reduce key biological markers of inflammation linked to aging and cardiovascular disease. While not a replacement for healthy habits, cocoa flavanol capsules may offer an added layer of nutritional support for heart and immune health.12
Cocoa Extract vs. Dark Chocolate
Chocolate has long had a “healthy indulgence” reputation, but when it comes to science, not all cocoa products are created equal. The benefits seen in studies don’t come from candy bars — they come from standardized cocoa extract supplements, which deliver precise doses of active compounds without added sugar or fat.13
In the COSMOS study, participants took a daily 500 mg cocoa flavanol supplement. To match that dose through dark chocolate alone, you’d need to eat multiple bars a day. Here’s how the two compare:14
| Factor | Cocoa extract (standardized) | Dark chocolate |
|---|---|---|
| Flavanols | Standardized 500 mg/day (including 80 mg epicatechin)15 | Varies widely; often unlisted and degraded by processing |
| Calories per “serving” used in studies | Negligible | ~170 calories per 1 oz (28 g)16 |
| Sugar content | None | ~6.8 g per 1 oz17 |
| Standardization | Consistent and clinically tested | Inconsistent; it depends on the bean source and manufacturing |
| Practicality for study dose | Easy to achieve through daily capsules | Impractical; requires multiple ounces daily |
| Health focus | Anti-inflammatory and heart health benefits supported by trial data | Primarily sensory and comfort-based |
“This study calls for more attention to the advantage of plant-based foods for cardiovascular health, including cocoa products rich in flavanols … It reinforces the importance of a diverse, colorful, plant-based diet — especially in the context of inflammation,” said Sesso.18
So, while dark chocolate can still have a place as a mindful treat, it’s not a reliable way to reproduce the results seen in the COSMOS trial. The difference comes down to dose, consistency, and purity. Cocoa extract offers a concentrated form of what makes chocolate healthy.

Save This Article for Later – Get the PDF Now
How Do Cocoa Flavanols Help Reduce ‘Inflammaging’?
“Inflammaging” describes the slow, low-grade inflammation that builds up as we age, often silently, and contributes to heart disease, diabetes, cognitive decline, and other chronic conditions. Scientists are now studying how plant nutrients like cocoa flavanols might help ease this process.19
• What cocoa flavanols are — Cocoa flavanols are naturally occurring compounds in the cocoa bean, with (−)-epicatechin being one of the most studied. Known for their antioxidant potential, these flavanols also influence cell signaling, which is the biochemical “switches” that control inflammation and blood vessel health.20
• Supporting endothelial function — The endothelium, the thin lining inside your blood vessels, plays a vital role in circulation and inflammation control. With age, these cells lose efficiency, leading to stiffer arteries and higher cardiovascular risk. Flavanols boost nitric oxide availability, helping blood vessels relax, improving oxygen delivery, and reducing oxidative stress.21
• The NF-κB connection — NF-κB is a protein complex that regulates immune response and inflammation. When overactivated, it triggers inflammatory cytokines that accelerate tissue damage and aging. Cocoa flavanols appear to help modulate these inflammatory pathways, reducing oxidative stress and supporting immune balance.22
• A gradual, long-term effect — These benefits emerged slowly over two years, underscoring that cocoa extract is not a quick fix but a steady support for long-term resilience. Like inflammaging itself, the shift happens quietly — and consistency matters more than immediacy.23
How to Choose a Safe, Effective Cocoa Flavanol Supplement
Cocoa flavanol supplements, often labeled as cocoa extract, can differ dramatically in purity, potency, and effectiveness. While some align with clinical-grade research formulas, many don’t. This checklist guides you in identifying trustworthy products and avoiding misleading marketing or unsafe blends.
1. Look for standardized flavanol content — Choose products that list “Cocoa flavanols: ≥500 mg per serving” and, ideally, “(−)-epicatechin: ~80 mg.” Avoid any label that just says “cocoa extract” without showing the flavanol amount — that’s your most enormous red flag.
2. Check for standardization and transparency — Look for phrases like “standardized to X% cocoa flavanols” or a QR code linking to a Certificate of Analysis (COA). Brands that verify purity and potency are more trustworthy than those relying on proprietary blends or vague claims.
3. Confirm the serving math — Doses can be misleading. Check whether the listed amount is per capsule or per day. Some brands require two or more capsules to reach the 500 mg daily benchmark.24
4. Third-party testing matters — Choose supplements that display seals from the United States Pharmacopeia (USP) or NSF International, two independent organizations that set strict standards for supplement quality, purity, and safety. These certifications confirm that the product contains what the label claims, is free from harmful contaminants, and meets rigorous manufacturing standards.
If a brand publishes a Certificate of Analysis (COA) from an accredited lab, that’s another strong sign of transparency.25
5. Check for heavy metals — Cocoa plants can absorb cadmium and lead from soil, which can accumulate in cocoa products. Look for brands that test every batch and meet safety standards like California Proposition 65 and USP limits. Prop 65 requires warnings for chemicals linked to cancer or reproductive harm, while USP sets strict daily exposure limits for heavy metals (e.g., cadmium and lead) in supplements.26
6. Pay attention to stimulant content — Cocoa naturally contains small amounts of caffeine (0 to 15 mg) and theobromine (40 to 60 mg) per serving. These compounds can affect heart rate and alertness, especially if you’re sensitive or already consume other stimulants. If this concerns you, look for “decaffeinated” or “caffeine-controlled” formulas that show exact levels on the label.27
7. Cocoa extract pills vs. powder — Powders marketed as “cocoa wellness drinks” often include sugar, flavoring, or fillers that dilute flavanol content. These additives can undermine the health benefits you’re looking for. To maximize health benefits, experts recommend choosing standardized cocoa extract supplements rather than sweetened powders or mixes.28
8. Ignore vague buzzwords — Phrases like “pure cacao,” “natural chocolate extract,” or “superfood blend” sound appealing but reveal nothing about potency. Always look for specific flavanol and epicatechin values, which indicate the product aligns with clinical research standards.29
|
TL;DR — 8 fast checks for cocoa extract supplements |
|
If you want to read more about the benefits of cacao, check out my article, “Dark Chocolate Reduces Stress and Inflammation, Boosts Memory.”
Demystifying Cocoa Extract Labels
Supplement labels can look scientific but still leave out the most essential details. Understanding what the terms mean can help you avoid weak formulas, filler-heavy blends, or unsafe products. The table below summarizes what to look for when comparing cocoa extract supplements:
| Label section | What to look for | Why It matters |
|---|---|---|
| Serving size | 1 capsule, one scoop, etc. | Serving size tells you how much you’re taking. It helps you avoid overdosing and track your daily intake easily. |
| Flavanol content | 500 – 1,000 mg per serving (optimal range) | The flavanol amount is what delivers the benefits. Too little won’t help, and too much can cause side effects.30 |
| Purity | % flavanols (e.g., ≥4% or ≥7.5%) and lab verification | Purity guarantees you’re getting active compounds, not just cocoa filler. Lab testing adds trust and transparency.31 |
| Additional ingredients | Minimal fillers, no artificial additives | Fewer additives mean fewer allergens or unnecessary chemicals.32 |
| Health claims | FDA-qualified claim (with disclaimer) | Real claims show compliance with regulations. If it sounds too good to be true, it probably is.33 |
| Certifications | Organic, Non-GMO, Third-Party Tested | Certifications signal higher quality and independent checks for safety and potency. |
Using Cocoa Extract Supplements with Caution
Cocoa extract supplements are generally considered safe for most healthy adults when used at studied doses (around 500 mg cocoa flavanols per day). Still, like any bioactive compound, they aren’t for everyone. Here are some handy things to know:
• Start with a lower dose — If you’re new to cocoa extract or sensitive to caffeine, ease in with half the recommended amount. It’s like testing the waters before diving in — your body gets time to adjust, and you avoid feeling jittery or uncomfortable.34• Cocoa extract side effects — Ever taken a supplement on an empty stomach and felt queasy? Cocoa extract can do that too. Pairing it with a meal makes the experience smoother and helps your body absorb those beneficial flavanols more effectively.35
• Skip the stimulants — Cocoa naturally contains caffeine and theobromine, so taking it with energy drinks or other stimulant supplements will make you feel wired or restless.36
• Double-check your meds — If you’re on blood thinners, blood pressure meds, or stimulants, cocoa’s natural compounds can amplify their effects. A quick chat with your clinician can save you from dizziness or other surprises.
What science is now discovering about cocoa’s more profound benefits only adds another layer to what we already love about it. Used wisely, cocoa extract supplements can complement a healthy lifestyle, not replace it. Think of them as gentle, long-game support for heart and brain health — best used consistently and with mindfulness.
Frequently Asked Questions (FAQs) About Cocoa Extract Supplements
Q: Does a cocoa extract supplement reduce hs-CRP?
A: Yes. In older adults, two years of daily cocoa extract supplementation lowered high-sensitivity C-reactive protein (hs-CRP) by about 8.4% per year compared with placebo. hs-CRP is a blood marker linked to chronic, low-grade inflammation that contributes to cardiovascular and age-related disease. The finding suggests cocoa flavanols may help calm underlying inflammation associated with aging.
Q: What dose of cocoa flavanols was used in the study?
A: Participants took 500 milligrams of cocoa flavanols daily, including 80 milligrams of the bioactive compound (−)-epicatechin, for two years. This standardized dose, used in the COSMOS trial, was shown to reduce hs-CRP levels while maintaining consistency across participants safely.
Q: Is a cocoa supplement better than dark chocolate for inflammation?
A: For matching the studied flavanol dose, the results are positive. Cocoa extract capsules are standardized for purity and potency, while dark chocolate varies widely depending on processing. Most chocolate products also include added sugar and fat, which dilute the benefits. Supplements offer a precise, calorie-free way to support inflammation balance without the extras.
Q: Who should avoid cocoa extract?
A: People who are sensitive to caffeine or theobromine are advised to approach cocoa extract supplementation carefully. Individuals taking blood thinners or blood pressure medications are also recommended to seek medical guidance before using these products to avoid interactions.
Q: How long until I might see results?
A: In the study, results build gradually. Researchers tracked participants over one and two years and saw consistent, year-over-year reductions in hs-CRP, rather than rapid changes. This suggests cocoa extract supports inflammation management over time when taken consistently as part of a healthy lifestyle.
Q: Can cocoa extract support heart health in older adults?
A: Emerging research suggests it may. The COSMOS trial found that participants taking cocoa extract experienced a 27% lower rate of cardiovascular mortality compared to those taking a placebo.
Q: Are there side effects of cocoa flavanol capsules?
A: Cocoa flavanol supplements are generally well tolerated, but mild side effects such as restlessness, insomnia, or stomach upset can occur in sensitive individuals. The caffeine and theobromine content may cause jitteriness if combined with other stimulants. As with any supplement, it’s best to start slowly, follow dosage guidelines, and talk to a healthcare provider before use.
- 1 The Good Chocolate, May 22, 2024
- 2, 7, 13, 19 Medical News Today, September 21, 2025
- 3, 4, 5, 8, 12, 14, 15, 34 Age Ageing, 2025;54(9):afaf269
- 6, 9, 11, 24 Medical Xpress, September 17, 2025
- 10, 18, 23 Mass General Brigham, September 17, 2025
- 16, 17 MyFoodData, Dark Chocolate (70-85% Cocoa)
- 20 Medical News Today, July 21, 2023
- 21 EMJ, September 23, 2025
- 22 Nutrients, 2016;8(4):212
- 25 Supernatural Man’s Vitality Blog, February 26, 2025
- 26 Medical News Today, July 31, 2024
- 27 Medical News Today, December 18, 2015
- 28 VitaLibrary, August 9, 2025
- 29, 36 Medical News Today, October 25, 2023
- 30 The Organic Cacao, September 3, 2025
- 31 Chocolat Madagascar, February 26, 2024
- 32 The Straight, November 2, 2025
- 33 Double Wood Supplements, August 4, 2025
- 35 Medical News Today, July 5, 2024
Niacinamide Found to Reduce the Risk of New Skin Cancers
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/11/22/niacinamide-reduce-skin-cancer-risk.aspx
Analysis by Dr. Joseph Mercola November 22, 2025

Story at-a-glance
- Skin cancer affects one in five Americans, with nonmelanoma types like basal and squamous cell carcinoma making up most cases. Niacinamide, a form of vitamin B3, is found to offer a strong preventive effect
- A recent study published in JAMA Dermatology associated niacinamide use with a 14% lower overall risk of developing additional nonmelanoma skin cancers, with the greatest benefit seen after the first cancer diagnosis
- Earlier research showed that taking 500 milligrams of niacinamide twice daily reduced new nonmelanoma skin cancers by 23% and precancerous lesions by up to 15%
- Niacinamide protects your skin by restoring NAD+ for DNA repair, reducing inflammation, supporting immune defenses, and strengthening the barrier that maintains moisture and resilience against environmental stress
- For long-term use, smaller daily doses of 50 milligrams three times per day are safe and sustainable. Combining niacinamide with sensible sun exposure habits and good nutrition strengthens skin defense naturally
Skin cancer is one of the most common cancers worldwide.1 In the United States, one in five Americans is expected to develop skin cancer during their lifetime, and roughly 9,500 people receive a diagnosis each day.2 The vast majority of these cases are nonmelanoma skin cancers, which include basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).3
The incidence of nonmelanoma skin cancers is estimated to be 18 to 20 times higher than that of melanoma.4 Although often treatable when detected early, recurrence is common and remains a significant concern.5 This has led researchers to explore better ways to prevent future cases, and one compound that has been recommended by dermatologists is niacinamide, a form of vitamin B3.6
What Is Niacinamide and How Does It Protect Your Skin?
Niacinamide is one of the two main forms of vitamin B3. The other is niacin, or nicotinic acid, which is known for causing flushing due to histamine release. Niacinamide does not produce this effect, which makes it easier to tolerate and suitable for long-term use. It used to be called nicotinamide, but the term niacinamide is now preferred to prevent confusion with nicotine, an entirely unrelated compound.
• Niacinamide supports the skin at the cellular level — It does this by restoring a vital molecule called nicotinamide adenine dinucleotide (NAD+), a coenzyme that every cell relies on for energy production, DNA repair, inflammation control, and mitochondrial health.
When prolonged UV exposure, oxidative stress, or aging depletes NAD+ levels, skin cells lose the energy needed to maintain normal repair processes. Niacinamide replenishes this supply, keeping your skin’s repair systems active and resilient.
• Inside your cells, niacinamide participates in the NAD+ salvage pathway — When NAD+ breaks down during normal metabolic activity, it forms niacinamide, which the body recycles by converting it into nicotinamide mononucleotide (NMN) and then back into NAD+. This cycle allows your cells to sustain energy production and DNA repair without interruption, ensuring that repair enzymes and antioxidant systems always have the resources they need.
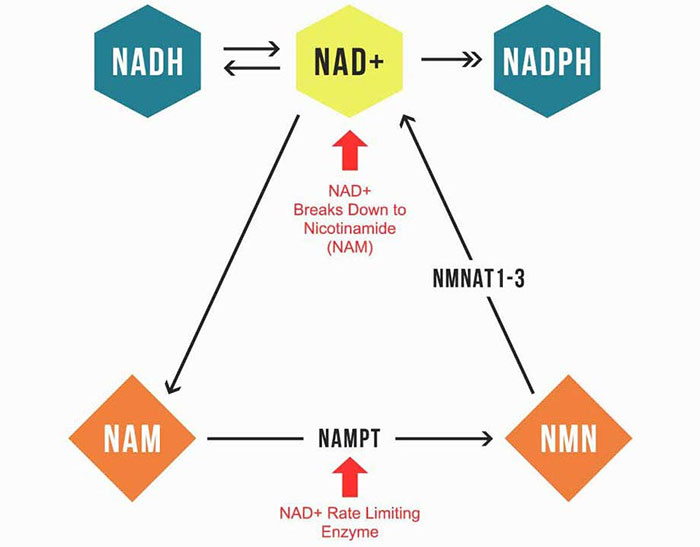
• NAD+ fuels key DNA-repair enzymes — These include poly (ADP-ribose) polymerase (PARPs) and sirtuins, which identify and repair DNA strand breaks. When NAD+ levels drop, these enzymes cannot function effectively, leading to the accumulation of damaged DNA. By maintaining NAD+ availability, niacinamide keeps these enzymes working efficiently and supports the genetic stability of your skin cells.
• Niacinamide also reinforces your skin’s structural defenses — It stimulates ceramide production, strengthening the barrier that locks in moisture and shields against environmental damage.7 Because of its effects, dermatologists have used niacinamide for decades in both topical and oral forms to manage acne, rosacea, hyperpigmentation, and photoaging.8
• Niacinamide’s influence extends far beyond skin health — Clinical studies have shown benefits in conditions linked to metabolic stress, inflammation, and mitochondrial dysfunction, including neurodegeneration,9 glaucoma,10 chronic pain,11 stress,12 and even oxidative damage linked to excessive linoleic acid (LA) intake.
To learn more about how niacinamide supports not only skin health but also your body’s broader resilience, read “The Wide-Ranging Health Benefits of Niacinamide.”
New Evidence Strengthens Niacinamide’s Role in Skin Cancer Prevention
The evidence confirming niacinamide’s protective role against skin cancer has been limited because its over-the-counter availability means most use goes unrecorded in medical databases. This is why researchers conducted a large-scale retrospective cohort study published in JAMA Dermatology, drawing on data from the Veterans Affairs (VA) Corporate Data Warehouse to examine whether niacinamide use led to a reduced risk of new skin cancers.13
• How the study was designed — The research team analyzed data from 33,822 veterans between 1999 and 2024. They identified patients who had filled prescriptions for 500 milligrams (mg) of oral nicotinamide twice daily for more than 30 days and compared them with matched controls who had not received the supplement.
In total, 12,287 niacinamide users were matched with 21,479 nonusers based on factors including age, sex, prior skin cancer history, and use of other dermatologic treatments. The primary outcome was time to the next diagnosis of BCC or cutaneous SCC (cSCC).
• Niacinamide use lowered overall skin cancer risk — Across the full study population, niacinamide use was associated with a 14% lower overall risk of developing skin cancer. The benefit was most pronounced when supplementation began after the first skin cancer diagnosis, producing a 54% reduction in new cases.
However, this preventive effect diminished when treatment was started after multiple prior cancers. Both BCC and cSCC incidence decreased, with the strongest risk reduction seen in cSCC.
• Findings in immunocompromised patients — The study also evaluated a subgroup of 1,334 patients who were immunocompromised due to organ transplants. Among these transplant recipients, no overall significant reduction in cancer risk was observed. However, early use of niacinamide after the first cancer diagnosis was linked to fewer cases of cSCC, underscoring the importance of timing in its effectiveness.
• Early use of niacinamide may redefine preventive skin cancer care — According to the study’s lead author, Dr. Lee Wheless, assistant professor of Dermatology and Medicine at Vanderbilt University Medical Center and a staff physician at VA Tennessee Valley Healthcare System:
“There are no guidelines for when to start treatment with nicotinamide for skin cancer prevention in the general population. These results would really shift our practice from starting it once patients have developed numerous skin cancers to starting it earlier. We still need to do a better job of identifying who will actually benefit, as roughly only half of patients will develop multiple skin cancers.”14
This real-world analysis builds on earlier randomized trials by confirming that niacinamide is associated with lower nonmelanoma skin cancer risk in a large, diverse population.

Save This Article for Later – Get the PDF Now
The First Clinical Evidence of Niacinamide’s Protective Effect
The protective role of niacinamide in skin cancer prevention was first confirmed in a controlled human trial published in The New England Journal of Medicine in 2015.15 The study, known as the Oral Nicotinamide to Reduce Actinic Cancer (ONTRAC) trial and conducted by researchers at the University of Sydney, showed that a simple oral supplement could lower the recurrence of common skin cancers in high-risk patients.16,17
• Study design and participants — The ONTRAC trial included 386 adults aged 30 to 91 years who had developed two or more nonmelanoma skin cancers in the past five years. Participants were randomly assigned to receive nicotinamide, 500 mg twice daily, or placebo for 12 months, with dermatologic evaluations every three months.
• What the results showed — After one year of supplementation, participants taking nicotinamide had 23% fewer new basal and squamous cell carcinomas than those taking placebo. The supplement also reduced actinic keratoses, precancerous lesions that signal future cancer risk, by 11% after three months and 15% after 12 months.
• Safety confirmed across all groups — Niacinamide was well tolerated, with no meaningful side effects. Unlike niacin, it did not cause flushing, headaches, or increased blood pressure, and no participants discontinued treatment due to adverse effects. Its clean safety profile made it an ideal option for older adults or those on multiple medications.
• Why the findings matter for high-risk patients — Lead investigator Diona Damian, MBBS, Ph.D., described niacinamide as “a new opportunity for skin cancer prevention,” noting that it is safe, inexpensive, and immediately accessible for those at greatest risk of recurrence.18
Supporting this view, Dr. Peter Paul Yu, the president of the American Society of Clinical Oncology at the time, called the results “a remarkably simple and inexpensive way to help people avoid repeat diagnoses of some of the most common skin cancers.”19
This trial established the foundation for research on niacinamide and skin cancer prevention. A survey conducted in 2021 found that nearly 77% of dermatologists who perform skin cancer surgery now recommend oral niacinamide to prevent skin cancers.20 Learn more about niacinamide’s protective role in “Niacinamide — The Best Supplement to Prevent Skin Cancer.”
How to Take Niacinamide Supplement
While clinical studies have shown that high doses can deliver therapeutic results in targeted treatments, those levels are not intended for routine use. For ongoing health and cellular support, smaller amounts taken regularly are safer and sustainable.
• Take small, evenly spaced doses throughout the day — For optimal health, I recommend taking 50 milligrams of niacinamide three times per day. You can also take it four times a day if you space out the dose evenly. Take a dose as soon as you get up, another before going to bed, and two more evenly spaced between those times.
• Higher doses can cause adverse effects — The problem with taking too much vitamin B3, whether in the form of niacin or niacinamide, is that it might backfire and contribute to cardiovascular disease and other side effects. Other potential side effects of high doses include nausea, vomiting, headache, dizziness, and fatigue.
• Make sure you’re getting all the other B vitamins — Your body relies on the full spectrum of B vitamins to maintain optimal health, especially regular niacin, riboflavin (B2), folate (B9), and pyridoxine (B6).
Vitamin B3 is found in grass fed beef, liver, wild-caught Alaskan salmon, and bananas,21 while vitamin B6 is abundant in grass fed beef, potatoes, and bananas.22 As for folate, you can obtain it in spinach, broccoli, and asparagus.23 Meanwhile, vitamin B12-rich foods include grass fed beef liver, wild rainbow trout, and wild sockeye salmon.24
5 Additional Strategies to Protect Your Skin Health
While niacinamide plays a key role in maintaining healthy skin, it works best as part of a broader foundation. Your daily lifestyle choices shape how your skin repairs, regenerates, and defends itself. The following strategies complement niacinamide’s protective effects and help lower your risk of skin cancer while supporting long-term skin vitality:
1. Optimize your vitamin D levels — Vitamin D activates receptors that regulate how your cells grow, repair, and communicate, helping reduce the risk of cancer by reducing DNA damage, improving immune surveillance, and promoting normal cell differentiation.25
A study from the University of Eastern Finland found that individuals who took vitamin D regularly had nearly 50% lower melanoma risk, even among those with high-risk skin types.26 Maintaining vitamin D levels in the 60 to 80 ng/mL (150 to 200 nmol/L) range provides the strongest protection.
While many studies discourage sun exposure, sunlight is your body’s primary and most efficient source of vitamin D. The key is to enjoy sunlight in a way that protects your skin from burning. Simple steps taken before and during sun exposure can make all the difference. For practical guidance on how to do this safely, read “Having Optimal Vitamin D Levels Helps Lower Your Risk of Melanoma.”
2. Nourish your skin from the inside out — Foods rich in antioxidants are especially valuable because they neutralize damaging free radicals. Prioritize carotenoid-rich fruits and vegetables such as carrots, sweet potatoes, tomatoes, and leafy greens. These pigments accumulate in your skin, where they act as a natural shield against oxidative damage.27
Equally important are vitamins C and E, which work together to preserve skin integrity. Vitamin C fuels collagen synthesis, accelerates tissue repair, and maintains the connective structure that keeps your skin firm and resilient.28 Good sources include bell peppers, citrus fruits, strawberries, and broccoli.29
Vitamin E shields cell membranes from lipid peroxidation, a reaction that weakens your skin’s lipid barrier and speeds visible aging.30 Pasture-raised eggs, grass fed beef liver, wild-caught fish, and leafy greens provide abundant amounts of this vitamin.
3. Improve sleep and circadian rhythm to boost skin repair — Your skin follows a daily rhythm of repair and renewal that peaks during sleep. Research shows that chronic circadian disruption not only weakens the skin barrier but also increases the risk of tumor formation by impairing clock genes that regulate cell division and DNA stability.31
Aim to get adequate, high-quality sleep nightly by creating a consistent bedtime routine, limiting blue light exposure in the evening, and getting natural sunlight in the morning to help reset your circadian rhythm. Keeping your room cool, dark, and quiet also supports deeper rest, allowing your skin the time it needs to repair and renew overnight.
4. Engage in regular physical activity — A study on melanoma shows that regular physical activity can slow tumor growth and enhance immune surveillance. Researchers also found that exercise boosts the activity of natural killer cells, improves blood flow to skin tissues, and reduces inflammatory signaling linked to tumor progression.32
You don’t need strenuous workouts to gain the benefits. Regular, moderate movements such as walking, stretching, or light resistance exercise will do. Consistent activity also helps balance blood sugar and hormones, which play a direct role in maintaining healthy and resilient skin.33
5. Be wise when it comes to sunscreen — Dermatologists often recommend daily sunscreen use to lower skin cancer risk, but many products on the market contain chemicals that can harm your health and the environment, including oxybenzone, octinoxate, homosalate, and octocrylene.34
If you choose to use a sunscreen, look for zinc oxide or titanium dioxide instead and make sure they’re not nano-sized. Lotions or creams with zinc oxide offer the most stable and broad UVA and UVB protection, while titanium dioxide is a good alternative.
Avoid high-SPF products above 50, which often create a false sense of security and don’t provide significantly better protection. SPF measures UVB defense only, not UVA, which causes the most skin damage and aging. Ultimately, sunscreen should not be your first line of defense. The healthiest approach is safe, sensible sun exposure.
Frequently Asked Questions (FAQs) About Niacinamide and Skin Cancer
Q: What is niacinamide?
A: Niacinamide is a form of vitamin B3 that supports your skin by restoring NAD+, which drives energy production and DNA repair, reducing inflammation, enhancing immune defenses, and strengthening the skin barrier by supporting ceramide production.
Q: Is niacinamide the same thing as niacin?
A: No. Niacinamide (also called nicotinamide) and niacin (nicotinic acid) are two different forms of vitamin B3. Niacin causes flushing due to histamine release, while niacinamide does not. However, excessive intake of either form can contribute to cardiovascular problems.
Q: How much niacinamide should I take for daily support?
A: Smaller doses of 50 milligrams (mg) taken three times per day are ideal for long-term use. Clinical trials that targeted skin cancer prevention used 500 mg twice daily, but that dose was studied in high-risk patients with previous skin cancers.
Q: Can I just get niacinamide from food?
A: You can get some niacinamide from foods naturally high in vitamin B3, including grass fed beef, liver, mushrooms, poultry, and salmon. You may also opt to take supplements to ensure steady support for your skin’s repair and protection processes.
Q: Does niacinamide help with other skin problems?
A: Yes. Dermatologists use niacinamide to manage acne, rosacea, uneven pigmentation, and signs of photoaging. Its anti-inflammatory, antioxidant, and barrier-strengthening effects make it a versatile nutrient for maintaining overall skin balance and resilience.
– Sources and References
- 1, 3, 4 Cancer Pathogenesis and Therapy Volume 3, Issue 2, March 2025, Pages 89-100
- 2 American Academy of Dermatology Association, Skin Cancer
- 5 Biomedicines. 2018 Jan 2;6(1):6
- 6, 14 Medical Xpress, September 18, 2025
- 7 Br J Dermatol. 2000 Sep;143(3):524-31
- 8 YouTube, Dr. Dray, The Skin Supplement You Need to Know About April 28, 2022
- 9 Clinical Trials Nicotinamide as an Early Alzheimer’s Disease Treatment (NEAT) NCT03061474
- 10 JAMA Ophthalmology 2022;140(1):11-18
- 11 Cell Reports Medicine November 8, 2023
- 12 Nutrients. 2022 Jun; 14(11): 2219
- 13 JAMA Dermatol. Published online September 17, 2025. doi: 10.1001/jamadermatol.2025.3238
- 15, 16 N Engl J Med. 2015 Oct 22;373(17):1618-26
- 17, 18, 19 Am Health Drug Benefits. 2015 Aug;8(Spec Issue):13-14
- 20 Dermatol Surg. 2021 Apr 1;47(4):452-453
- 21 NIH ODS, Niacin
- 22 My Food Data, Top 10 Foods Highest in Vitamin B6 April 25, 2024
- 23 My Food Data, Top 10 Foods Highest in Vitamin B9 (Folate) April 25, 2024
- 24 Harvard Health Publishing, The A List for Vitamin B-12 Sources (Archived)
- 25 Melanoma Manag. 2015 Feb 25;2(1):51–61
- 26 Melanoma Research 33(2):p 126-135, April 2023
- 27 Oxid Med Cell Longev. 2014 Mar 26;2014:860479
- 28 Nutrients 2017, 9(8), 866
- 29 Cleveland Clinic, April 10, 2023
- 30 Aspects of Molecular Medicine Volume 5, June 2025, 100063
- 31 Int J Mol Sci. 2021 Jun 6;22(11):6112
- 32 J Cancer. 2024 Jan 1;15(1):1-19
- 33 JMIR Dermatol. 2024 Mar 14;7:e51962
- 34 EWG.org The Trouble with Ingredients in Sunscreens
Turmeric Extract May Prevent, Even Reverse Diabetes (Type 1 and 2)
© GreenMedInfo LLC. This work is reproduced and distributed with the permission of GreenMedInfo LLC.
Want to learn more from GreenMedInfo? Sign up for the newsletter here:
www.greenmedinfo.com/greenmed/newsletter
Reproduced from original article:
https://greenmedinfo.com/blog/turmeric-extract-may-prevent-even-reverse-diabetes-type-1-and-2-1
Posted on: Friday, September 6th 2019 at 6:15 am
Written By: Sayer Ji, Founder
This article is copyrighted by GreenMedInfo LLC, 2022

What if the long sought after “cure” for diabetes was as safe, affordable, and accessible as a spice sitting in your kitchen cupboard?
“Leave your drugs in the chemist’s pot if you can cure the patient with food.” -Hippocrates, 420 BC
Slowly but surely the world is waking up to the reality that diabetes is not only a preventable but in some cases a reversible condition, and that the drug-based model of symptom suppression and disease management has fatal flaws. For instance, some of the drugs used to treat type 2 diabetes actually increase the risk of death, with a ground-breaking 2013 study showing GMO insulin given to type 2 diabetics may lead to the development of so-called “double diabetes“: type 2 and type 1 diabetes, together. Clearly, if medicine can’t at least abide by its founding principle to “do no harm,” it must seek the answer somewhere other than from the “chemist’s pot.”
As the pharmaceutically-driven medical paradigm continues to lose adherents by the droves, and the public seeks a system that identifies and resolves the root causes of disease, interest is growing in the use of natural substances and lifestyle modifications to prevent and treat blood sugar disorders. And unlike a few decades ago, where most of the evidence for “natural healing” was anecdotal, there are now tens of thousands of studies on hundreds of natural substances and therapeutic activities that may ameliorate blood sugar disorders and their complications. You can check out a good portion of the relevant research on the topic on GreenMedInfo.com’s blood sugar disorder database.
While plants like cinnamon and gymnema sylvestre have received plenty of attention for diabetes over the years, one special plant extract that is beginning to stand out from the crowd as being exceptionally valuable as an anti-diabetic agent is turmeric. There are, in fact, 21 articles on turmeric’s value in type 2 diabetes on our database alone.
Turmeric’s primary polyphenol curcumin is the main compound in the plant that has been researched for it’s blood sugar regulating properties. One particularly striking study, published in the American Diabetic Association’s own journal, Diabetes Care, found turmeric extract to be 100% effective in preventing pre-diabetics from developing type 2 diabetes — a feat of prevention that no FDA approved drug for type 2 diabetes has yet come even close to accomplishing.
Turmeric Extract May Reverse Pancreatic Damage In Type 1 Diabetes
The truth is that this extraordinary spice may be a powerful therapeutic intervention for more than just type 2 diabetics. Pre-clinical research now reveals it may have a role in reversing pancreatic damage in insulin-dependent, type 1 diabetics, who are routinely told that their condition can not be cured. Type 1 diabetics are rarely educated to the fact that the root cause of their disorder can be addressed: namely, that the deficiency and/or dysfunction of the beta cells in the pancreas responsible for producing insulin can be repaired, as well as the autoimmune issues at the heart of the problem.

In 2013, an exciting study published in the journal Diabetology & Metabolic Syndrome titled, “The effect of a novel curcumin derivative on pancreatic islet regeneration in experimental type-1 diabetes in rats (long term study),” found that diabetic rats who received a novel water-soluble, high concentrate (53.21%) curcumin derivative orally for 40 days showed an improvement of their plasma glucose, insulin and C-peptide (a marker for the health and insulin producing capability of the beta cells) levels, that began after about 4 months, and continued to improve until the 10 month mark, when their values were almost completely normalized and evidence of significant pancreatic regeneration could be observed. The researchers concluded the novel curcumin derivative (NCD): “…possesses antidiabetic actions and enhanced pancreatic islets regeneration.”
.png)

The daily dose used in this rodent study (80 mg/kg) was the body weight equivalent of 6,400 mg or 6.4 grams of curcumin for an average North American male adult (80 kilograms/176 lbs). Rodent and human physiology is, of course, radically different, but significant crossovers nonetheless do exist. In another article, titled “Why Turmeric May Be the Diseased Liver’s Best Friend,” we reviewed research indicating that turmeric may help to reverse damage in and even regenerate the diabetic liver, as well as safety literature on what is a safe human dose:
“A 2001 study in cancer patients reported that quantities of curcumin up to 8 g, administered per day for three months, were not toxic and resulted in significant anti-cancer properties in a number of those treated.[5] Considering that turmeric is only 3-4% curcumin by weight, this implies that a larger quantity of turmeric can be consumed safely, as well.”
Given that organ transplantation (pancreatic islet transplants) is exceedingly expensive and prohibitive due to a lack of donor material and the potential for rejection by the host, the notion that a safe, affordable, and non-prescription spice extract like curcumin may have significant therapeutic value and may even regenerate damaged pancreatic tissue, is truly exciting. That said, it should be noted that since curcumin is not patentable, it is unlikely the 800 million dollars or more needed to fund the requisite clinical trials needed to obtain FDA drug approval will materialize. Because the so-called “evidence” needed to justify the use of a new treatment is locked behind an insurmountably high paywall, don’t count on randomized, controlled, trials being performed on this “natural cure” in the near or distant future.
In this study, the authors surmised that the ameliorative effects curcumin treatment on type 1 diabetic rodents observed were the result of beta cell regeneration and they explained the theory behind how this works:
“Each tissue or organ is believed to contain a small sub-population of cells that is capable of self-renewal and has the ability to give rise to each mature cell type [47]. Thus, one of the most promising sources of beta cells might be pancreatic stem cells.”
The researchers theorized that curcumin likely produces,
“…a favorable systemic and pancreatic environment to foster bone marrow transplantation and islet neogenesis. Accordingly, administration of curcumin; as an established anti-inflammatory and immune modulatory drug; would likely boost and preserve the process of islet regeneration; which was evidently proven true in this study.”
Curcumin’s “immunomodulatory” benefit in type 1 diabetes, also known as autoimmune diabetes, appears to be based on it reducing the activity of the host immune system in attacking self-structures. In fact, another recent study, published in 2014 in the journal Clinical and Experimental Immunology titled, “Curcumin ameliorates autoimmune diabetes. Evidence in accelerated murine models of type 1 diabetes,” found that curcumin down-regulates the T cell response that destroys pancreatic beta cells, resulting in an improvement in autoimmune or type 1 diabetes.
It is important for the reader to know that curcumin is not a magic bullet; nor is it the only natural substance studied to have potential beta cell regenerative properties. Indeed, pancreatic regeneration has been induced experimentally for at least 23 different natural substances. We have a keyword dedicated to indexing relevant research on the topic here: beta cell regeneration. We’ve highlighted 10 of the most compelling ones in our article, “10 Natuaral Substances That Could Help Cure Type 1 Diabetes.”
As the research continues to accumulate on the value of natural substances for disease prevention and treatment, it is clear the future of medicine will rely on returning to the wisdom of the ancients, where Hippocrates’ fundamental principle that one can “cure the patient with food” is once again passionately embraced.
Are you a health professional or just a serious research geek? Interested in taking your the GreenMedInfo experience to the next level? Learn about our GMI pro membership features, which includes access to our research PDF database of over 150,000 documents. Learn More Here.
Is Zinc the Missing Nutrient in Childhood Asthma Care?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/09/23/zinc-childhood-asthma.aspx
Analysis by Dr. Joseph Mercola September 23, 2025

Story at-a-glance
- Childhood asthma affects 4.6 million U.S. kids, and research now shows zinc deficiency drives more inflammation, worse lung function, and greater breathing problems
- Zinc strengthens airway barriers, trains immune cells, reduces allergic inflammation, and helps repair tissues, making it central to protecting children against worsening asthma symptoms
- A review in Nutrients found zinc deficiency in children consistently linked to more severe asthma and allergic rhinitis, with greater benefits when levels were restored
- A large U.S. analysis showed overweight children eating more zinc-rich foods had up to 29% lower odds of asthma and fewer attacks compared to peers
- Zinc works best when sourced from whole foods like beef, lamb, oysters, and eggs, with supplements serving only as a backup when your diet falls short
Asthma is one of the most common chronic diseases in children, characterized by wheezing, coughing, chest tightness, and shortness of breath. The U.S. Centers for Disease Control and Prevention (CDC) reports that 4.6 million children in America are currently living with asthma, making it a leading cause of missed school days and hospital visits.1
However, asthma is not just a breathing problem — it involves chronic inflammation of the airways that leaves the lungs hypersensitive to allergens, pollutants, and infections. This disease is deeply tied to a child’s immune system, and when it comes to optimal immunity, one of the key nutrients that you need is zinc.
Recent studies point to how having low levels of zinc correlates with more severe asthma. This brings forward an important question. Could improving zinc intake help children gain better control of this disease?
Zinc’s Multifaceted Role in the Body
Zinc is an essential mineral found throughout your body’s organs, tissues, and fluids. It’s the second-most abundant mineral in your body next to iron. Your muscles, bones, liver, and skin all need zinc to function optimally — it’s actually involved in “over 300 enzyme-mediated reactions, gene transcription, and protein structure.”2 Here are some of zinc’s important functions:
• Protects your cells from free radicals — Zinc works within the redox cycle, where it competes with metals like iron and copper to limit the creation of most damaging free radicals, preventing unnecessary harm to your cells.
• Acts as a coenzyme for copper-zinc superoxide dismutase — This antioxidant enzyme stops fats in your cell membranes from breaking down (lipid peroxidation), keeping inflammation in check and tissues healthier.
• Supports the thymus gland — Zinc keeps thymulin, a hormone in the thymus, at healthy levels, which allows T cells to mature properly. T cells are the immune system’s frontline soldiers, and without zinc, they don’t develop as they should.
This lack of development pushes the immune system toward what’s called a Th2-dominant state. To put it simply, this means your body reacts to harmless triggers — like dust or pollen — as if they were dangerous, sparking allergic inflammation.
• Influences other key immune players — It regulates group 2 innate lymphoid cells, which are important in managing asthma and allergies. Zinc also keeps dendritic cells, which decide whether to spark or tolerate an immune reaction, balanced.
• Acts like a shield for your body’s barriers — It keeps the epithelial lining, the thin layer of cells that covers your airways and skin, strong and intact. It does this by stabilizing proteins called tight junctions that hold cells together, creating a protective wall. When zinc is lacking, that wall weakens, and allergens or irritants can slip through more easily, leading to chronic inflammation and hypersensitivity.
• Supports apoptosis (programmed cell death) — By doing so, zinc helps prevent unnecessary cell loss and ensures tissues repair effectively. It allows the body to heal from oxidative stress or toxic exposures without spiraling into chronic damage. This protective role highlights why zinc is so important in preventing atopy, the genetic tendency to develop allergic conditions like asthma, eczema, and hay fever.
However, your body has no way to store zinc long-term; this means you have to constantly get it from your diet. Without a steady daily supply, you risk falling short and becoming zinc-deficient. For children dealing with asthma, this deficiency could be an important reason why their symptoms worsen.
Zinc’s Link to Childhood Asthma Becomes Clearer
A recent literature review published in Nutrients gathered evidence on how zinc influences childhood asthma and allergic rhinitis. It highlights this nutrient’s effects on oxidative stress and immune balance, and why it could be the missing piece in children’s asthma care.3
The researchers analyzed both observational and interventional studies to determine how zinc — along with other nutrients — shapes the severity of symptoms, lung function, and even the long-term outlook for airway health.
“Trace elements like zinc and iron, and vitamins like A, C, and D, can alter the immune response and enhance the body’s antioxidant capacity. These are often deficient in children suffering from atopy, with zinc and vitamin A deficiency linked to airway inflammation,” an article in News-Medical.net reports.4
• What defines zinc deficiency? Certain factors affect zinc levels, such as age, gender, inflammation, and individual body rhythms. However, the levels are different between adults and children. In children 10 years old and below, this is defined as having zinc levels below 70 µg/dL in males and 66 µg/dL in females. Meanwhile, adults are considered zinc-deficient if they have levels below 74 µg/dL (males) and 70 µg/dL (females).5
• Children living with asthma and allergies formed the focus of this research — In these groups, zinc deficiency was consistently associated with more severe disease. These children appear to have worse lung function, higher oxidative stress, and more frequent breathing issues. And even though zinc deficiency was not always “severe enough” to meet the lab cutoffs used in adults, the children still experienced worse outcomes when their zinc levels ran low.
• One striking finding was the effect of zinc on allergic rhinitis — Children with this condition were more likely to have swollen nasal tissues and lower zinc levels in their blood. Interestingly, during acute allergy flare-ups, zinc levels in the mucosa (the lining inside the nose) actually increased, hinting that zinc shifts to the site of inflammation. This redistribution indicates that zinc is actively pulled into the tissues where it is needed most, leaving less circulating in the bloodstream.
• Zinc status also matters during the developmental stage — The researchers noted that when mothers had adequate zinc during pregnancy, their children had better lung function and a lower risk of developing asthma, proving that zinc’s role starts even before a child is born.
• The most significant improvements were observed in kids with lower zinc levels to begin with — This suggests that zinc supplementation offers the biggest payoff when deficiency is present. In other words, if your child already eats plenty of zinc-rich foods like beef, lamb, or shellfish, supplementation might not create dramatic changes. But if their diet lacks these foods, the difference in breathing and recovery could be much more noticeable.
• The delivery method also affects the outcome — While some trials found zinc supplementation led to improvements, others reported little change. These inconsistencies were often due to variations in dosage, duration, or even whether the zinc was given orally or intranasally.
This research made one thing clear: Zinc deficiency is not just a side note in asthma care; it’s a driver of worse symptoms, more inflammation, and weaker immune control. For children struggling with breathing problems, ensuring adequate zinc intake offers a practical way to support recovery and resilience alongside conventional treatments. And in asthmatic children dealing with other health conditions like obesity, optimizing levels of this nutrient becomes even more important.

Save This Article for Later – Get the PDF Now
Zinc Shows Protective Effects in Overweight Children with Asthma
A 2024 cross-sectional analysis published in the World Allergy Organization Journal investigated how dietary zinc intake influences asthma in overweight and obese children and adolescents. The researchers used data from the U.S. National Health and Nutrition Examination Survey (NHANES) between 2011 and 2020 to determine whether children struggling with both excess weight and asthma had lower zinc intake compared to their healthier peers.6
• The study analyzed 4,597 overweight or obese children and adolescents under 20 years old — Of this population, 963 have asthma. After adjusting for confounding factors, the researchers discovered that higher zinc intake consistently correlated with a reduced asthma risk.
• The researchers divided the participants based on their dietary zinc intake — Four groups were created, based on the lowest to highest intake. Compared to the lowest intake group, children in the second quartile had 22% lower odds of asthma, while those in the third quartile had 24% lower odds. Those in the fourth quartile had 29% lower odds.
• This connection held even after adjusting for asthma treatments — Children with higher zinc intake also had fewer recent asthma attacks, strengthening the case that zinc isn’t just about long-term risk but could also make day-to-day management easier.
• Sensitivity analyses (tests that check whether findings hold under different assumptions) confirmed the results — However, because the study was cross-sectional, it cannot prove that zinc intake directly prevents asthma; only that the two are strongly linked. Even so, it strengthens the notion that improving zinc intake is a safe and low-cost step that supports a child’s health. According to the researchers:
“Our findings align with existing research, even if the precise mechanisms by which zinc influences asthma in overweight or obese individuals remain incompletely known. Zinc, recognized for its antioxidant properties, contributes to diminishing oxidative stress through a variety of mechanisms.”7
• Zinc does not act in isolation — A separate 2024 study published in the World Journal of Clinical Pediatrics looked at how zinc levels and other related blood markers affect asthma symptoms. The researchers found that ferritin, a protein that stores iron, was significantly higher in asthmatic children as well.
Zinc and ferritin work in a web of immune responses. When ferritin rises due to inflammation, zinc’s role in balancing oxidative stress and supporting immune cells becomes even more important.8
Overall, these studies prove that nutrition is not just background noise in asthma care — it plays a measurable role. As News-Medicat.net concludes:
“These results emphasize the importance of considering nutritional factors in asthma management and warrant further research into the therapeutic potential of zinc supplementation. Future studies using prospective cohort designs and randomized controlled trials may shed further light on the causal effect of dietary zinc intake on alleviating asthma in this population.”9
Practical Steps to Address Zinc Deficiency in Childhood Asthma
If your child is struggling with asthma, it’s important to go beyond just treating the symptoms. The real problem often starts with inflammation and an overactive immune response. Zinc plays a key role in calming that inflammation, strengthening airway barriers, and keeping the immune system balanced. Here are five practical steps for you to take to help optimize their zinc levels:
1. Make zinc-rich foods part of your daily meals — The most reliable way to improve zinc intake is through food. Focus on meats like grass fed beef and lamb, along with seafood such as oysters or shrimp (derived from safe, clean sources). These foods give your child zinc in a form the body uses easily.
Pastured eggs, beans, and lentils also provide zinc, but know that the zinc they provide isn’t absorbed as efficiently. Adding vitamin C-rich foods like fruit at the same meal helps your body use zinc from plants better.
2. Minimize ultraprocessed and junk foods from their diet — Processed meals often contain seed oils and additives that irritate the body and make asthma symptoms harder to manage. In addition, while zinc is often used in breakfast cereals and other packaged fortified foods, I recommend avoiding these products. You will do far better by consuming the whole-food sources of zinc noted above.
3. Support your child during allergy seasons — If your child deals with allergies alongside asthma, know that their zinc gets pulled into inflamed tissues, especially in the nose and lungs. During high-pollen seasons, make sure meals are packed with zinc-rich options every day. If you’re already doing this, pay attention to whether your child still experiences worsening symptoms — this is often a sign that zinc needs to be boosted even further.
4. Don’t forget about pregnancy and early life nutrition — Adequate zinc intake during pregnancy helps shape your baby’s immune system and reduces their risk of developing asthma later. Focus on whole foods like meats, seafood, and eggs during pregnancy and breastfeeding to give your child the strongest start possible.
5. Use supplementation strategically if diet alone falls short — Always match supplementation with food-based sources so you aren’t relying on pills alone. Think of zinc supplements as a backup, not the foundation.
By addressing zinc deficiency head-on, you’re not just helping manage asthma flare-ups — you’re giving your child stronger immune defenses, healthier lung function, and better recovery when challenges arise.
Frequently Asked Questions (FAQs) About Zinc for Childhood Asthma
Q: Why is zinc important for children with asthma?
A: Zinc plays several key roles in protecting your child’s airways. It helps immune cells mature properly, reduces allergic inflammation, and strengthens the barriers that line the lungs. Zinc also supports tissue repair, so the body recovers better after flare-ups. Without enough zinc, your child’s immune system is more likely to overreact to harmless triggers like dust or pollen, making asthma symptoms worse.
Q: How common is asthma in children?
A: Asthma is one of the most widespread chronic conditions in children today. The CDC reports that 4.6 million children in the United States are currently living with asthma. It isn’t just about wheezing or shortness of breath — it’s also a major reason kids miss school and need urgent medical care, putting stress on both children and families.
Q: What does the research say about zinc and asthma?
A: Several studies have found that zinc deficiency is linked to more severe asthma symptoms. Kids with lower zinc levels often have poorer lung function, higher oxidative stress, and more frequent breathing issues. On the other hand, children who consume more zinc-rich foods are less likely to suffer attacks, and overweight children with higher zinc intake showed up to a 29% lower risk of asthma in one U.S. study.
Q: What foods provide the best sources of zinc?
A: The most effective sources of zinc are whole foods like beef, lamb, oysters, shrimp, and eggs. These give zinc in a form the body absorbs easily. Plant-based foods like beans and lentils also contain zinc, though less is absorbed. Pairing these with vitamin C-rich foods, like fruits, can help improve absorption. Relying less on processed or fortified foods and more on whole-food options is the best way to keep zinc levels healthy.
Q: Should I give my child zinc supplements for asthma?
A: Supplements are helpful mainly when there is a real deficiency or when diet falls short. The biggest improvements in breathing and recovery are usually seen in kids who start out with low zinc levels. Whole foods are ideally the foundation, with supplements acting as a backup if needed. Even then, it’s important to be consistent and combine them with good dietary habits for the best results.
Fisetin — An Unsung Hero in the Fight Against Vascular Calcification
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/03/fisetin-cardiovascular-benefits.aspx
Analysis by Dr. Joseph Mercola July 03, 2025

Story at-a-glance
- Fisetin, naturally found in strawberries, apples, and onions, prevents artery stiffness by halting harmful calcium buildup in blood vessels
- Regular consumption of fisetin-rich foods significantly reduces inflammation and oxidative stress, effectively lowering your risk of heart disease and stroke
- Fisetin enhances your body’s natural defenses by activating enzymes that switch off dangerous signals responsible for arterial calcification
- Eliminating ultraprocessed foods from your diet protects your arteries from chronic inflammation and metabolic damage
- Daily physical activity and targeted carbohydrate intake help maintain healthy insulin levels, which is essential for preserving flexible arteries and good cardiovascular health
One of the most overlooked threats to your cardiovascular health is vascular calcification, meaning your arteries harden and stiffen as calcium builds up within their walls.
When your arteries lose flexibility, your heart works harder to pump blood, significantly raising your risk for hypertension, heart attack, and stroke. In fact, you could have it right now. Research indicates that nearly half of all adults over the age of 60 have some level of calcification throughout their body, also known as diffuse calcification.1
To manage the issue, researchers are turning towards fisetin, a natural flavonol found abundantly in foods like strawberries, apples, and onions. Interestingly, fisetin also exhibits antioxidant and anti-inflammatory properties that promote better overall health.
Fisetin Prevents Calcium Buildup in Arteries
In a study published in Aging,2 researchers investigated how fisetin helps prevent vascular calcification, a process that makes your blood vessels stiff and less able to function properly. To conduct their study, they used human vascular smooth muscle cells, segments of mouse arteries, and a special mouse model that mimics calcification caused by too much vitamin D.
The team treated cells and tissues with high levels of calcium and phosphate, which simulates conditions that promote artery hardening, and then added fisetin. They closely monitored changes in calcification markers, such as genes and proteins involved in calcium deposition.
• The impact of fisetin on cardiovascular health — When fisetin was added, it dramatically reduced the buildup of calcium in the artery cells and in artery segments from mice. Specifically, it lowered activity levels of genes known to promote calcification, including BMP2, ALPL, and CBFA1.
For context, BMP2 is a gene that signals your body to start depositing calcium, ALPL promotes mineralization, and CBFA1 is crucial in transforming smooth muscle cells into bone-like cells — none of which you want happening in your arteries. In other words, fisetin directly interrupts the dangerous transformation of your artery cells from smooth, flexible structures into hardened, calcium-filled tissues.
• Going deeper into fisetin’s effectiveness — The researchers observed that fisetin significantly reduced calcification markers across all experimental setups, proving it is consistently beneficial, and this wasn’t a minor improvement at all. It was substantial enough to suggest that regular intake of fisetin-rich foods or supplementation could effectively shield your arteries from harmful calcium buildup.
Interestingly, these benefits hinged strongly on one crucial enzyme called dual-specificity phosphatase 1 (DUSP1). When researchers turned it off, fisetin lost its protective effects completely. Even worse, shutting down this enzyme increased calcification, showing that DUSP1 is what fisetin activates to halt the hardening of arteries.
• Fisetin works right away — Time-related specifics were equally striking. In mouse models overloaded with vitamin D (a known way to rapidly induce artery calcification) the introduction of fisetin led to visible improvements in as little as two weeks. Calcium deposits were lower, showing fisetin works swiftly to prevent artery stiffening from progressing once introduced.
• Groups who will benefit the most from fisetin — The research strongly indicates that anyone already at risk from conditions like kidney disease, diabetes, or vitamin D overload (which excessively raises calcium levels) will likely see significant heart-health benefits from fisetin. These groups typically face higher risks of rapid vascular calcification.
Conversely, the effectiveness of fisetin compared to untreated scenarios was stark. Cells and tissues exposed to high phosphate and calcium without fisetin quickly became calcified, mirroring the conditions that lead to stiff, blocked arteries in people. But with fisetin treatment, those same tissues remained flexible and significantly less mineralized.
• A look into the biological processes — The central player in vascular calcification is a protein called p38 mitogen-activated protein kinase (p38 MAPK). Think of this protein as a harmful switch that, when activated by stress signals like excess calcium and phosphate, instructs your artery cells to harden and calcify.
Fisetin’s primary action involves activating DUSP1. When it raises the levels of DUSP1, p38 MAPK gets turned off, blocking the harmful signal pathway.
• Fisetin also helps maintain balance in cell signaling — Normally, cells in your arteries carefully regulate their internal calcium levels, but certain conditions disrupt this balance. High phosphate, chronic inflammation, and metabolic disorders upset calcium regulation, pushing smooth muscle cells toward calcification. By enhancing DUSP1 activity, fisetin restores balance, preserving the natural state of your arteries and safeguarding your cardiovascular system from unnecessary strain.
• The dual role of fisetin for your overall health — Not only does fisetin halt calcium buildup, it also addresses inflammation and oxidative stress, which are powerful contributors to artery disease.
Other Health Benefits of Increasing Fisetin Intake
In a meta-analysis published in Acta Scientific Nutritional Health,3 researchers investigated the different health-promoting effects of fisetin. Moreover, they highlighted its specific advantages for your cardiovascular system.
• Maintain lipid balance — This means your cholesterol and triglyceride levels become healthier. Animal studies showed substantial reductions in LDL cholesterol, commonly called “bad cholesterol,” and triglycerides after fisetin administration. This improvement is essential because lower LDL and triglycerides directly reduce your risk of plaque buildup in arteries, thereby dramatically lowering your chance of heart attack or stroke.
• Improve insulin sensitivity — This is a critical factor for managing and preventing Type 2 diabetes and its related cardiovascular complications. Laboratory tests showed improvements within weeks of fisetin supplementation, particularly on animal models of insulin resistance.
• Manage blood pressure — Several studies cited in the review demonstrated significant drops in blood pressure after fisetin was administered regularly. High blood pressure puts relentless strain on your heart and arteries, increasing risks of severe cardiac events.
• Control metabolic dysfunction — The most substantial cardiovascular benefits of fisetin appeared among test animal models. In these groups, fisetin not only normalized cholesterol levels and blood pressure, but also reduced inflammation. These benefits could also translate for human applications, too.
• Modulate the MAPK pathway — As noted in the previous study, this pathway triggers inflammatory responses in your blood vessels, contributing to plaque buildup and vascular damage if unchecked. Studies reviewed showed that fisetin blocks these inflammatory signals at their source, creating powerful protection against heart disease.
• Antioxidant capabilities — Antioxidants help neutralize harmful free radicals, and fisetin stands out because it specifically protects cardiovascular tissues. Previously published literature outlined in the featured study illustrated that fisetin directly scavenges damaging free radicals in heart cells, reducing oxidative stress and minimizing tissue damage.
When oxidative stress is controlled, your heart stays healthier and functions more effectively, significantly reducing your risks of long-term cardiovascular conditions.
• Anticancer properties — Interestingly, the researchers noted that fisetin helps fight cancer, specifically by activating tumor suppressor pathways through the p53 protein:4
“P53 is often referred to as the ‘guardian of the genome’ because it regulates critical cellular processes, such as DNA repair, cell cycle arrest, and apoptosis (programmed cell death), in response to cellular stress or DNA damage.
In many cancers, p53 is either mutated or downregulated, leading to uncontrolled cell growth and evasion of apoptosis. Fisetin has been shown to restore or enhance the function of p53, promoting cell cycle arrest and apoptosis in cancer cells.”
• Endothelial function support — Healthy endothelial cells are crucial for proper circulation, blood pressure control, and overall heart health, and fisetin was shown to help keep endothelial cells functioning optimally, maintaining healthy blood vessel dilation and smooth blood flow.

Save This Article for Later – Get the PDF Now
How to Protect Your Arteries and Improve Cardiovascular Health
If you’re dealing with early signs of arterial stiffness or simply want to ensure your cardiovascular system remains strong, tackling the root causes is your best strategy. Here are my recommendations to help you effectively improve your heart health naturally:
1. Boost your fisetin intake through diet — Start incorporating more fisetin-rich foods into your meals daily. Strawberries, apples, onions, cucumbers, and even persimmons contain significant amounts of this beneficial flavonol. As the prior studies have shown, increasing your fisetin intake will help reduce the risk of artery calcification, as well as lower inflammation, and improve overall heart health.
2. Cut out ultraprocessed foods from your life — Avoiding ultraprocessed foods, especially those high in linoleic acid (LA) is one of the most effective steps to protect your cardiovascular system.
These synthetic products directly fuel inflammation and oxidative stress, which are major drivers of artery stiffness. Instead, replace these harmful choices with whole, nutritious foods. Ideally, swap high-LA vegetable oils with healthy fats instead, such as grass fed butter, ghee, or tallow.
For a detailed explanation of the dangers that LA poses to human health, I encourage you to read my study published in Advances in Redox Research.5 There, I discuss crucial topics, such as LA’s effect on cardiolipin, metabolic function, and gut microbiome.
3. Get moving with regular exercise — Make exercise a non-negotiable part of your routine. Whether it’s biking, swimming, or lifting weights, regular physical activity significantly reduces inflammation and insulin resistance, improving the flexibility and health of your arteries.
If you are new to exercise, I recommend you start walking. This simple act, done gradually and steadily, is one of the most effective forms of exercise anyone can do. Best of all, it’s an exercise that can’t be overdone. For an in-depth look at the benefits of walking, read “The Benefits of Walking — How to Get More Steps in This Summer.”
4. Lose excess weight — In relation to the previous point, excess weight leads to plaque buildup in your arteries, thus restricting blood flow to your heart. Ultimately, this affects your other organs, too, as they won’t get enough blood. To help you tackle the root cause of obesity, read “Study Challenges the Current Definition of Obesity.”
5. Boost your vitamin K2 intake — This nutrient serves as your body’s master regulator for calcium distribution, ensuring that it supports important functions instead of calcifying your arteries. That said, I recommend boosting your K2 intake via fermented foods, such as natto and homemade fermented veggies. Certain cheeses, such as Munster, Gouda, and Brie, are also rich in vitamin K2.
Frequently Asked Questions (FAQs) About Fisetin and Vascular Calcification
Q: What is vascular calcification, and why is it harmful?
A: Vascular calcification occurs when calcium builds up in artery walls, making them stiff and less flexible. This condition increases the risk of hypertension, heart attacks, and strokes, especially prevalent among adults over age 60.
Q: How can fisetin help prevent vascular calcification?
A: Fisetin, a naturally occurring flavonol found in strawberries, apples, and onions, prevents artery calcification by activating the enzyme DUSP1. This enzyme inhibits harmful signals (specifically the p38 MAPK pathway) that otherwise lead to hardened arteries.
Q: Who would benefit most from increasing fisetin intake?
A: Individuals with conditions like kidney disease, diabetes, or those experiencing excessive vitamin D intake can gain cardiovascular benefits by regularly consuming fisetin-rich foods or supplements.
Q: Beyond cardiovascular health, what other health benefits does fisetin provide?
A: Fisetin supports overall health by improving cholesterol and triglyceride levels, enhancing insulin sensitivity, lowering blood pressure, reducing oxidative stress, and exerting anticancer effects by activating the p53 tumor suppressor pathway.
Q: What dietary and lifestyle changes can I make to improve cardiovascular health?
A: To protect your heart and arteries, incorporate more fisetin-rich foods (like strawberries, onions, apples), eliminate ultraprocessed foods, increase physical activity, manage body weight, and consume vitamin K2-rich foods like fermented vegetables and specific cheeses (Gouda, Brie, and Munster).
Heart attack survivors face a hidden nightmare: Two-thirds develop brain damage
Reproduced from original article:
https://www.naturalhealth365.com/heart-attack-survivors-face-a-hidden-nightmare-two-thirds-develop-brain-damage.html
by: June 28, 2025</span
 (NaturalHealth365) You beat the odds. You survived a massive heart attack when your heart literally stopped doing its job. The doctors called you lucky. Your family threw a celebration. You thought the worst was behind you.
(NaturalHealth365) You beat the odds. You survived a massive heart attack when your heart literally stopped doing its job. The doctors called you lucky. Your family threw a celebration. You thought the worst was behind you.
Then you tried to go back to your normal life and realized something was wrong.
You can’t remember where you put your keys. Simple conversations leave you confused. Tasks you’ve done a thousand times suddenly feel impossible. Your brain feels like it’s wrapped in thick fog that never lifts.
Welcome to the nightmare that doctors don’t warn you about – and a shocking new study reveals it’s happening to almost everyone who survives cardiogenic shock.
Two-thirds of survivors get their brains scrambled
Researchers from UT Southwestern Medical Center just released a bombshell report that should wake up every person dealing with heart disease.
They tracked 141 people who survived cardiogenic shock – a life-threatening condition where your heart literally can’t pump enough blood to keep your organs alive – and discovered that 65% developed new brain damage by the time they left the hospital. Even worse, 53% were still mentally impaired three months later.
Dr. James de Lemos, who led this research, didn’t mince words: “Nearly two-thirds of cardiogenic shock survivors experienced cognitive impairment within three months of hospital discharge, underscoring a critical but overlooked aspect of recovery.”
Think about those numbers for a second. If you survive one of the most catastrophic heart events possible, you’ve got better than a coin flip’s chance of walking out of that hospital with a damaged brain. And nobody, not your cardiologist, not your nurses, not your discharge team, is going to warn you about it.
What cardiogenic shock does to you
Here’s what happens when your heart goes into cardiogenic shock: it basically gives up. Whether from a massive heart attack, severe heart failure, or surgical complications, your heart just stops pumping enough blood to keep you alive.
About 100,000 Americans go through this hell every year. Until recently, most people died. Period. However, medical technology has advanced to the point where up to 70% of patients now survive the initial event.
The problem? While doctors are patting themselves on the back for keeping you breathing, your brain is slowly starving to death.
Your brain needs about 20% of all the blood in your body to function properly. When your heart can’t pump enough blood, your brain cells start dying from oxygen starvation. Even if the medical team manages to get your heart working again, the damage to your brain tissue might already be permanent.
The medical cover-up that’s destroying lives
The medical establishment has known for years that heart problems cause brain damage, but they have not paid much attention to what kind of life they’re sending people back to.
Dr. Eric Hall, who led the study, admits: “We found that cardiogenic shock is associated with cognitive impairment, which is an under-recognized consequence strongly linked to patients’ overall quality of life.”
“Under-recognized” is medical speak for “we’ve been ignoring this massive problem for decades.”
So imagine yourself lying in that hospital bed, grateful to be alive, while doctors explain your discharge instructions. Nobody mentions that there’s a two-thirds chance you won’t be able to think straight for months – maybe years. Nobody suggests cognitive testing. Nobody connects you with brain specialists who might be able to help.
You get sent home to discover your mental decline on your own, wondering if you’re going crazy.
How to protect yourself before crisis strikes
The harsh truth is that once your heart goes into cardiogenic shock, the brain damage is probably already happening. Your best defense is to ensure your heart never reaches that point.
Here’s how to keep your heart so strong it never fails catastrophically:
Ditch the foods that are literally poisoning your cardiovascular system. Processed junk, sugar-loaded garbage, and those toxic seed oils they put in everything are creating chronic inflammation that’s slowly destroying your heart and blood vessels.
Feed your heart the nutrients it actually needs to stay strong. CoQ10, magnesium, omega-3s, and hawthorn berry are beneficial for your cardiovascular system.
Stop treating symptoms and start fixing root causes. High blood pressure, insulin resistance, and chronic stress are all warning signs that your heart is headed for trouble. Most doctors just want to throw pills at these problems instead of actually solving them.
Get real testing that can catch problems before they kill you. Standard heart tests often miss early problems that advanced testing can identify years in advance. For example, talk to a holistic doctor about C-reactive protein (CRP) and fibrinogen, two tests that measure levels of inflammation in the body.
Improve your body’s detoxification systems. Environmental toxins, heavy metals, and chronic infections are all attacking your cardiovascular system. Your liver, kidneys, and lymphatic system need support to protect your heart from this toxic assault.
Your heart and brain are connected, whether doctors admit it or not
What happens to your heart directly affects your brain. When your cardiovascular system breaks down, your brain pays the price. The medical system might want to treat these as separate issues, but your body knows better.
Thousands of people are walking around right now thinking they’re “heart attack survivors” when they’re actually brain damage victims who don’t even know what happened to them.
If you are ready to give your heart the protection it needs, consider Jonathan Landsman’s Cardiovascular Docu-Class, featuring 22 leading heart health experts who understand the real connection between heart and brain health. These aren’t the same doctors who ignore cognitive damage – these are experts who know how to prevent heart disease before it destroys your life and your mind. Get lifetime access to strategies that could save both your heart and your ability to think clearly.
Sources for this article include:
