Kidney
now browsing by category
Common Dry-Cleaning Chemical Linked to Liver Damage
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/11/25/tetrachloroethylene-pce-liver-damage.aspx
Analysis by Dr. Joseph Mercola November 25, 2025

Story at-a-glance
- A widely used grease remover and dry-cleaning chemical called tetrachloroethylene (PCE) has been linked to liver fibrosis, a condition that causes scarring and loss of liver function even in people who don’t drink alcohol or have obesity
- Researchers found that people with measurable levels of PCE in their blood were three times more likely to have liver fibrosis, and for every tiny one-nanogram-per-milliliter increase in PCE, the risk increased fivefold
- PCE exposure often occurs through inhaling fumes from dry-cleaned clothes, contaminated air, or drinking water, and the chemical can also enter through the skin, affecting the liver, kidneys, heart, and nervous system
- Long-term exposure to PCE has been linked not only to liver disease but also to nerve damage, reproductive issues, and several cancers, including those of the bladder and liver, prompting the EPA to begin phasing it out
- Lower your risk of liver damage by switching to solvent-free wet cleaning, letting dry-cleaned clothes air out before use, replacing household products that contain PCE, and supporting liver repair through clean nutrition, hydration, and sun exposure
Liver disease can arise from certain factors, such as alcohol consumption, a high-fructose diet, excessive fat buildup in the organ, and diseases like hepatitis B or C. But now, research reveals another possible cause — and it’s found in many everyday products like household degreasers and dry-cleaned clothes.
This chemical, known as tetrachloroethylene (PCE), is used to remove grease from metal parts, fabrics, and household surfaces. PCE is now under intense scrutiny after new findings reveal that it can lead to liver damage, particularly liver fibrosis.
Researchers Link PCE to Hidden Liver Damage
A recent study published by researchers from Keck Medicine of USC analyzed PCE exposure affects the liver. The study, published in Liver International,1 examined data from the National Health and Nutrition Examination Survey (NHANES), a long-running health survey that tracks chemical exposure and disease trends in the United States.2
• Conducting the study — The researchers measured PCE exposure by analyzing blood samples from 1,614 adults aged 20 and older collected between 2017 and 2020 — the most recent data available. They found that about 7% of the population had measurable levels of PCE in their bloodstream, which is a clear sign of ongoing environmental exposure.
• Comparing PCE levels — The researchers next compared individuals with detectable PCE in their blood to those without it. What they found was striking — those exposed to this chemical were three times more likely to develop significant liver fibrosis. This implies that even people who don’t drink alcohol or are obese could still develop liver scarring due to this invisible environmental toxin. In addition, these findings remained consistent regardless of age, sex, race, ethnicity, or education level.
• What is liver fibrosis? Simply put, fibrosis refers to scarring that disrupts the liver’s ability to filter toxins and regulate metabolism. It’s characterized by appetite loss, nausea, unexplained weight loss, and weakness. When fibrosis becomes severe and extensive, it leads to liver cirrhosis.3
• The higher the levels, the greater the risk — For every single nanogram per milliliter increase of PCE in the bloodstream — an amount so tiny it’s measured in billionths of a gram — the risk of liver fibrosis increased fivefold. This indicates that even small, consistent exposures could have serious long-term effects, making it particularly concerning for those regularly exposed to the chemical.
• PCE exposure overrides typical liver disease risk factors — Notably, when this chemical was present, alcohol use and liver fat accumulation associated with obesity and other health conditions did not seem to contribute to significant liver fibrosis. According to Dr. Brian P. Lee, hepatologist and liver transplant specialist with Keck Medicine and the study’s lead author:
“Patients will ask, how can I have liver disease if I don’t drink and I don’t have any of the health conditions typically associated with liver disease, and the answer may be PCE exposure. The findings suggest that exposure to PCE may be the reason why one person develops liver disease while someone with the exact same health and demographic profile does not.”4
Facts About PCE — What It Is and How You Can Become Exposed
The researchers of the featured study noticed something unexpected about the population most at risk — They found that those who had greater PCE exposure came from higher-income households.5 This is because these people were more prone to getting their clothes dry-cleaned. In fact, dry cleaning is one of the main sources of exposure to this chemical.6
• PCE is colorless and used in various products — Also called perchloroethylene or ethylene tetrachloride, this clear, colorless, human-made liquid has been used not just as a dry-cleaning solvent, but also in household goods and other industrial settings. It has numerous uses, such as for removing grease, a heat transfer medium, and a drying agent for metals.
• Its odor is defined as sweet and similar to ether — However, relying on smell to detect exposure is misleading because the odor threshold (the level at which a person notices the smell) varies greatly and usually appears long after toxic exposure has already occurred. That means you could be breathing dangerous levels of PCE without even realizing it.
• Contaminated air and water are also sources of PCE — This chemical is released into the air over time, especially from freshly dry-cleaned clothes that continue to emit fumes even after cleaning. It also contaminates drinking water when spills or improper disposal allow the chemical to seep through soil layers and enter the groundwater supply.7
• PCE can easily enter the body — It can be inhaled, absorbed through the skin, or even enter through contaminated water or food. Once inside your body, it affects multiple organs, including the liver, kidneys, heart, and nervous system.
• Previous studies have linked this chemical to liver damage — While the featured study did shed light on how PCE can lead to liver fibrosis, there are earlier studies that have warned about its liver-damaging effects. According to an archived report from Agency for Toxic Substances and Disease Registry (ATSDR), PCE exposure has been associated with conditions such as hepatomegaly (an enlarged liver) and hepatocellular injury (damage to liver cells).8
Laboratory and occupational studies have also shown elevated levels of liver enzymes, indicating cellular stress and inflammation. Workers exposed to high levels of PCE in dry-cleaning facilities were found to develop these changes far more often than those who were not exposed.

Save This Article for Later – Get the PDF Now
PCE’s Dangers Extend Beyond the Liver
Because of its toxic nature, the U.S. Environmental Protection Agency (EPA) has initiated a 10-year plan to phase out PCE use in dry cleaning and has either banned or tightly restricted its use in many workplaces. Still, the chemical continues to appear in certain products and remains widely used in countries that lack comparable safety regulations.9 This is particularly concerning, as PCE has been associated with a wide range of side effects. Although some are mild, others are severe and life-threatening.10
• Physical contact with the chemical is dangerous — When PCE comes into contact with your skin and eyes, it will lead to irritation and burning. The skin may develop rashes, blisters, redness, dryness, and cracking as well. When inhaled, it will irritate the nose, throat, and lungs.
• Prolonged exposure can lead to more serious effects — These include nerve damage, heart rhythm problems, and reproductive harm. Pulmonary edema, a dangerous buildup of fluid in the lungs, can also occur with chronic exposure. It causes difficulty breathing, making it a life-threatening condition.
• The central nervous system is one of the most sensitive targets of PCE toxicity — This means your brain and nerves respond to the chemical even before other organs show damage. People exposed to this chemical via air or water often develop symptoms like dizziness, blurred vision, confusion, and headaches.
These neurological symptoms occur because PCE acts like an anesthetic. It slows brain activity and interferes with neurotransmission (the process by which nerve cells communicate). What’s most troubling is that these symptoms often fade once someone leaves the contaminated environment, making it easy to overlook or misdiagnose.
For anyone who works with solvents, noticing recurring “brain fog” or lightheadedness after a shift could be a warning sign that the body is overloaded with toxins.
• Kidney damage was another major finding highlighted in the ATSDR report — Studies have documented increases in urinary proteins such as beta-2 microglobulin and lysozymes among chronically exposed workers, which are early warning signs of tubular injury in the kidneys.
• The reproductive system also appears highly vulnerable — PCE exposure has been linked to menstrual irregularities, changes in semen quality, reduced fertility, and adverse pregnancy outcomes, including miscarriages, stillbirths, and low birth weight. Although the evidence varies across populations, researchers consistently found that PCE crosses the placenta and even appears in breast milk.
• PCE is carcinogenic — The International Agency for Research on Cancer has classified it as a probable human carcinogen;11 it’s strongly linked to several cancers in both humans and animals, which is why it needs to be handled with extreme caution. According to the New Jersey Department of Health Hazardous Substance Fact Sheet:
“There is evidence that it causes cancer of the liver, esophagus, bladder, and other types of cancer in humans. It has also been shown to cause cancer of the liver and leukemia in animals.
There may be no safe level of exposure to a carcinogen, so all contact should be reduced to the lowest possible level.”12
Limit Your Exposure to These Liver-Damaging Chemicals
The researchers highlight the importance of their findings, particularly for people who are at high risk of liver damage. “If more people with PCE exposure are screened for liver fibrosis, the disease can be caught earlier and patients may have a better chance of recovering their liver function,” Lee said.13
• The easiest way to reduce the risk is to remove the main sources of PCE in your environment — For example, if you use dry cleaning services, switch to wet-cleaning or CO₂-based methods that don’t rely on solvents. When you need to dry-clean garments, hang them outside or in a well-ventilated space for at least 24 hours before wearing or storing them.
• Check your household chemicals as well — If you have household degreasers, adhesive removers, or stain removers that list “perchloroethylene,” “tetrachloroethylene,” or “PCE” on the label, get rid of them immediately. Every change you make — no matter how small — reduces the chemical load your liver has to process each day.
• Beware of other liver-damaging “forever chemicals,” too — In particular, exposure to polyfluoroalkyl or perfluoroalkyl chemicals (PFAS), which include PFOA and PFOS, has been associated with fatty liver disease. When these endocrine-disrupting chemicals accumulate in the liver tissues, they can accelerate metabolic changes that lead to fatty liver. Read more about it in “Toxic To-Go Containers Linked to Liver Disease.”
More Strategies to Protect Your Liver Health
Your liver is one of the largest and most vital organs in the body. It performs more than 500 vital functions, such as detoxification, energy regulation, bile production, nutrient storage, immune function, and more. Many of these processes take place simultaneously.14
Everything you eat, drink, breathe, and absorb through your skin eventually passes through the liver for evaluation and processing. Without its continuous work, your body’s internal balance, from metabolism to immunity, would unravel in a matter of days. Hence, it’s only prudent to take extra steps to keep it well-functioning. In addition to avoiding PCE, below are additional strategies to keep your liver healthy and thriving.
• Eliminate linoleic acid (LA) and alcohol from your diet — Consuming processed and junk foods loaded with soybean, canola, corn, or anything labeled “vegetable oil,” puts your liver under constant assault. Industrial seed oils are loaded with LA, which is metabolized into toxic byproducts called oxidized linoleic acid metabolites (OXLAMs). These are unstable, highly damaging molecules that disrupt cell membranes and set off chronic inflammation.
Meanwhile, alcohol is converted to acetaldehyde, a reactive aldehyde that interferes with your liver’s ability to detoxify, regenerate, and store energy. If you already have belly fat, insulin resistance, or elevated liver enzymes, it’s vital to cut out both seed oils and alcohol to give your liver a chance to heal.
• Prioritize choline-rich foods — Studies have shown that choline deficiency directly contributes to fatty liver disease and that restoring adequate levels helps reverse fat accumulation.15 The best food sources are pastured egg yolks (look for low-PUFA eggs) and grass fed beef liver.
• Maintain a healthy weight — Studies show that waist circumference is a stronger predictor of liver health than weight alone. Keeping your waistline in check and maintaining a healthy weight through a combination of a healthy diet and regular physical activity helps ease the pressure on your liver.16
• Be physically active — Incorporating movement in your life is linked to lower levels of liver enzymes, which are a key marker of liver damage and dysfunction. Taking short walks, even just 10 to 15 minutes after meals, helps lower blood sugar spikes, easing the metabolic load on your liver.
• Get adequate high-quality sleep — Maintain a consistent bedtime routine so you can get adequate, high-quality sleep at night. Getting enough rest at night allows your liver to repair and detoxify. It’s also important to get early morning sunlight to reset your circadian rhythm. Check out my top sleep tips for more strategies to get a good night’s sleep.
For a more comprehensive guide to maintaining a healthy liver, especially as you grow old, read “How to Keep Your Liver Healthy in Your 50s and Beyond.” It provides lifestyle and dietary strategies, along with evidence-based supplementation, that will help your liver stay resilient as you age.
Frequently Asked Questions (FAQs) About Tetrachloroethylene (PCE) and Liver Damage
Q: What is tetrachloroethylene (PCE) and where is it found?
A: Tetrachloroethylene, also known as perchloroethylene (PCE) or ethylene tetrachloride, is a colorless chemical commonly used in dry cleaning, metal degreasing, and some household cleaning products. It’s released into the air from freshly dry-cleaned clothes and can contaminate drinking water through spills or improper disposal that seep into soil and groundwater.
Q: How does PCE exposure affect your liver?
A: Exposure to PCE damages liver cells, leading to a condition called liver fibrosis, a buildup of scar tissue that disrupts the liver’s ability to filter toxins and regulate metabolism. Studies show that even small increases in PCE levels in the blood raise the risk of liver fibrosis significantly, even in people who don’t drink alcohol or have other common liver disease risk factors.
Q: What other health problems are linked to PCE exposure?
A: In addition to liver damage, PCE exposure affects the nervous system, kidneys, and reproductive organs. It’s been associated with dizziness, headaches, confusion, nerve injury, heart rhythm problems, and reduced fertility. Long-term exposure is also linked to several cancers, including bladder, liver, and lymphatic cancers.
Q: How can you limit your exposure to PCE?
A: To reduce your risk, switch from traditional dry cleaning to wet-cleaning or CO₂-based methods. Air out dry-cleaned clothing outdoors before wearing or storing it. Check household products like degreasers and stain removers — if they list “perchloroethylene” or “tetrachloroethylene,” replace them with safer alternatives.
Q: What are the best ways to protect and support your liver naturally?
A: You can protect your liver by eliminating alcohol and seed oils from your diet, as both add extra toxic stress. Eat choline-rich foods like pastured egg yolks and grass fed beef liver, get daily sunlight to support cellular energy production, and stay active with short walks after meals. These habits help your liver repair, detoxify, and maintain long-term health.
- 1 Liver International, November 2025, Volume 45, Issue 11, e70398
- 2, 4, 7, 9, 11, 13 News-Medical.net, October 23, 2025
- 3 Alpha Digestive and Liver Centre, Liver Fibrosis/Cirrhosis
- 5 Keck Medicine of USC, October 23, 2025
- 6, 12 NJ Health, Hazardous Substance Fact Sheet
- 8, 10 Agency for Toxic Substances and Disease Registry, May 26, 2023
- 14 Johns Hopkins Medicine, 5 Ways to Be Kind to Your Liver
- 15 Int. J. Mol. Sci. 2025, 26(15), 7159
- 16 Medscape, August 6, 2025
Types of Medications That Harm Your Kidneys
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/28/medications-that-damage-kidneys.aspx
Analysis by Dr. Joseph Mercola July 28, 2025

Story at-a-glance
- Common medications like NSAIDs, antibiotics, acid blockers, and laxatives quietly damage your kidneys, even when used as directed
- Kidney symptoms often show up late, so damage is underway before you feel anything, especially if you’re older or taking multiple prescriptions
- NSAIDs reduce blood flow, antibiotics clog, or inflame kidney filters and proton pump inhibitors trigger immune reactions that harm kidney tissue
- Imaging contrast dyes used in CT or MRI scans sharply reduce kidney function in vulnerable people, particularly those with diabetes or dehydration
- Reviewing your medications regularly, leading a healthy lifestyle and using natural alternatives help reduce your kidney burden and prevent long-term harm
Kidney damage doesn’t always start with disease — it often starts with prescriptions. Many of the medications you’ve been told are safe are filtered through your kidneys, creating a constant workload that backfires over time. As drug use climbs, so does the hidden toll on this key organ.
Your kidneys handle far more than waste. They help balance fluids, regulate blood pressure, and support red blood cell production. But the more medications your body has to process, the more strain your kidneys are under, especially if you’re older, managing chronic illness, or taking multiple prescriptions.
Most people don’t think to question their medications until something goes wrong. But when kidney function declines, the signs often show up late, after the real damage has been done. That’s why catching the risk early matters. Let’s break down which drug classes pose the greatest kidney risks — and what to do to stay protected.
NSAIDs and Other Painkillers Are Tough on Your Kidneys
An article, published by AARP, highlighted how widely used medications, including both over-the-counter (OTC) and prescription drugs, damage your kidneys even when taken as directed.1 The most vulnerable include older adults, people with diabetes, and anyone who’s dehydrated or managing other illnesses. However, even people without diagnosed kidney issues are at risk if they take multiple medications or ignore dosage guidelines.
• Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce blood flow to your kidneys — Drugs like ibuprofen and naproxen, often used to relieve pain, inflammation, or fever, work by blocking enzymes that cause inflammation. But they also reduce a hormone that keeps the blood vessels in your kidneys open. Without enough of that hormone, these vessels narrow, making it harder for blood to flow in. This leads to reduced kidney function, especially during illness or if you’re dehydrated.
• Don’t take them for too long — Clinical pharmacist Derek Owen, with the University of Chicago Department of Medicine, told AARP that NSAIDs shouldn’t be taken for more than 10 days in a row for pain, or more than three days for fever. These drugs seem harmless because they’re sold over the counter, but regular or prolonged use does real damage.
• Taking NSAIDs with blood pressure and water pills is dangerous — When NSAIDs are combined with ACE inhibitors (for blood pressure) and diuretics (to reduce swelling or fluid buildup), your kidneys are hit from multiple angles. This combination reduces blood flow and filtration pressure, leading to a dangerous drop in kidney function — often without early symptoms. It’s called the “triple whammy” for a reason.
• Get simple tests to check your kidneys — Your doctor can run basic lab tests to measure how well your kidneys are filtering waste and whether they’re leaking protein. Catching small changes early helps you adjust your medications before permanent damage occurs.
Antibiotics, Antivirals, and Immunosuppressants Are Powerful Drugs with Hidden Risks
Antibiotics, antivirals, and immunosuppressants come with serious risks for your kidneys. Even when taken as prescribed, these medications disrupt filtration, block urine flow or cause direct damage if not carefully managed.2
• Some antibiotics damage kidney cells directly — Drugs like tobramycin are especially hard on your kidneys. They build up inside the tiny filtering cells and cause structural damage. The longer these antibiotics are used, the greater the risk, which is why they’re usually only given in short courses under close supervision.
• Others block urine flow — Sulfonamides, another type of antibiotic, form crystals that don’t dissolve well in urine. If you’re dehydrated or your urine flow is slow, these crystals clog the tiny tubes in your kidneys, leading to inflammation, back pressure, and pain. Even if you don’t notice right away, your creatinine levels could start creeping up — a warning sign that filtration is slowing down.
• Doses need to match how well your kidneys are working — If your kidneys aren’t filtering properly and the dose isn’t adjusted, drugs like amoxicillin and ciprofloxacin build up and become harmful. In some cases, they even cause an allergic reaction in the kidneys, leading to swelling and more damage.3
• HIV and transplant drugs also harm your kidneys — Medications like tenofovir for HIV and cyclosporine to prevent organ rejection reduce blood flow in the kidneys and damage the same cells that handle waste removal. People taking these drugs are often on complex medication regimens, making it even more important to track kidney labs regularly.4

Save This Article for Later – Get the PDF Now
Proton Pump Inhibitors and Other Acid Suppressants Are Quiet Contributors to Chronic Kidney Trouble
Proton pump inhibitors (PPIs), such as omeprazole (Prilosec), esomeprazole (Nexium) and lansoprazole (Prevacid), are widely used to reduce stomach acid. They’re commonly taken for heartburn, indigestion, or ulcers, sometimes for years. But long-term PPI use is linked to chronic kidney disease.5
• They inflame your kidney’s filters — PPIs are associated with a condition called interstitial nephritis, an allergic-type reaction that causes swelling in the spaces between kidney structures. This leads to fatigue, swelling in your legs, and darker urine. Because the symptoms are sometimes mild or vague, they often go unnoticed until serious damage has occurred.
• People often stay on these drugs too long — Many start taking PPIs for temporary symptoms but never stop. If you’re using PPIs, taper off slowly and switch to famotidine (Pepcid), a safer option that not only avoids PPI-related heart risks but also helps block excess serotonin that disrupts energy and drives inflammation.
• Lifestyle changes often replace the need for acid blockers — Low stomach acid — not high — is often the actual problem behind acid reflux. The solution isn’t just symptom relief with drugs. It’s optimizing your mitochondrial function to restore the foundation that helps your stomach break down food, absorb nutrients, and protect you from pathogens.
Laxatives Seem Harmless but Quietly Hurt Your Kidneys
Stimulant laxatives like senna and osmotic types like Miralax work by pulling water into your intestines or speeding up how fast things move through your gut. But if you’re not drinking enough fluids — or if you use these products regularly — you lose too much water. That drop in body fluid also reduces blood flow to your kidneys, making it harder for them to do their job.6
• Long-term use often leads to kidney stones — When you’re dehydrated, your urine becomes more concentrated with minerals like calcium and oxalate. Over time, these minerals form crystals and turn into kidney stones. These stones often block urine flow, cause pain and damage the kidneys further if not treated.
• Frequent laxative use is more common than you think — Many people use laxatives several times a week, or even daily, without realizing it could be hurting their kidneys. This is especially true for older adults who are already prone to dehydration or who are on other medications that affect kidney function.
• There are safer, natural ways to manage constipation — Instead of relying on laxatives, try focusing on your gut health and increasing your intake of fiber-rich foods like fruit and vegetables. Drinking more water and moving your body daily also support regular bowel movements.
• Ask your doctor about safer options — If you feel like you can’t go without laxatives, talk to your integrative health care provider. You could have an underlying issue, like low stomach acid, a sluggish thyroid or imbalanced gut bacteria, that’s better off fixed naturally, without risking damage to your kidneys.
Imaging Contrast Dyes Overload Your Kidneys
Doctors often use contrast dyes during CT or MRI scans. These dyes highlight organs and blood vessels, but they also pass through your kidneys. In some people, especially those with diabetes, heart disease or reduced kidney function, these dyes reduce blood flow and damage the filters inside the kidneys.7
• Iodine-based contrast from CT scans trigger acute kidney problems — Some contrast agents contain iodine, which your kidneys have to filter out. In people with existing kidney concerns, this sudden workload leads to contrast-induced nephropathy, a condition where kidney function drops sharply within 48 hours of the scan.
• MRI dyes carry a different kind of risk — Gadolinium-based contrast dyes, used in MRI scans, have been linked to a rare condition called nephrogenic systemic fibrosis. This causes thickening of the skin and connective tissue, mainly in people with severely impaired kidney function.
• The risks go up if you’re sick or dehydrated — If you have a chronic illness, are already taking multiple medications or haven’t been drinking enough fluids, your kidneys could be too stressed to handle the extra load from imaging dyes. The effects don’t always show up right away but are often long-lasting.
How to Protect Your Kidneys
If you’re managing chronic pain, blood pressure, reflux, or inflammation with multiple medications, your kidneys are bearing the brunt, not because they’re weak, but because they’re forced to filter and excrete drug residues day after day. What starts as temporary relief quietly becomes permanent dependence, especially when no one revisits the original reason the drug was prescribed.
Breaking that cycle doesn’t begin with another pill. It starts by restoring your body’s own ability to function. Here’s how to take the pressure off your kidneys and reclaim control over your health:
1. Revisit the original reason for each drug — Was it for a short-term issue like post-surgery pain or an infection? Many people stay on medications for years simply because no one rechecked whether they still need them. If the root cause has resolved, the drug is likely doing more harm than good.
2. Watch for warning signs your kidneys are under strain — Fatigue, fluid retention, back pain, changes in urination, or brain fog all point to sluggish kidney function, especially if you’re on multiple medications. These symptoms are often dismissed as “just aging,” but they’re often your body’s early alert system. Don’t ignore them.
3. Support the systems that make medication unnecessary — Chronic symptoms like fatigue, bloating, reflux, or joint pain are often signs of deeper imbalances. Focus on restoring your body’s energy production, improving mitochondrial health, eating nutrient-dense carbs and avoiding vegetable oils that disrupt metabolism. As health improves, medications become easier to taper.
4. Switch out harmful drugs for safer strategies — NSAIDs damage kidney tissues over time but topical magnesium, turmeric, or gentle exercise offer relief without the risk. Acid blockers reduce stomach acid, but the real cause of reflux, for most people, is low stomach acid, not too much of it; switching to digestive bitters before meals to signal your body to start acid production could ease symptoms without long-term harm.
5. Make a medication review part of your routine — Set a calendar reminder every six months to review your medications with your doctor. Ask one powerful question: “Is this fixing the problem — or just covering up symptoms?” That single shift in thinking could help protect your kidneys for years to come.
When your treatment plan aligns with your biology — instead of working against it — most medications become optional, not mandatory. That’s the path to true healing and long-term kidney protection.
FAQs About Medications That Harm Your Kidneys
Q: Which types of medications are most likely to harm my kidneys over time?
A: Common culprits include NSAIDs (like ibuprofen and naproxen), antibiotics (such as tobramycin and sulfonamides), acid blockers (especially PPIs like omeprazole), certain antivirals, and immunosuppressants (like tenofovir and cyclosporine), laxatives and imaging contrast dyes. These drugs reduce kidney blood flow, cause inflammation, or block urine filtration, often without obvious symptoms at first.
Q: Why don’t most people realize their kidneys are being damaged by medications?
A: Kidney damage typically develops slowly and symptoms often appear late. Early signs, like fatigue, swelling, changes in urination or brain fog, are frequently mistaken for aging or other conditions. Without routine lab tests, many people remain unaware until permanent damage is done.
Q: How do NSAIDs and acid blockers affect kidney function?
A: NSAIDs reduce a hormone that keeps kidney blood vessels open, leading to restricted flow and lower filtration, especially during illness or dehydration. PPIs cause an inflammatory reaction in kidney tissues known as interstitial nephritis and are also linked to chronic kidney disease with long-term use.
Q: Does using laxatives or undergoing medical scans also affect kidney health?
A: Yes. Overuse of laxatives cause dehydration and kidney stone formation, while contrast dyes used in CT and MRI scans reduce kidney function, particularly in people with preexisting conditions or poor hydration. Both scenarios increase your risk of long-term kidney damage if not managed carefully.
Q: How do I protect my kidneys if I use these medications?
A: Start by reviewing each drug’s original purpose to see if it’s still necessary. Also watch for signs of kidney stress while supporting your body’s natural healing systems through diet and lifestyle. Taper off unnecessary medications and explore safer nondrug alternatives. Set a six-month reminder to review all prescriptions regularly.
Could Low Testosterone Be Secretly Driving Your Kidney Stone Risk?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/06/04/low-testosterone-kidney-stones-risk.aspx
Analysis by Dr. Joseph Mercola June 04, 2025

Story at-a-glance
- Low testosterone levels below 3.33 ng/mL increase kidney stone risk by 65%, regardless of other health factors like age, weight, or blood pressure
- Men aged 34 to 44 years old with low testosterone face a 29% higher risk of developing their first kidney stone compared to those with normal levels
- Maintaining testosterone above 360 ng/dL significantly reduces kidney stone risk, with protective benefits most pronounced in men over 40 years old
- Testosterone influences kidney stone formation possibly by affecting glycolate oxidase production, which catalyzes metabolites involved in stone development
- Natural ways to boost testosterone include reducing exposure to endocrine-disrupting chemicals, KAATSU training, optimizing diet, sunlight exposure, and balancing hormones with progesterone
Kidney stones form when substances like calcium oxalate, struvite, and uric acid crystallize in your urinary tract,1 often resulting from hormonal imbalances or metabolic disturbances.
Left untreated, kidney stones not only cause severe discomfort, but also trigger urinary tract infections (UTIs) and obstruct urine flow that eventually lead to kidney damage. Now, researchers have identified one significant risk factor linked to their formation — low testosterone levels.
Your Testosterone Levels Predict Kidney Stone Risk
In a study published in the International Journal of Impotence Research (IJIR), researchers examined how low testosterone affects your likelihood of developing kidney stones, especially as you age.2
The team followed 3,234 healthy adult males (primarily middle-aged) participating in health screenings over a 10-year period, specifically from 2010 to 2020. Each of them was tested for total testosterone along with scans to detect kidney stones, allowing researchers to analyze the relationship between the two variables.
• There is a threshold where kidney stone risk is dramatically increased — Findings revealed that once your testosterone levels drop below 3.33 ng/mL (nanograms per milliliter), the risk of kidney stones spikes by approximately 65% compared to men whose hormone levels remain within a normal range. Furthermore, this was regardless of age, body weight, cholesterol levels, or blood pressure.
This means that even if you’re otherwise healthy and physically fit, having low testosterone is already enough to put you at risk for kidney stones. As noted in the study, “low serum testosterone levels (<3.33 ng/mL) were significantly and independently related to kidney stones in men.”
• Other common factors ceased to be important — Low testosterone alone is uniquely capable of influencing kidney stone formation compared to other typical health biomarkers, such as blood pressure or cholesterol levels.
• Age impacts risk more than others — The strongest increase in kidney stone risk occurred among participants who exhibited the lowest testosterone levels coupled with older age. Specifically, the study found a pronounced jump among men over 50 who were simultaneously struggling with severely low testosterone.
The takeaway here is that older men, already naturally prone to hormonal decline, will benefit greatly by managing their testosterone to prevent kidney stone issues from complicating their health down the road.
The Link Between Age and Testosterone-Related Kidney Stones
In an earlier study, also published in IJIR, researchers explored how age influences the relationship between testosterone levels and kidney stone formation. They tested whether the risk of developing kidney stones associated with low testosterone changes across different age groups in men not using testosterone replacement therapy (TRT).3
The researchers combed through electronic health records and eventually selected 263,557 men across multiple health care institutions in the United States. All participants had documented testosterone levels below 300 ng/dL (nanograms per deciliter) and had never undergone TRT. This allowed the team to analyze the natural relationship between untreated low testosterone and kidney stone risk across various age groups.
• The impact of age — This factor (alongside low testosterone) dramatically affects your kidney stone risk. While young men between 18 and 24 years old with low testosterone showed virtually no increased risk, it climbed steadily with age.
Meanwhile, men aged 34 to 44 years old experienced the most significant spike, with a 29% greater likelihood of developing their first kidney stone compared to men with normal testosterone levels in this same group.
• Testosterone declines as you age — In relation to the point above, the study pinpointed how risk varied across different age groups. Younger adults, surprisingly, did not seem immediately vulnerable, which indicates hormonal influences likely require prolonged interaction with other factors to trigger kidney stone formation.
As you approach middle age, however, the body’s declining hormone levels begin to amplify the vulnerabilities.
• The risk plateaus past a certain age — Another notable discovery was how the danger for kidney stones declined again as men reached older ages. Although still elevated, the increased likelihood diminished somewhat among men over 55 years old.
Researchers theorize that this action occurs because older men often have other competing health factors or lifestyle changes that overshadow testosterone’s direct impact, making age-specific awareness particularly valuable if you’re currently navigating your mid-30s to early 50s.
• How kidney stones form isn’t still known — According to the authors, there’s no solid research explaining the formation of kidney stones. However, they are certain that men are “two times more likely than women to develop a kidney stone.”4

Save This Article for Later – Get the PDF Now
The Testosterone Threshold Leading to Kidney Stones
In a study published in Frontiers in Endocrinology, researchers investigated the range wherein testosterone levels influence kidney stone risks for men. They used a nationwide dataset database involving 6,633 adult males to define the range associated with the lowest likelihood of kidney stone formation.5
The researchers focused exclusively on adult men without preexisting hormonal therapies or prior kidney stones. From there, the analysis revealed a clear number — maintaining testosterone levels above approximately 360 to 422 ng/dL sharply reduces kidney stone risk. Conversely, dropping below this range will be bad for your health.
• The link between testosterone and kidney stones is clear — The authors divided testosterone measurements into four quartiles, effectively categorizing men into groups (lowest to highest hormone levels). Men with testosterone levels above 360 ng/dL — those in the highest quartile — experienced a significantly lower likelihood of developing kidney stones.
In contrast, men in the lowest testosterone group faced a nearly 47% increased risk compared to those whose levels exceeded the mentioned cutoff point.
• The protective benefits of higher testosterone are not evenly spread — Younger men between 20 and 40 years old did not see significant changes in kidney stone risk related to their testosterone levels.
Instead, the protection became most pronounced in men over the age of 40. Within this group, men whose testosterone remained above the 360 ng/dL threshold enjoyed the greatest advantage, highlighting that managing testosterone effectively in middle age significantly reduces your long-term kidney health risks.
• Testosterone’s effects on other common factors — The findings emphasize that while obesity and poor diet independently increase your risk for kidney stones, having low testosterone compounds these problems considerably. Other factors that interact with low testosterone include vascular disease, Type 2 diabetes, and osteoporosis.
Maintaining optimal testosterone levels supports your body’s metabolic health, making it easier to regulate body weight, which, as mentioned earlier, is a risk factor for stone prevention. To add, men with healthy testosterone levels typically have fewer metabolic disturbances, translating into fewer kidney-related complications down the road.
• A theory on how stones form — In previously published literature cited by the researchers,6,7 they noted that testosterone influences the production of glycolate oxidase, a liver enzyme that catalyzes “glycolate to glyoxylate and glyoxylate to oxalate, a key metabolite in kidney stone formation.”8 However, this is just an educated inference:
“As far as we know, the rat ethylene glycol model of urolithiasis relies on artificial mechanisms that are not comparable with the pathophysiology of naturally occurring stone disease in humans … However, in natural human stone formation, no evidence exists to show that stones form secondary to oxalate-induced renal injury and calcium oxalate crystals are deposited in the renal interstitium.”9
Natural Ways to Raise Your Testosterone Levels
After examining the research, one finding is clear — your testosterone levels influence your risk for developing kidney stones. Considering this, it’s important to be aware of the signs of low testosterone, such as fatigue, reduced libido, loss of muscle mass, and mood swings.
I recommend that you have your blood tested.10 Now, what’s a healthy range? In a previous article, I mentioned 300 to 1,000 ng/dL as a baseline. Having said that, how do you begin to raise your testosterone? In the video above, I share nine tips you can implement right away. Additional strategies are outlined below:
1. Reduce exposure to endocrine-disrupting chemicals (EDCs) — Your first step is to minimize your exposure to chemicals known to disrupt hormones, which are commonly found in plastics, nonstick cookware, personal care products, and pesticides.
Switch to glass or stainless steel containers instead of plastic, choose organic, sustainably produced food as often as you can, and look for personal care products labeled “paraben-free” and “phthalate-free.”
2. Start KAATSU training for hormonal balance — If you’re unsure where to begin exercising, I recommend KAATSU training. This approach temporarily restricts blood flow with specially designed bands, stimulating muscle growth and testosterone production without over-stressing your joints or muscles.11
3. Consider taking a niacinamide supplement — Also known as nicotinamide, this nutrient is important for optimal mitochondrial function. Moreover, research has shown that increasing intake helps with issues related to declining testosterone levels.12 In light of this, I recommend taking this combination for maximum effect:
- 50 milligrams (mg) three times a day
- 5 mg to 10 mg of DHEA orally once a day
- 50 mg of pregnenolone once a day
4. Prioritize sunlight exposure — Sun exposure does far more than boost vitamin D levels. It directly enhances your cellular energy health, a foundational step in supporting testosterone levels and even overall health. As noted in a study published in Cureus, vitamin D influences calcium balance. Moreover, participants with low vitamin D levels have also been found to have low testosterone levels.13
For optimal results, it’s important you get around one hour of exposure during solar noon (12 noon or 1 p.m.) during daylight savings time. However, there’s one caveat to this recommendation.
If you’ve been eating a diet high in linoleic acid (LA), you’ll need to avoid sunlight during peak hours (usually an hour before and after solar noon) for two to six months while following a low-LA diet. It usually takes two to three years to remove most of the LA in your skin, but there is a way to speed up the process.
5. Add raw, grass fed milk to your diet — I’ve recently discovered that C15:0, a special fat found in raw milk, helps flush out LA than just following a low-LA diet.
Specifically, increasing your C15:0 intake to 2 grams per day allows the keratinocytes in your skin to incorporate this healthy fat instead of LA within four weeks. This means that if you continue with this approach, the total LA should go down by 25% to 30% within three to four months.
When you keep it up for 12 to 18 months, the LA in your adipose tissue will go down by 80%. After doing this, whatever remaining ultraviolet risks on your skin come from direct DNA damage and can’t be fixed by your diet.
6. Incorporate a natural anti-estrogen like progesterone — Testosterone and estrogen must remain balanced to ensure optimal health, especially if you’re a middle-aged man experiencing hormonal shifts. In this case, progesterone is a natural hormone that safely counteracts excessive estrogen buildup. To administer it correctly, read the following sections.
Frequently Asked Questions (FAQs) About Testosterone and Kidney Stones
Q: What causes kidney stones and how are they linked to testosterone?
A: Kidney stones form when substances like calcium oxalate crystallize in the urinary tract. While the exact process is unknown, studies show a strong link between low testosterone levels and an increased risk of developing kidney stones. Specifically, testosterone levels below approximately 360 ng/dL significantly raise the risk.
Q: Does age affect how testosterone influences kidney stone risk?
A: Yes, age greatly impacts the relationship between testosterone and kidney stone risk. Men under 30 years old typically see less immediate risk from low testosterone, while middle-aged men (ages 34 to 55 years old) experience a dramatic increase in kidney stone risk if their testosterone is low. Interestingly, after age 55, the risk plateaus slightly, though it remains elevated.
Q: Can maintaining normal testosterone levels protect against kidney stones?
A: Maintaining testosterone levels at approximately 360 ng/dL can significantly reduce kidney stone risk, particularly for men over 40. Research identifies this as a safe threshold.
Q: How does testosterone interact with other kidney stone risk factors?
A: Low testosterone exacerbates the effects of other conditions like obesity, diabetes, and metabolic syndrome — each already known to increase kidney stone risk. Men experiencing both low testosterone and one of these conditions face a substantially higher risk than those with just one issue alone.
Q: Are there natural methods to boost testosterone and reduce kidney stone risk?
A: Yes. Natural ways to boost testosterone and lower kidney stone risk include reducing exposure to EDCs (found in plastics and pesticides), practicing blood-flow-restriction exercises (KAATSU training), prioritizing safe sunlight exposure, and balancing estrogen levels naturally, such as with progesterone.
- 1 Mayo Clinic, “Kidney Stones”
- 2 Int J Impot Res (2025)
- 3, 4 Int J Impot Res (2024)
- 5, 9 Front Endocrinol (Lausanne). 2022 May 2;13:863675
- 6 J Urol. 2001 Sep;166(3):1078-82
- 7 J Am Soc Nephrol. 1999 Nov:10 Suppl 14:S376-80
- 8 Biochemistry. 2008 Jan 24;47(8):2439–2449
- 10 Cleveland Clinic, “Testosterone Test”
- 11 J Int Med Res. 2021 Sep; 49(9): 03000605211039564
- 12 Nature Aging 2022; 2: 105-114
- 13 Cureus. 2023 Sep 24;15(9):e45856
Bay Leaves Help Lower Blood Sugar and Improve Cholesterol Levels
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/05/19/bay-leaves-lowering-blood-sugar.aspx
Analysis by Dr. Joseph Mercola May 19, 2025
Story at-a-glance
- According to research, consuming as little as 1 gram of bay leaves daily can lower fasting glucose by up to 26% and reduces LDL cholesterol by 40%, offering natural support for metabolic health
- Insulin sensitivity improves with regular bay leaf intake, as studies show it protects pancreatic beta cells and enhances the body’s ability to regulate blood sugar
- Liver and kidney function benefit from bay leaf extract, which reduces inflammation, improves enzyme balance, and prevents diabetes-related organ damage
- Powerful antioxidants in bay leaves fight oxidative stress and inflammation, lowering the risk of metabolic dysfunction, heart disease, and complications linked to diabetes
- Try adding bay leaves to your meals, brewing them into tea, or using them in powdered form to provide an easy, natural way to regulate blood sugar and improve overall health
Bay leaves (Laurus nobilis L.) have been a staple in traditional medicine and cooking for centuries, but modern research now reveals something far more important about this common herb. Studies show that bay leaves significantly lower blood sugar levels and improve cholesterol, making them a powerful tool for managing your metabolic health.
Bay leaves also contain beneficial compounds that help protect cells from oxidative stress, which is one of the key drivers of inflammation and chronic disease. This ability to support both glucose metabolism and lipid balance makes them an overlooked but valuable addition to a health-conscious diet.
Bay Leaves Protect Your Organs While Lowering Blood Sugar
A 2021 animal study published in the Annals of Medicine and Surgery journal1 examined how bay leaf helps mitigate the damage caused by diabetes, particularly in the pancreas, liver and kidneys — organs that are often severely affected by the disease. Over four weeks, diabetic rats were given bay leaf extract, and their blood sugar levels, insulin response and organ function were closely monitored.
- Bay leaf extract led to a significant drop in blood sugar — The rats that received the bay leaf extract experienced a significant drop in blood sugar, bringing their glucose levels much closer to normal compared to diabetic rats that received no treatment.
- Pancreatic beta cells were better preserved — These cells are responsible for producing insulin. In untreated diabetic rats, these insulin-producing cells were severely damaged, leading to insulin dysfunction and uncontrolled blood sugar. In contrast, rats that received bay leaf extract showed stronger insulin production and healthier pancreatic tissue.
- Untreated diabetic rats had severe liver damage — The liver, which helps regulate glucose and lipid metabolism, often becomes inflamed and overloaded with fat in diabetics. The researchers found that rats that didn’t receive bay leaf extract had liver necrosis (cell death), fatty deposits and structural degeneration.
- Bay leaf extract-treated rats had improved liver function — Their liver enzyme (AST, ALT, and GGT) levels, key markers of liver function, improved significantly, suggesting reduced liver stress and better overall metabolic control. Liver enzymes are critical for detoxification and metabolic health, and when elevated, it means the liver is under strain. Bay leaf-treated rats had levels that were closer to those of healthy rats.
- Remarkable improvements were also seen in kidney function — Diabetes causes kidney damage due to high blood sugar and inflammation, often resulting in diabetic nephropathy. In this study, untreated diabetic rats had kidney damage, inflammation, and abnormal structural changes. Bay leaf extract prevented much of the damage, helping reduce cellular stress and maintain normal kidney architecture in the treated rats.2
What Makes Bay Leaves So Powerful?
Bay leaves have a positive effect on insulin signaling, which is one of the key mechanisms behind its antidiabetic effects. Insulin is the hormone responsible for moving sugar from the bloodstream into cells, but when you have diabetes, your cells become resistant to insulin’s effects.
- Bay leaves improve insulin signaling — In the animal study above, bay leaf extract was found to enhance insulin sensitivity. This leads to lower blood sugar levels and improves glucose metabolism, key factors in preventing long-term complications of diabetes.
- Potent antioxidants in bay leaves — 1,8-cineole, α-terpinyl acetate and linalool in bay leaves help reduce oxidative stress, which is a major driver of diabetic complications. High blood sugar generates free radicals, unstable molecules that damage cells and accelerate disease progression. Bay leaf’s potent antioxidants help neutralize free radicals.
- Bioactive compounds in bay leaves help regulate lipid metabolism — In diabetes, cholesterol and triglyceride levels often become dangerously unbalanced, increasing the risk of heart disease. The study showed that rats treated with bay leaf extract had better lipid profiles (reduced LDL cholesterol and triglycerides and increased HDL cholesterol), which helped support heart health and overall metabolic stability.
This research provides compelling evidence that bay leaves are more than just a spice — they’re a powerful tool for metabolic health. “We believe that further preclinical research into the utility of L. nobilis treatment may indicate its suitability as a potential treatment in diabetic patients,” the study authors wrote.3

Save This Article for Later – Get the PDF Now
Human Research Confirms Results
Previous research has demonstrated these effects in humans as well. A study published in the Journal of Clinical Biochemistry and Nutrition4 examined the effects of bay leaf consumption on blood sugar and cholesterol levels in Type 2 diabetics. Their primary goal was to determine whether bay leaves could naturally help control glucose levels and improve lipid profiles in people who are at risk of diabetes and heart disease.
- Different bay leaf doses were tested over a 30-day period — The study involved 40 participants, all diagnosed with Type 2 diabetes. They were divided into four groups, each receiving a different amount of bay leaves (1, 2 or 3 grams of ground bay leaves in capsule form) or a placebo. After just 10 days, significant changes were already evident in the groups taking bay leaves, and more significant improvements were seen after 30 days.
- Bay leaves help regulate glucose more effectively over time — Participants consuming bay leaves saw fasting blood sugar levels drop by 21% to 26%, with the most significant reductions occurring in those taking 1 or 3 grams daily. Even more interesting, these lower blood sugar levels persisted for 10 days after stopping bay leaf consumption, indicating a lasting effect.
- Cholesterol levels also saw major improvements — Across all bay leaf groups, total cholesterol levels dropped between 20% and 24%, with the biggest reductions seen in LDL cholesterol (“bad” cholesterol). LDL levels plummeted by as much as 40%, a decrease that rivals the effects of some cholesterol-lowering medications.
- Triglycerides decreased significantly — In the 1-gram group, triglycerides dropped by 34%, while the 2-gram group saw a 25% reduction. Even after stopping bay leaf consumption, their levels remained lower than before the study, reinforcing the long-term benefits.
- HDL cholesterol levels soared — The researchers found that HDL “good” cholesterol rose by 19% to 29%, improving participants’ overall heart health. This shift in cholesterol ratios is crucial, as high LDL and low HDL levels are key drivers of heart disease, stroke and other cardiovascular problems.
The researchers noted that none of the participants were taking insulin, and they all continued their usual diabetes medications and diets during the study. This setup allowed them to identify how bay leaves affected the diabetics’ health beyond the effects of their existing treatments.
Another interesting aspect is that the most notable benefits were observed in the 1-gram group. They had the most consistent improvements across blood sugar, cholesterol, and triglycerides. This suggests that even a small daily amount of bay leaves provides meaningful health benefits, making it easy to incorporate into a regular diet.5
What Else Is Bay Leaf Good For?
Bay leaves are an excellent source of vitamins A and C, iron, manganese, copper and calcium — all of these are antioxidants with free radical-scavenging abilities, and positively impact your eyesight, bones, blood and more.6 Below are other health benefits associated with bay leaves.
- Pain relief — In traditional medicine, bay leaves are used for alleviating digestive issues, like ulcer pain, heartburn, gas and colic. It’s also helpful in easing arthritis and headaches.7
- Protects against pathogenic bacteria — A study published in the Journal of Pathogen Research tested the antimicrobial and antioxidant properties of bay leaves against multiple bacterial strains, including Staphylococcus aureus, Escherichia coli (E.coli) and Pseudomonas aeruginosa. The results revealed strong antibacterial effects, particularly against S. aureus and E. coli.8
- Bioactive compounds provide immune support — Researchers attribute these effects to the flavonoids (kaempferol, myricetin and quercetin), polyphenols, and essential oils found in bay leaves, which all have well-documented anti-inflammatory and immune-supporting properties.
- Inhibits bacterial growth — The monoterpenes and sesquiterpenes in bay leaves also disrupt bacterial membranes and inhibit their ability to grow and multiply.9
For more interesting trivia on bay leaves and how they benefit your health, read “Are Bay Leaves Good for You?”
How to Add Bay Leaves to Your Diet
If you’re looking for a natural way to improve your blood sugar levels and cholesterol, adding bay leaves to your diet is one of the easiest steps you can take. The best part? You don’t need much. As the studies above demonstrate, even a small amount daily makes a big difference. Here are tips to get the most out of bay leaves and improve your overall health:
1. Use whole bay leaves in cooking — The simplest way to start using bay leaves is to cook with them regularly. Add a couple of whole bay leaves to soups, stews, rice or slow-cooked meats. The leaves will infuse your food with their beneficial compounds while enhancing flavor. Just remember to remove them before serving, as they are not meant to be eaten whole.
2. Brew bay leaf tea — If you prefer a more direct way to consume bay leaves, make a tea by simmering two or three dried bay leaves in hot water for 10 minutes. This allows the active compounds to extract fully. Drink this tea daily to help regulate blood sugar and reduce oxidative stress. You can also add a squeeze of lemon or a teaspoon of raw honey if you want to enhance the taste.
There are other types of tea that are beneficial for diabetics. Learn more about them in my article, “Study Shows Tea Can Reduce Risk and Progression of Diabetes.”
3. Use ground bay leaves for maximum benefits — If you want a more concentrated effect, use ground bay leaves instead of whole ones. Sprinkle a small amount into sauces, curries or even mix it into a smoothie. This method ensures you consume the beneficial compounds directly without having to remove the leaves later.
4. Combine bay leaves with other antioxidant-rich foods — Bay leaves work even better when paired with other antioxidant-rich foods. Since oxidative stress contributes to insulin resistance and cholesterol imbalances, eating more fresh fruits, vegetables, and healthy fats alongside bay leaves further reduces inflammation and protects your cells.
Adding other herbs and spices to your meals gives you even more metabolic support. One example is cinnamon — read more about it in this article, “Cinnamon — An Ancient Spice That May Be Beneficial for Prediabetics.”
5. Be consistent and give it time — The studies on bay leaves showed significant improvements within 30 days, but these benefits are best sustained through long-term use. Make bay leaves a regular part of your meals and be patient as your body gradually improves insulin sensitivity, lowers LDL cholesterol and balances blood sugar levels. Like any natural approach, consistency is key.
Bay leaves offer a simple, natural way to support metabolic health, and incorporating them into your diet requires minimal effort. Whether you add them to your meals, brew them into tea, or use them as a seasoning, they are a powerful tool for improving glucose regulation and protecting your heart.
If you’re struggling with diabetes, there are other herbs and spices that will help manage your blood sugar levels. Read “These Herbs and Spices Can Help Deter Diabetes” for more information.
Frequently Asked Questions (FAQs) About Bay Leaves
Q: How do bay leaves help lower blood sugar?
A: Bay leaves improve insulin sensitivity, allowing the body to use insulin more effectively. This leads to better glucose control and lower fasting blood sugar levels by up to 26%.
Q: Can bay leaves improve cholesterol levels?
A: Yes, studies show bay leaves reduce LDL (“bad”) cholesterol by up to 40% while increasing HDL (“good”) cholesterol by 19% to 29%, supporting heart health and metabolic balance.
Q: How do bay leaves support liver and kidney function?
A: Research found that bay leaf extract reduces liver inflammation, improves enzyme balance, and prevents kidney damage linked to diabetes, helping protect these organs from long-term deterioration.
Q: What is the best way to consume bay leaves for health benefits?
A: You can use whole bay leaves in cooking, brew them into tea, or take them in ground form. Studies suggest 1 to 3 grams daily for optimal metabolic support.
Q: Do bay leaves have other health benefits beyond blood sugar and cholesterol control?
A: Yes, bay leaves contain powerful antioxidants that fight oxidative stress and inflammation, which helps reduce the risk of heart disease, metabolic dysfunction, and bacterial infections.
Study warns: Repeated acetaminophen use may harm heart, kidneys, and gut in seniors
Reproduced from original article:
https://www.naturalhealth365.com/study-warns-repeated-acetaminophen-use-may-harm-heart-kidneys-and-gut-in-seniors.html
News Staff | April 7, 2025
 (NaturalHealth365) That bottle of Tylenol in your medicine cabinet isn’t as innocent as you think. A new study from the University of Nottingham just published in Arthritis Care and Research exposes the truth about acetaminophen.
(NaturalHealth365) That bottle of Tylenol in your medicine cabinet isn’t as innocent as you think. A new study from the University of Nottingham just published in Arthritis Care and Research exposes the truth about acetaminophen.
(LeanMachine edit: In Australia, better known as Panadol, Paracetamol and other names).
For generations, doctors have pushed acetaminophen (also sold as Mapap and Panadol) as the “safe” pain relief option. Meanwhile, this common drug has been silently damaging organs in millions of trusting patients, especially seniors.
Massive 20-year study confirms what natural health experts suspected all along
University researchers analyzed medical records of over half a million people between 1998 and 2018. They compared 180,483 regular acetaminophen users with 402,478 non-users, defining “regular use” as receiving at least two prescriptions within six months.
The results? Absolutely devastating. People taking acetaminophen – particularly those over 65 – showed dramatically higher rates of serious health problems across multiple body systems.
Six ways acetaminophen destroys your body
This isn’t just about minor side effects. Regular acetaminophen users faced significantly increased risks of:
- Hypertension
- Heart failure
- Peptic ulcers
- Peptic ulcer bleeding
- Bleeding in the lower gastrointestinal tract
- Chronic kidney disease
(LeanMachine Edit: The majority of patients on the Liver Transplant Waiting List are there because of Paracetamol / Panadol).
Let that sink in. The pill millions pop without a second thought for headaches and minor pain is linked to kidney failure, heart damage, and dangerous internal bleeding.
Why you haven’t heard this on the evening news
Turn on your TV and count the Tylenol commercials. Check any magazine and spot the acetaminophen ads. Big Pharma spends millions keeping media outlets flush with advertising dollars. Think they’re eager to report on studies that threaten those relationships?
The corporations selling these pills have a vested interest in keeping you in the dark about their products’ true effects. And the mainstream media – dependent on pharmaceutical advertising – isn’t rushing to bite the hand that feeds them.
The toxic reality: How acetaminophen targets vulnerable seniors
What makes these findings particularly alarming is how acetaminophen specifically endangers older adults. As we age, our kidneys naturally lose the energy of our youth, making it harder to clear medications from the bloodstream. This means seniors taking regular acetaminophen doses face a double threat – decreased ability to eliminate the drug combined with increased vulnerability to its toxic effects.
The researchers found the risk of adverse effects rose dramatically with age, with those over 75 showing the most severe outcomes. Even more troubling, many seniors take acetaminophen alongside other medications, creating dangerous interactions that multiply organ damage potential. And since acetaminophen appears in countless combination cold and flu products, many unknowingly take multiple doses daily, pushing their exposure to dangerous levels.
Exploring your options: Natural pain solutions that actually work
Instead of risking your organs with acetaminophen, especially if you’re over 65, consider these safer alternatives:
- Cold compresses and ice packs work wonders for inflammation without side effects
- Regular massage therapy addresses underlying muscle tension and pain
- Acupuncture offers proven relief for many chronic pain conditions
- Kitchen cabinet remedies like turmeric, ginger, and clove oil provide natural anti-inflammatory effects
For severe osteoarthritis that doesn’t respond to these approaches, talk with a doctor who understands holistic medicine rather than one who just pushes pills.
This eye-opening research confirms what natural health advocates have said for years – the quick-fix pills promoted by pharmaceutical giants often create more problems than they solve. As more independent studies reveal these dangers, smart consumers are abandoning acetaminophen for safer, natural pain management approaches.
Sources for this article include:
Research links excessive oxalates to breast cancer
Reproduced from original article:
https://www.naturalhealth365.com/research-links-excessive-oxalates-to-breast-cancer.html
by: February 19, 2025
 (NaturalHealth365) Information about little-known compounds called oxalates can be confusing and conflicting. They are often equated with the “bad” substances in foods, but, in reality, oxalates are neither good nor bad. They can become problematic, however, when too many of them accumulate in the body.
(NaturalHealth365) Information about little-known compounds called oxalates can be confusing and conflicting. They are often equated with the “bad” substances in foods, but, in reality, oxalates are neither good nor bad. They can become problematic, however, when too many of them accumulate in the body.
When there are too many oxalates – they can overwhelm the kidneys and lead to kidney stones and immune deficiency. Furthermore, research indicates that high levels of oxalate in the mammary area have been linked to breast cancer tumor growth as well.
The body itself forms most oxalates
Oxalates (COOH), or oxalic acid, are strongly acidic substances that help plants and animals metabolize. The body’s functions form about 60% to 80% of oxalates. The other 20 to 40% of oxalates come from food.
Most fruits and vegetables contain a small amount of oxalic acid, and they are found in the leaves of plants as opposed to the roots, stalks, and stems. The following foods contain a high amount of oxalates overall:
- Rhubarb
- Chocolate
- Spinach
- Beet greens
- Swiss chard
- Some nuts, especially almonds, cashews, and peanuts
- Some berries, especially gooseberries
- Lemon and lime peel
- Some grains and pasta (except brown rice)
- Some legumes, especially navy beans, black beans, and soybeans
- Okra
- Parsley
How are oxalates linked to breast cancer?
Oxalates are oxidizing substances. As such, they are extremely volatile and can damage tissue in large amounts. Oxalate crystals cause the formation of kidney stones, which can block the flow of urine and lead to kidney infection and bladder cancer.
These crystals are also razor sharp and can cause direct damage and long-lasting inflammation to whatever internal tissues they come into contact with. Oxalate-iron crystals can lead to iron depletion. When calcium-oxalate crystals form, they can lodge in internal organs and bone. As they grow, they crowd out bone marrow, leading to immune deficiency and anemia.
Excess oxalates also can chelate heavy metals. However, oxalates trap metals like mercury and lead in tissues, unlike other chelators. Excess oxalate has been linked to fibromyalgia, vulvodynia (vulvar pain), digestive disorders, and autism.
The most startling new connection between excess oxalates and disease has to do with breast cancer, however. A study conducted by the National University of Cordova in Argentina compared the oxalate levels of breast cancer tumor tissue and regular breast tissue. They found that “all tested breast tumor tissues contain a higher concentration of oxalates than their counterpart non-pathological breast tissue.”
The researchers also discovered that oxalic acid caused tumor proliferation and stimulated the expression of pro-tumor genes. Surprisingly, proliferation did not happen when oxalate was injected into the backs of laboratory mice. This indicates that high oxalate levels do not induce cancer tumor growth in all types of tissue.
Three ways to reduce your oxalate levels
Obtain calcium from natural foods, not calcium supplements.
Calcium has an interesting relationship with oxalates. Approximately 5-15% of the world population will develop some form of kidney stone. Of those, 80% will be calcium-oxalate stones. When calcium is combined with foods that are high in oxalates within the intestines, the two together form an oxalate-calcium crystal that the body cannot absorb.
When this happens, a “stone” is formed that will make its way to the kidneys to eventually be eliminated in the urine. The presence of oxalate-calcium crystals, which can block urine flow and cause kidney infection, can also lead to a higher risk of renal, pelvis, and bladder cancers. These same kinds of crystals can also form in the lungs, nerves, brain, bones, blood vessels, and joints.
Does this mean you should limit calcium intake if you are prone to kidney stones? Not necessarily. Research conducted on vegetarians found that they did not have higher-than-normal rates of calcium deficiency or osteoporosis caused by oxalate interference.
In fact, according to a study published in the European Journal of Epidemiology, vegetarians had a lower rate of kidney stones than meat eaters did. Those who consumed calcium supplements regularly, however, have shown time and again to have higher rates of kidney stones. Calcium supplementation has also been linked to both prostate and breast cancer. Stick to natural and preferably vegetable and fruit-based calcium sources to avoid kidney stones and cancer.
Be aware of your protein intake.
Be cautious about protein, especially if it is derived from meat and dairy. Oxalates are produced from amino acids in the liver.
Amino acids are the building blocks on which proteins are made so some researchers make the connection between total protein amounts and total oxalates formed. For meat-eating women, the general recommendation is around 5 ounces a day. This is equivalent to a small hamburger patty or four eggs. The USDA states that, on average, Americans eat 30% more meat protein than the recommended allowance.
Maintain good intestinal flora.
According to research, some individuals have a physiology prone to higher levels of oxalate uptake in the digestive tract (thus, a higher risk of kidney stones). Although there is evidence to suggest that hereditary disposition plays a role for some people, there is also a strong link between kidney stone formation and disorders of the digestive system, such as inflammatory bowel disease, leaky gut, and Crohn’s.
Could oxalate hyper-absorption have more to do with extreme gut flora imbalance than genetics? The jury is still out on that one. What is known, however, is that it is the job of specific flora, in particular, certain species of Oxalobacter formigenes, Lactobacillus, and Bifidobacteria, to process oxalic acid and prepare it for absorption. Currently, there are several studies underway which focus on the role of oral probiotics in this process.
Let food work for you to keep oxalate levels in balance
Remember that problems only emerge when there is an excess of oxalates in the system. The standard American diet contributes to oxalate overload, but you can also keep it in check by being proactive with prevention. Eating antioxidant-rich food, consuming citrate-rich lemon and lime juice (which experts say can help prevent calcium-oxalate kidney stones), staying hydrated, and watching your salt intake are other ways to keep kidney stones in check.
Also, don’t let the fear of kidney stones prevent you from getting adequate amounts of vitamin C and D. One of the ways that oxalates are formed is through conversion from vitamin C. However, studies thus far have been inclusive as to whether high vitamin C intake actually leads to increased oxalate production.
In regards to vitamin D, deficiency of this vital substance has reached pandemic proportions in the developed world, including among those who have experienced kidney stones. Be sure to get your levels checked the next time you get blood work done. Maintaining a healthy balance of all substances in the body, including oxalates, is the only way to achieve and experience true health naturally.
Sources for this article include:
NIH.gov
NIH.gov
Oxfordjournals.org
MDPI.com
NIH.gov
NIH.gov
NIH.gov
Sciencedaily.com
Scientificamerican.com
Nutrition.org
How DMSO Protects and Heals Internal Organs
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/12/06/dmso-internal-organs.aspx
Analysis by A Midwestern Doctor December 06, 2024

STORY AT-A-GLANCE
- The therapeutic actions of dimethyl sulfoxide (DMSO) make it well suited to treat challenging conditions throughout the body, including many of the internal organs
- DMSO effectively protects organs from injury, such as poisoning or blood loss, and has been shown to treat many life threatening conditions (e.g., heart attacks, ARDS, or pancreatitis)
- DMSO has been shown to treat disorders of the urogenital tract and reproductive system, such as kidney stones, nephritis, enlarged prostates, prostatitis, cystitis, epididymitis, genital pain, urethral syndrome, tubal infertility, and endometrial inflammation or fibrosis
- DMSO has also been shown to repair damaged organs (e.g., liver cirrhosis, pulmonary fibrosis, smoke inhalation damage) and improve blood sugar control
Dimethyl sulfoxide (DMSO) is a remarkably safe1 naturally occurring compound that can treat a variety of challenging conditions. Since DMSO is incredibly effective for treating chronic pain, arthritis, and injuries like sprains or burns2 (discussed further here), it quickly spread across America as a miracle drug.
Thousands of studies were conducted to confirm its value, and before long, hundreds of thousands of people considered it to be the most important therapeutic ever discovered. Unfortunately, due to politics, the FDA turned against DMSO and refused to relent3 even once:
• DMSO was shown to effectively treat strokes, traumatic brain injuries, spinal cord injuries, and many circulatory disorders (discussed here).
• DMSO was shown to cure a variety of “incurable” autoimmune and connective tissue disorders (discussed here).
• DMSO was shown to treat a variety of challenging (and often incurable) eye, ear, sinus, and dental conditions such as tinnitus and blindness (discussed here).
Since publishing those articles, I’ve received over a thousand reports from people of the remarkable effects DMSO has had on them (which can be read here), that while unbelievable, are almost identical to what people across America reported before the FDA buried DMSO.
Reversing Organ Degeneration
The following process underlies many disease states:

In rapid cases, this is easy to recognize (as cells will rapidly die after a traumatic injury or having their blood supply cut off), whereas in slower cases (e.g., those arising from a chronic illness or toxicity), the issue often is that the cellular repair process becomes frozen and unable to bring the cells back to normal functioning.
Many regenerative medical therapies in turn, seek to “unfreeze” this cell danger response so that the normal function of the cells can be restored.
DMSO is uniquely suited to reversing this process as, especially when done early in the rapid cases following a severe injury (whereas the more gradual and chronic ones we often see frequently require systemic regenerative therapy). This is because:
1. DMSO protects the blood supply of the body,4 and disperses the microclotting, which often follows injury (e.g., burns) and leads to tissue death.5 Simultaneously, it also protects tissues from dying during periods of inadequate blood supply (ischemia) or being injured when that blood supply is rapidly restored (reperfused).
Numerous animal studies have demonstrated DMSO’s protective effect in organs that rapidly die once they lose their blood supply, such as the heart6,7,8,9,10,11,12 and brain13,14,15,16,17,18,19,20,21,22,23 (and even DMSO maintaining their function24,25,26 during periods of ischemia).
Likewise, DMSO has also been shown to prevent ischemia and reperfusion injuries to the liver27,28 kidney,29,30,31,32 lungs,33,34 ovaries35 and small intestine.36
2. DMSO protects organs from toxins that would otherwise be lethal to them or permanently damage them. This has been shown with the heart,37 kidneys,38,39,40 liver41,42,43,44 lungs,45 pancreas.46,47,48 Additionally, DMSO has also been repeatedly shown to mitigate radiation damage to tissues (e.g., in the kidneys).49
3. DMSO has been shown to protect the brain50,51 liver,52 and lungs53 from the tissue damage that develops after blunt trauma or surgical excisions.
Note: This was also repeatedly demonstrated in humans with severe blunt head trauma.54,55,56
4. DMSO dampens the destructive autoimmune process and swelling that often follows tissue trauma.57,58 In addition to protecting organs from injury, and reversing that degenerative process, DMSO has also been shown to help with a variety of challenging medical conditions.
Heart
The majority of the pertinent studies evaluating DMSO’s interactions with the heart (e.g., the previously mentioned ones) evaluated its ability to protect the heart from ischemic events like heart attacks and to improve the circulation within the body.59

Save This Article for Later – Get the PDF Now
Gastrointestinal Tract
Numerous randomized controlled trials conducted in Iraq found DMSO was highly beneficial for gastrointestinal diseases:
| One evaluated 136 patients with recurrent attacks of proctosigmoid ulcerative colitis that were not being prevented by their prophylactic medical regimen. For those receiving standard care, 51% recovered in two weeks compared to 84% of those also receiving DMSO. Over the next year, 25% of those continuing to receive standard care had a relapse rate, whereas only 5% of those receiving DMSO did.60 |
| One evaluated hospitalized patients with pelvic fractures or hypovolemic shock who were at risk for a stress induced gastric ulcer. Of the 58 controls, 22% developed an ulcer, whereas of the 57 receiving DMSO, only 4% did. Additionally, none of those receiving DMSO deteriorated or required emergency surgery, whereas 8 controls and 1 allopurinol recipient did (of whom 3 then died).61 |
| One evaluated 302 consecutive patients with previous symptomatic duodenal ulceration that was shown to have healed, and who were smokers and social drinkers, to receive four different treatments. Of the 220 available for evaluation, 65% who received a placebo had a recurrence of the ulcer, 30% of those who received cimetidine, and 13% of those who received oral DMSO.62
Note: Similar results have been obtained by American physicians in a smaller number of patients.63 |
| One evaluated 363 consecutive patients whose duodenal ulcers that did not heal despite 3 months of treatment with cimetidine (and who were cigarette smokers or social drinkers), were given either cimetidine twice a day alone or with DMSO or allopurinol. In 315 patients who were evaluable for analysis, at 8 weeks, 60% of those who had cimetidine recovered, whereas 100% of those who received DMSO recovered.
Additionally, the one year relapse rate was 29% for cimetidine alone and 7% in those who took DMSO.64 |
| One evaluated 238 patients with symptomatic acute duodenal ulceration who were smokers and social drinkers were randomized to receive for 8 weeks cimetidine or 8 weeks of a half dose of cimetidine plus oral DMSO (400mg two times a day) or allopurinol. After 8 weeks, 69 of the 87 (79%) who only received cimetidine recovered, whereas all of the 85 who received DMSO did.
Additionally, 67% of those who received cimetidine over the next year relapsed, compared to 6% of those who took DMSO.65 |
| One evaluated 101 patients presenting with hematemesis (coughing up blood) due to erosive gastritis (a fairly dangerous condition). It gave them either saline or oral allopurinol and DMSO orally every 6 hours for 5 days.
Of the 50 controls and 48 who were treated (along with 2 who left because they could not tolerate the treatment), 29% of the controls and 8% of who were treated had further episodes of hematemesis (with three of the controls requiring subsequent surgery — one of whom died). Of those who remained stable, a subsequent endoscopy showed evidence of hemorrhagic inflammation in 44% of controls and 9% of those who were treated.66 Finally, DMSO also has been shown to help with irritable bowel syndrome, acute or chronic gastritis, peptic ulcers, enterocolitis, and mucomembranous colitis.67 |
Liver
In addition to DMSO protecting the liver from injury, DMSO can sometimes heal the liver. For example, 12 patients who had terminal liver cirrhosis who agreed to stop drinking all alcohol for the duration of the program were put on daily DMSO program.
Of the 8 who chose to continue the program for 6 months, all had improved health, significantly reduced vomiting, and improved liver function tests, and rather than all being dead within one year as expected, they were in better condition than they had been at the start of the study.68
Gallbladder
- A rat study created obstructive jaundice by ligating (cutting off) the common bile ducts and found that laboratory values showed DMSO mitigated the expected pathologic effects.69
- A Japanese study found that injecting 90% DMSO mixed with 5% hexametaphosphate into the biliary tract effectively dissolved gallstones within the liver and was safe for the patients.70
Lungs
Additional data supports the protective role of DMSO for the lungs:
•After sheep experienced a lung injury from inhaling smoke, nebulized DMSO (with heparin) was found to reduce the damage to their lungs significantly.71
Note: Some unresolved questions exist regarding the safety of long term DMSO nebulization.72
•DMSO was found to prevent oxygen deprivation and inability to exchange gasses through the lungs which results from an Ehrlichia ruminantium infection (which is typically fatal).
DMSO has also been shown to treat acute respiratory distress syndrome (ARDS), a challenging condition that frequently results in being placed on a ventilator (e.g., this happened throughout COVID-19).
In a hamster study and a mouse study, where a toxin was used to induce ARDS, DMSO significantly reduced the resulting lung damage and fluid leakage (which effectively drowns ARDS patients).73,74 A third mouse study found DMSO prevented all of them from dying (whereas 58% of controls died).75
In the one human study where IV DMSO was used for ARDS (given intravenously at concentrations under 10%) it was found to produce a dramatic improvement in all three patients who received it (e.g., one patient’s lungs were completely normal after a week) and prior to receiving DMSO all three were near death.76

Note: In the one case when DMSO was nebulized, the improvement occurred in 1 hour.
Finally, DMSO can help chronic lung conditions.
• One study found DMSO reduces chronic pulmonary fibrosis, and this beneficial effect was increased when it was mixed with zinc.77
• For older patients with chronic respiratory insufficiency (leading to chronically low blood oxygen levels, elevated carbon dioxide levels and an abnormal acid base balance, especially during exercises) due to issues in the lungs or bronchi, DMSO was found to bring about a recovery without the need for hospitalization in 35/43 (81%).78
• Human studies also have shown DMSO can treat asthma.79
Pancreas and Diabetes
Diabetics have reported that DMSO reduces (but does not eliminate) their need for insulin and that DMSO is particularly helpful for the condition since it can also alleviate the pain from diabetic peripheral neuropathy.80 Studies in this area include:
• Alloxan is toxic to the insulin producing cells of the pancreas and can be used to induce diabetes. A 1977 study found that DMSO prevented alloxan from causing diabetes.81
• DMSO has been shown to prevent the immune system from attacking transplanted insulin secreting cells (suggesting DMSO has significant potential for Type 1 diabetes).82
• GLP-1 is a key hormone the body uses to regulate satiety and blood sugar (and which diabetes drugs like Ozempic mimic). One study found that 0.5% to 2.5% DMSO increased GLP-1’s production of insulin by 2 to 2.5 times. This suggests DMSO could help treat diabetes or allow GLP-1 users to use a lower dose of the medication.83
• Exposing insulin secreting cells to DMSO was found to enhance glucose-induced and tolbutamide-stimulated insulin secretion without significant effects on basal secretion or potassium responsiveness.84
DMSO (along with ultraviolet blood irradiation) has also been shown to help pancreatitis, a challenging and dangerous condition85 (as there are no conventional treatments besides supportive care for most types of pancreatitis). For example, three rat and mice studies found DMSO significantly improved experimentally induced pancreatitis.86,87,88
Additionally, a randomized double-blind trial took 78 patients with chronic recurring pancreatitis (and no other confounding gastrointestinal disorders) who presented within 2 hours with signs of pancreatitis but did not have signs of generalized peritonitis. Of them, 26 received 10% DMSO rectally, and at least 57% were free of pain after 12 hours (compared to 17% of controls), and all were free of pain after 24 hours (whereas 48% of controls were still in pain).
As a result, all DMSO subjects were discharged within 3 days, whereas only 22% of controls were discharged after 5 days of hospitalization.89
Kidneys
In most circumstances, DMSO has been shown to be safe for the kidneys, to function as a potent diuretic, and to increase the kidney flow rate.90 In addition to protecting the kidneys from ischemia and toxins like mercury, many studies have also shown DMSO protects the kidneys from amyloidosis.91
Many kidney autoimmune diseases result from immune deposits in the kidneys (one of which is Heymann nephritis, an experimentally induced form of nephritis92 where antibodies that target the kidneys are injected causing immune deposits on the glomerular walls). In three rat studies of Heymann nephritis, DMSO was found to protect the kidneys and their function.93,94,95
Similarly, a study of 56 DMSO treated rats (and 48 controls) with lupus nephritis found that those who received DMSO had nearly normal kidneys, whereas the controls had significant damage to their kidneys.96 DMSO, likely due to its effects on zeta potential,97 has also shown promise for kidney stones:
• A study fed rats a diet designed to create kidney stones, and found that after two months, 40 of the 45 water-drinking rats had developed stones in the kidney, bladder or ureter, while only 11 of the 46 DMSO group did.98
• A study of 6 patients with kidney stones (5 of which were confirmed by ultrasound) found IV DMSO99 resolved the condition in 2 to 3 treatments (although one patient had a complete resolution after a single infusion).100
Note: We have had a great deal of success treating kidney stones by improving the physiologic zeta potential.
Genitourinary Disorders
DMSO is extremely helpful for inflammation of the bladder, particularly “interstitial cystitis” (also known as painful bladder syndrome), a challenging condition which results in very frequent, painful (and often bloody) urination. DMSO, however can also help many other parts of the urinary tract. For example one study found:101

Likewise, a study of inflammatory conditions of the urinary tract, in addition to showing significant benefit for interstitial cystitis, also found:102
• Of the 12 patients with radiation cystitis (e.g., from prostate cancer therapy) 50% had a good response to it.
• Of the 35 patients with chronic prostatitis, 75% benefited significantly, with 12 having an “excellent” response, 14 a “good” response, and in 90% of cases, inflammation of the prostatic urethra improved.
• Another study gave 4 men with chronic excessive (and untreatable) urination due to bladder or prostate issues DMSO, 3 of whom had an excellent response.103
• A Polish study found urethral syndrome (chronic irritation of the urethra without signs of an infection) responds to DMSO being put into the urethral tract.104
Note: Many other remarkable reports exist of DMSO’s value for prostatitis (e.g., one DMSO doctor recently shared that it treated 40 out of 40 cases of bacterial prostatitis).105
Additionally, while no formal studies have been conducted on prostate enlargement many anecdotal reports (including from readers of the Forgotten Side of Medicine) have found DMSO is remarkably beneficial for this condition.106
Reproductive Disorders
• A 1975 Chilean study at a Navy hospital took 69 women who were infertile due to an obstruction in their fallopian tubes and injected a DMSO mixture into their fallopian tubes six separate times (and then repeated the series if the tubes had not opened). Out of 47 patients, 27 (57.4%) subsequently became pregnant, including one who got pregnant twice (without any further assistance).
Of the 27 pregnancies, 12 resulted in successful deliveries, 7 had a normal pregnancy at the time of publication, 4 patients chose to have abortions, and 3 had spontaneous abortions, and 1 had an abnormal pregnancy requiring a surgical intervention, and 0 had ectopic pregnancies (one of the risks of surgically opening the fallopian tubes).
Additionally, out of the 426 DMSO hydrotubations which were performed, only 7 (1.5%) had side effects all of which were minor.107
Note: 25% to 35%108 of infertility is due to tubal obstructions (typically from inflammation there). The current surgical approach for opening a tubal obstruction and restoring fertility (which bears some risks) has a 10% to 30%109,110 success rate.
• One study administered 10% to 30% DMSO into the uteruses of horses that could not get pregnant. It found no harm occurred to the lining of the uterus and that 18 out of 27 had significant improvement to the lining of their uterus (compared to 2 out of 18 who received a saline placebo), such as a reduction of chronic inflammatory cell infiltrates and reduction of periglandular fibrosis.
Additionally, there were signs their fertility improved, but the trial’s design made it impossible to be sure this improvement occurred.111
A New Therapeutic Principle
When DMSO was discovered, Stanley Jacob quickly realized that it represented a new therapeutic principle since it made so many things which had previously seemed impossible in medicine suddenly possible — and even more remarkably, 60 years later, many of the things DMSO can address the medical system still struggles to deal with.
For example, in the same way DMSO could significantly improve surgical outcomes,112 the data here makes good case that DMSO should be a mainstay therapy whenever someone is at risk of organ failure from being poisoned (e.g., due to a drug overdose). Likewise, the data here shows how numerous immensely challenging diseases that require a hospital or intensive care admission could be dramatically improved with DMSO.
However, while the FDA’s war against DMSO was immensely unfortunate, I am extremely hopeful the unprecedented political climate we are now entering we will at last make it possible to reform a medical system that has always put profits before people.
Much of that is thanks to the incredible work many of you have done throughout the pandemic to bring awareness to the crimes of the medical industrial complex and I am profoundly grateful to each of you for helping to make it happen and giving me the voice to as well.
Author’s note: This is an abridged version of a longer article that goes into greater detail on the data discussed here, how DMSO is used for each of the conditions mentioned (along with other approaches we’ve seen help them), and provides guidance for personal DMSO use (e.g., dosing, therapeutic precautions and where to obtain it). That article and its additional references can be read here.
A Note from Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician from the Midwest and a longtime reader of Mercola.com. I appreciate AMD’s exceptional insight on a wide range of topics and am grateful to share it. I also respect AMD’s desire to remain anonymous since AMD is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
Staghorn Kidney Stones — What They Are and How to Avoid Them
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/01/06/staghorn-kidney-stones.aspx
Analysis by Dr. Joseph Mercola January 06, 2025

STORY AT-A-GLANCE
- Staghorn kidney stones are large, branched structures primarily composed of struvite. They account for about 10% to 15% of kidney stone cases in developing countries
- Risk factors for staghorn stones include chronic UTIs, anatomical abnormalities, long-term catheter use, neurogenic bladder conditions and metabolic disorders that affect your urinary composition
- Unlike smaller kidney stones, staghorn stones initially do not show symptoms, but later cause abdominal pain, blood in urine and fever, leading to sepsis and kidney failure if untreated
- Treatment for staghorn stones typically requires surgical intervention like percutaneous nephrolithotomy; extracorporeal shockwave lithotripsy is a less invasive option
- Strategies to prevent recurring UTIs and lower your risk of staghorn stones are included below
Kidney stones are solid mineral and salt deposits that form in the kidneys, causing intense pain and discomfort. Each year, over half a million people visit emergency rooms due to kidney stone issues. According to the National Kidney Foundation,1 1 in 10 people will develop a kidney stone at some point in their lives.
There are four primary types of kidney stones — calcium oxalate, uric acid, struvite and cysteine. Among these, the struvite stones have the most distinctive appearance, as they form into large, branched structures known as “staghorn calculi,” which fill the kidney’s inner spaces.2
Because of their size and position, staghorn stones are particularly dangerous and challenging to treat. Recognizing their symptoms, understanding the risk factors and familiarizing yourself with effective management strategies for this condition are essential for timely detection and treatment.
What Are Staghorn Kidney Stones?
Staghorn stones, named for their distinctive “antler-like” shape, are primarily composed of struvite (magnesium ammonium phosphate) and typically form due to chronic urinary tract infections (UTIs), especially from bacteria that produce the enzyme urease, such as Proteus mirabilis. This enzyme breaks down urea, which increases the concentration of ammonia in the urine, raising its pH and creating an alkaline environment conducive to stone formation.3
Staghorn stones account for about 10% to 15% of kidney stones in developing countries, while the rate is lower in developed nations due to early detection and preventive measures.4 The symptoms of staghorn stones differ from other types of kidney stones because of their size and complicated structure.
While smaller stones cause intense, sharp pain when they get stuck in your urinary tract, staghorn stones typically do not produce obvious symptoms at first. Over time, however, they lead to pain on the sides of your abdomen, between your ribs and hip, as well as blood and pus in your urine, exhaustion and fever. In more serious cases, they increase the risk of sepsis, a life-threatening response to infection.5,6
The anatomy of staghorn stones complicates treatment. They branch out into the renal pelvis, a funnel-shaped area of the kidney that channels urine into the ureters, which then carry it to the bladder for storage. If the renal pelvis or ureters are blocked, kidney swelling will occur. These stones may also block the calyces, where urine collection starts. Swelling of these areas, called caliectasis, leads to kidney failure if untreated, so prompt diagnosis and treatment is important.7,8
Are You at Risk of Developing Staghorn Kidney Stones?
Certain risk factors increase your likelihood of developing staghorn kidney stones, with chronic UTIs being the most significant. Individuals with a history of frequent UTIs or kidney infections need to be vigilant about developing this condition. Women, in particular, face a higher risk due to anatomical susceptibility to UTIs.9
In addition to that, several anatomical and medical conditions significantly increase your risk, such as having an atypical urinary tract anatomy. Any blockages in your urinary tract create areas where minerals accumulate and crystallize, leading to stone development.
Long-term catheter use presents another significant risk factor, as catheters introduce bacteria and create conditions favorable for stone formation. Similarly, if you’ve undergone a urinary diversion procedure in the past, your altered urinary anatomy promotes stone development.10
Moreover, having a neurogenic bladder, a condition where nerve damage affects bladder function, creates a perfect environment for staghorn stones because of incomplete bladder emptying and frequent infections. Additionally, if you’ve had untreated kidney stones in the past, they serve as starting points for larger staghorn calculi to develop.11
Metabolic disorders play a role in stone formation as well. Obesity increases your risk through various mechanisms, including altered kidney function and increased crystal formation in urine.12 Diabetic patients face elevated risks due to changes in urine composition and pH levels. High blood sugar also impairs your immune response, allowing bacterial infections to thrive.13
The combination of these metabolic conditions with poor dietary habits or dehydration makes stone formation even more likely. Diagnosis of staghorn stones involves urinalysis and imaging to assess both stone presence and infection. A urinalysis checks for bacteria and elevated pH levels, which are strong indicators of infection-related stones. Imaging through X-rays, ultrasounds or CT scans reveals the stone’s shape, size and location within the kidney.

Save This Article for Later – Get the PDF Now
How Are Staghorn Kidney Stones Treated?
While small kidney stones typically pass on their own without medical intervention, larger ones like staghorn stones often require more intensive treatment. Because of their complex, branching structure, staghorn stones typically don’t resolve with medical therapy alone.
Medical treatments are often used as supportive measures to reduce infection risk and manage symptoms rather than to remove the stones entirely. Complete surgical removal is often recommended to address staghorn stones, with surgical techniques like percutaneous nephrolithotomy (PCNL) being the most common.14
This minimally invasive procedure involves making a small incision on your back, wherein instruments will be inserted directly into the kidney to break up and remove the stones. PCNL has largely replaced traditional open surgeries for staghorn stores, like anatrophic nephrolithotomy or pyelolithotomy, which carry significant risks and do not always achieve complete stone removal.15
For patients seeking less invasive options, extracorporeal shockwave lithotripsy (ESWL) is another option, especially for smaller fragments or remaining stone pieces after PCNL. In ESWL, sound waves are directed at the stones to break them into smaller fragments, allowing them to pass naturally through the urine over days or weeks.16
Address Recurring UTIs to Reduce Your Risk of Staghorn Kidney Stones
Since recurring UTIs are the primary risk factor for staghorn kidney stones, taking proactive steps to maintain a healthy urinary tract is important. Here are practical strategies to reduce your risk of UTIs:
| Stay hydrated — Drink plenty of pure, filtered water daily to dilute your urine and flush out bacteria. |
| Don’t delay urination — Empty your bladder as soon as you feel the need; holding it in promotes bacterial growth. |
| Practice good hygiene — Always wipe from front to back to keep bacteria from entering your urethra. |
| Opt for showers over baths — Avoid prolonged exposure to water in hot tubs or jacuzzis, which encourage bacterial infections. |
| Practice pre- and post-sexual hygiene — Cleanse your genital area before and after sexual activity. |
| Avoid irritants — Skip feminine hygiene sprays or other products that will irritate your urethra. |
| Consider using a bidet — This provides gentle, thorough cleansing, reducing irritation and bacteria transfer compared to wiping with tissue. |
| Eat fermented foods — Incorporate kefir, sauerkraut and other fermented foods into your diet to support a healthy microbiome. |
Cranberries are also a powerful natural ally against UTIs. They contain proanthocyanidins, which inhibit E. coli — a common UTI-causing bacteria — from adhering to the bladder walls. A comprehensive review in the Cochrane Database of Systematic Reviews17 found that cranberry products reduced the risk of symptomatic, culture-verified UTIs in women with recurrent infections and in children and individuals prone to UTIs after medical interventions.
The source of your meat matters too, as contaminated meat harbor UTI-causing bacteria. Conventionally raised chicken is particularly problematic, not just for its bacterial load but also for its high linoleic acid (LA) content, which is harmful to overall health. If you choose to eat chicken, opt for organic, pasture-raised options. Ideally, source your meat from local farms that use regenerative farming methods to reduce contamination and protect your health.
Methylene Blue Helps Against UTIs, Too
For treating UTIs, consider using methylene blue, a potent compound with a long history of medicinal use. Discovered in 1876, it was originally used as a textile dye but is now recognized for its remarkable antimicrobial properties. Unlike antibiotics, methylene blue is excreted directly into the bladder, where it becomes highly concentrated, effectively killing pathogens there without disrupting the gut microbiome.
In addition to fighting UTIs, methylene blue offers cognitive benefits, such as improving brain health and reducing dementia risk, making it especially valuable for older adults prone to UTIs. It serves as a unique, targeted treatment with minimal side effects compared to traditional antibiotics. Learn how to use it as a part of your treatment protocol in “Benefits and Side Effects of Methylene Blue — A Comprehensive Guide.”
Can You Eat Oxalate-Containing Food if You Have Staghorn Stones?
Staghorn stones are primarily composed of struvite, but they sometimes include calcium oxalate or calcium phosphate. While these are usually secondary components, limiting high-oxalate foods is a smart precaution if you’re dealing with any type of kidney stone. In fact, I believe managing oxalate intake benefits everyone — not just those with kidney stones, metabolic challenges or mineral imbalances.
Oxalates are natural compounds found in many plant foods, including beans, grains, seeds, nuts, fruits, berries and herbs. When consumed in excess, oxalates interfere with various body functions and lead to joint pain, digestive issues, skin irritation and reduced cellular energy production.
Gut health and kidney stone risk are closely linked, and since oxalates are gut-irritating antinutrients, reducing them in your diet supports healing. Start by identifying and cutting out high-oxalate foods until your gut health improves. Common high-oxalate foods to watch for include:
- Spinach — Contains up to 600 to 800 milligrams (mg) of oxalates per 100 grams. In addition to spinach, other leafy greens considered “superfoods,” like Swiss chard and beet greens, are also high in oxalates, so you’ll want to avoid them, especially if you’re prone to kidney stones or sensitive to oxalates.
- Almonds — Contains around 122 mg of oxalates per 100 grams. However, all nuts in general are particularly problematic, since they contain LA. Even macadamia nuts add to your toxic load, as they contain oleic acid, which could just be as bad as LA.
- Peanut butter — Contains around 140 mg of oxalates per 100 grams.
- Sweet potatoes — Approximately 30 mg of oxalates per 100 grams. Although this is considered high compared to other vegetables, it’s actually much lower than spinach or nuts.
- Figs — They have approximately 40 mg of oxalates per 100 grams.
I recommend watching my interview with Sally Norton, an esteemed authority on oxalates, to learn more about oxalates and how to reduce their harmful effects to your health.
Additional Strategies to Minimize Oxalate-Related Risks
Since excess oxalates sometimes contribute to the development of staghorn stones,18 I recommend implementing strategies to reduce and eliminate them from your body. In addition to avoiding high-oxalate foods listed above, consider the following key recommendations:
| Increase your calcium intake — Eating calcium-rich foods or taking calcium supplements helps bind oxalates in the gut, preventing their absorption and promoting excretion through your stool. Good sources of calcium include dairy products and low-oxalate leafy greens like kale. |
| Stay hydrated — Drink plenty of water throughout the day to flush oxalates from your system and lower the risk of kidney stone formation. |
| Optimize your gut health — A balanced gut microbiome aids in breaking down oxalates. Add probiotic-rich foods like yogurt, kefir and fermented vegetables to your diet to encourage the growth of beneficial bacteria such as Oxalobacter formigenes, which naturally degrade oxalates. |
| Incorporate citrate into your diet — Found in lemons, limes and oranges, citrate binds with calcium and oxalates, reducing the likelihood of stone formation. However, be careful not to take excessive ascorbic acid (vitamin C), as high doses convert into oxalates. |
| Cook high-oxalate foods well — If you do choose to eat high-oxalate foods, boiling them will significantly lower their oxalate content as the compounds leach into the cooking water, which is then discarded. |
| Use topical calcium for oxalate-related skin irritations — If oxalates are causing you skin irritation, applying topical calcium will neutralize them and provide relief directly at the site. |
- 1 National Kidney Foundation, Kidney Stones
- 2, 3, 6, 8, 10, 11 Cleveland Clinic, Staghorn Calculus
- 4, 7, 9 Int Braz J Urol. 2020 Sep 2;46(6):927–933
- 5, 12 American Urological Association, Kidney Stones
- 13 International Journal of Medical Science and Clinical Research Studies. July 2023; Volume 03 (Issue 7)
- 14, 15, 16 Medscape, Struvite and Staghorn Calculi Treatment and Management
- 17 Cochrane Library, April 17, 2023
- 18 Medscape, Struvite and Staghorn Calculi
All About Phytic Acid and Phytates – Good and Bad
Reproduced from original article:
https://www.precisionnutrition.com/all-about-phytates-phytic-acid
By Ryan Andrews, MS, MA, RD, RYT, CSCS
Phytic acid – the storage form of phosphorus – is one of those pesky “anti-nutrients” the Paleo community keeps telling you to avoid.
It’s often considered an anti-nutrient because it binds minerals in the digestive tract, making them less available to our bodies.
Yet these same anti-nutrient properties can also help in the prevention of chronic disease.
What is phytic acid?
Seeds — such as nuts, edible seeds, beans/legumes, and grains — store phosphorus as phytic acid. When phytic acid is bound to a mineral in the seed, it’s known as phytate.
The tables below compare various seed types according to their phytic acid/phytate content.
Whole grains
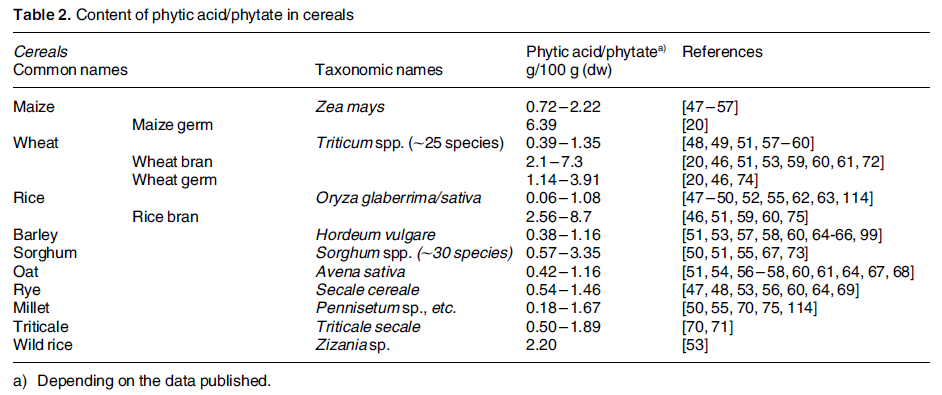
Legumes
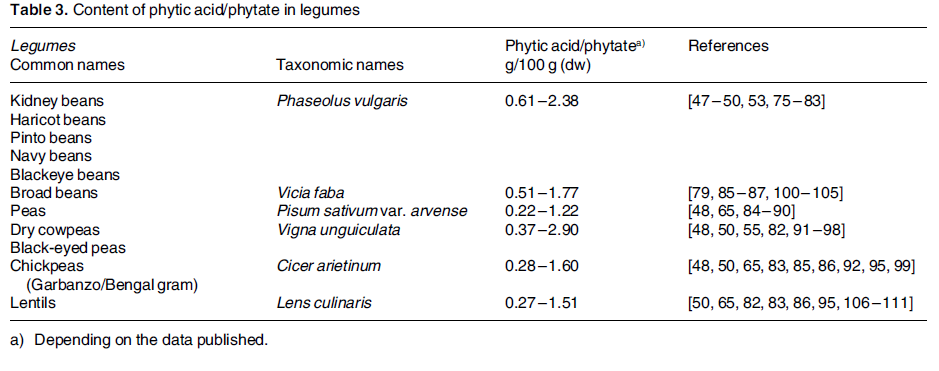
Nuts
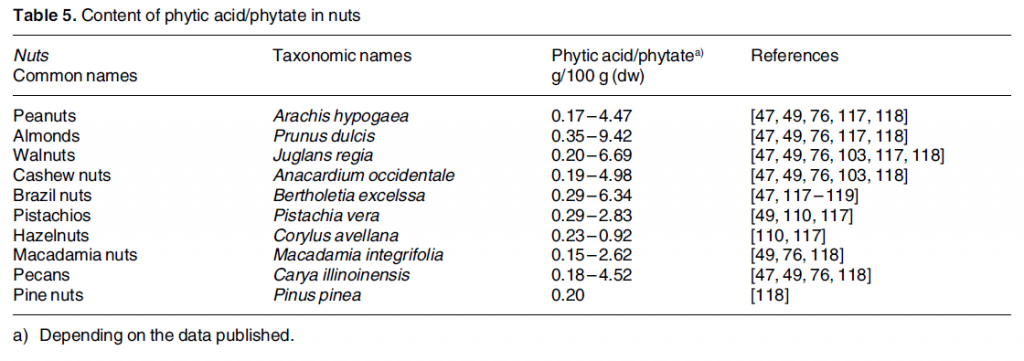
Oil seeds
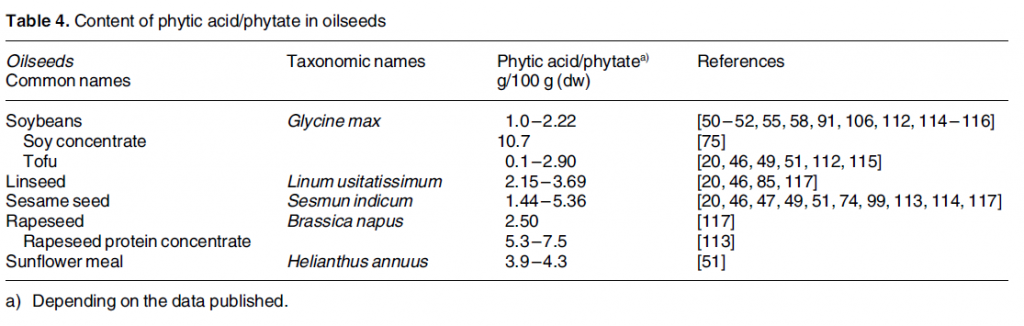
As you can see, phytic acid content varies greatly among plants. This is due to the type of seed, environmental condition, climate, soil quality, how phytate is measured in the lab, and so forth.
Roots, tubers, and other vegetables may also contain phytic acid, but usually in lower amounts.
The most concentrated sources tend to be whole grains and beans. Phytic acid is isolated in the aleurone layer in most grains, making it more concentrated in the bran. In legumes, it’s found in the cotyledon layer (where the protein is).
Phytate = phytic acid bound to a mineral
Phytates perform an essential role in plants, as they are an energy source for the sprouting seed. When a seed sprouts, phytase enzymes break down the stored phytates.
When we eat the plant, phytates are hydrolyzed during digestion to myo-inositol-1,2,3,4,5,6-hexkisphosphate (IP6) and lower inositol polyphosphates including IP1 through IP5 (these are phytate degradation products).
Who’s eating phytic acid?
Everyone who eats plants consumes some phytic acid. It’s all a question of degree.
As you can imagine, intake tends to be much higher among those who follow non-Westernized diets. In developing countries, plants are staple foods, which means people eat more of them, and therefore get more phytic acid.
In developed countries, plant-based or vegetarian eaters tend to consume more phytic acid than omnivores. Further, males usually consume more phytic acid than females, simply because they eat more food.
Phytate digestion
Most phytate (37-66%) is degraded in the stomach and small intestines.
Ordinarily, our bodies regulate phytate levels pretty well, adjusting uptake in the gut and excretion until body levels come into balance.
Vitamin D status in the body seems to influence how much phytate is actually retained. The more vitamin D, the more phytate retained; the less vitamin D, the less phytate retained.
Potential problems with phytic acid
Phytic acid can bind minerals in the gut before they are absorbed and influence digestive enzymes. Phytates also reduce the digestibility of starches, proteins, and fats.
Here’s an example.
Vegan eaters often consume more iron than omnivores. Yet, they also consume more anti-nutrients, including phytates, and these reduce the amount of iron available to their bodies. Consuming 5-10 mg of phytic acid can reduce iron absorption by 50%.
This is why vegetarian eaters should eat more iron than omnivores (33 mg for veg eaters vs. 18 mg for omnivores).
Daily iron loss for men & women
- Adult men lose ~1 mg of iron per day
- Adult menstruating women lose ~1.4 mg/day
- Postmenopausal women lose ~0.8 mg/day
- Lactating women lose ~1.1 mg/day
While in the intestines, phytic acid can bind the minerals iron, zinc, and manganese. Once bound, they are then excreted in waste.
This can be a good or bad thing, depending on the condition. It’s a bad thing if you’re having trouble building up iron stores in the body and have developed iron-deficiency anemia.
When is it a good thing? Keep reading – you’ll find potential benefits of phytic acid below.
Potential benefits of phytic acid
Despite its potential drawbacks, phytic acid is similar in some ways to a vitamin, and metabolites of phytic acid may have secondary messenger roles in cells.
Some experts even suggest that it’s the phytic acid in whole grains and beans that lends them their apparent protective properties against cardiovascular disease, cancer, and diabetes.
(Remember, the grains with little to no phytic acid are the refined ones.)
The supplement industry has caught on to this. Have you even seen a bottle of inositol hexaphosphate, or IP6? That’s simply a supplemental source of phytic acid.
When phytic acid binds minerals in the gut, it prevents the formation of free radicals, thus making it an antioxidant. Not only that, but it seems to bind heavy metals (e.g., cadmium, lead) helping to prevent their accumulation in the body
Phytic acid’s preventative properties
Cancer
Foods higher in phytic acid seem to enhance the activity of natural killer cells and inhibit tumor growth.
Those who consume more phytic acid are less likely to succumb to breast and prostate cancer. Exposing the colon to less iron seems to decrease the risk of colon cancer. And phytic acid might reduce the side effects of chemotherapy.
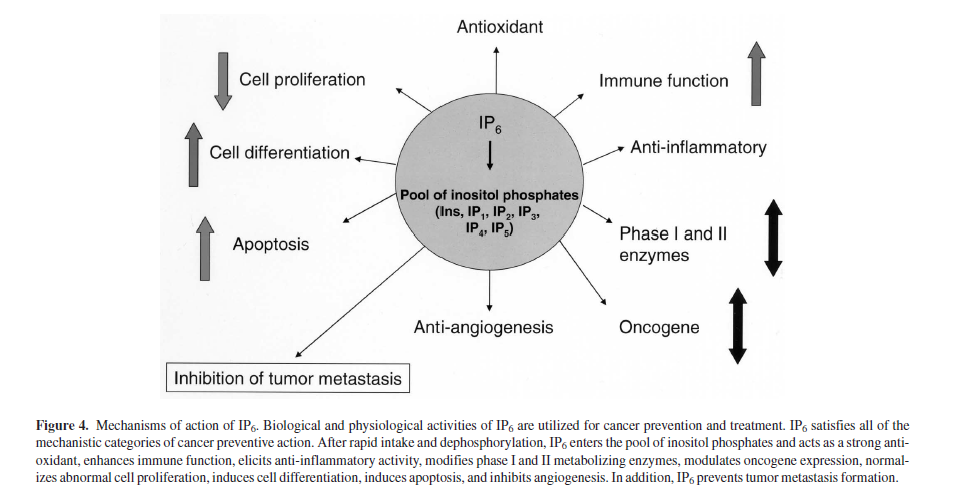
Cardiovascular disease
Phytic acid helps prevent hardening of the arteries and platelet formation.
Kidney stones
With some phytate being excreted in the urine, this may improve kidney health and prevent stones.
Insulin resistance
Phytic acid plays a role in pancreatic function and insulin secretion. And it may reduce the glycemic response from meals, meaning you feel full for longer.
Hemochromatosis
Hemochromatosis, or iron overload, is a common genetic disorder that phytic acid’s iron-binding properties can protect against or reduce.
In the balance
Is phytic acid worth worrying about? Maybe not, for most of us.
One study showed that subjects consuming a Mediterranean-style diet that included 1000-2000 mg of phytic acid per day did not suffer from reduced mineral bioavailability.
At the same time, certain people might have to be more wary.
In particular, iron intake and absorption can be critical for infants nearing six months of age. So when plants are added to infants’ diets, it may be important to adopt strategies to reduce phytic acid and enhance iron absorption.
Overcoming phytic acid as an antinutrient
Luckily, it’s possible to overcome the anti-nutrient effects of phytic acid in our foods while still getting the benefits of a plant-rich diet. Here are a few strategies that my be more or less helpful depending on the specific situation:
Heat
Heating foods can destroy small amounts of phytic acid. (Note: heat can also destroy phytase and vitamin C.)
Processing
Milling grains and removing the bran decreases phytic acid. Unfortunately, milling also tends to remove many of the minerals! Removing the bran and then enriching a food with minerals might allow for enhanced nutrient absorption in the body.
Soaking
Soaking beans and grains can reduce phytic acid (and other antinutrients).
Fermenting
Fermentation and bread leavening (using yeast) can help to break down phytic acid due to the activation of native phytase enzymes, reducing the number of phosphate groups.
This is big stuff since myo-inositol phosphates with fewer than five phosphate groups don’t inhibit zinc absorption (IP1 to IP4). And those with fewer than three phosphate groups don’t inhibit iron absorption (IP3 to IP2).
Also, some of the acids produced during fermentation might actually boost absorption of certain minerals.
Sprouting
Sprouting and malting enhances native phytase activity in plants and thus decreases phytic acid.
Vitamin C
Vitamin C appears strong enough to overcome phytic acid. In one study, adding 50 mg of vitamin C counteracted the phytic acid load of a meal. In another study, 80 mg of ascorbic acid (vitamin C) counteracted 25 mg of phytic acid.
Protein powders
During processing of plant-based protein powders, it’s possible to de-phytinize (via addition of microbial phytase). Also, protein isolates and concentrates can be treated with dialysis or ultrafiltration to remove phytic acid.
Seed breeding
Scientists are working on seed breeds containing less phytic acid. There are modern seed hybrids of grain and legume plants that contain less phytic acid.
Animal protein
Animal protein may enhance absorption of zinc, iron, and copper. Adding small amounts of animal protein might increase the absorption of these minerals in the body. (Well, except for dairy/casein, as it also seems to hinder iron and zinc absorption.)
Gut health
A low pH in the gut enhances iron absorption. Balancing the level of beneficial bacteria in the GI tract might help with this. See All About Probiotics.

Bonus: Can other animals digest phytic acid?
Ruminant animals (e.g., cattle, sheep, goats, buffalo) possess phytase producing flora for digesting phytic acid.
Non-ruminant animals (e.g., pigs, chickens, dogs, cats) don’t have phytase producing flora, so phytic acid passes through them undigested and makes its way into the soil.
Feeding livestock too much grain can inhibit mineral absorption and increase phosphorus excretion, leading to pollution. Ever heard of the Dead Zone in the Gulf of Mexico?
Summary and recommendations
In healthy people eating balanced diets, phytic acid’s effects on iron, zinc, and manganese status is minimal and it doesn’t seem to cause nutrient deficiencies.
To argue that some plant foods are “unhealthy” because of their phytic acid content seems mistaken, especially when phytic acid’s potential negative effects on mineral assimilation may be offset by its health benefits.
So we should aim to reduce phytic acid rather than eliminate it.
To reduce the anti-nutrient effects of phytic acid in foods, try the following:
- Soak, sprout, ferment, and cook plant foods.
- Consume vitamin C-rich foods with meals that contain phytic acid. Dense source of vitamin C include guava, bell pepper, kiwi, oranges, grapefruit, strawberries, Brussels sprouts, cantaloupe, papaya, broccoli, sweet potato, pineapple, cauliflower, kale, lemon juice, and parsley.
- Use vinegar in salad dressings and cooking to enhance mineral absorption and offset phytic acid.
- Supplement with phytase enzymes if necessary.
- Eat mineral fortified foods if necessary
- Supplement minerals if there is still a shortfall in your diet.
- If you’re eating a plant-based diet and have confirmed nutrient deficiencies, and you’ve tried all the above strategies with no success, adding small amounts of animal foods on occasion might boost stores of necessary minerals in your body.

High Animal Protein Diet Raises Risk of Negative Calcium Balance
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/06/29/risks-of-high-animal-protein-diet.aspx
Analysis by Dr. Joseph Mercola June 29, 2024
STORY AT-A-GLANCE
- A diet high in animal protein may increase your risk of negative calcium balance, putting your health at risk
- Negative calcium balance occurs when your body loses more calcium than it absorbs, which can lead to kidney damage, insulin resistance, bone breakdown and other problems
- Animal protein, particularly, meat, eggs and cheese, leads to the formation of large amounts of acid in your body
- If your body can’t combat acid accumulation, metabolic acidosis can occur; even low-grade metabolic acidosis can lead to Type 2 diabetes, high blood pressure, fibromyalgia, gout and other chronic conditions
- While I don’t recommend vegan or vegetarian diets, including more fruits and vegetables, which are alkaline, as well as bicarbonate mineral waters, can help counteract acid load
In the video above, James DiNicolantonio, Pharm.D., who is also the coauthor of my book, “Superfuel: Ketogenic Keys to Unlock the Secrets of Good Fats, Bad Fats, and Great Health,” explains why a diet high in animal protein may increase your risk of negative calcium balance, putting your health at risk.1
Negative calcium balance occurs when your body loses more calcium than it absorbs. Almost all calcium — 99% — is found in your teeth and bones, so your body compensates for a lack of calcium by leaching it from your bones.
This process helps maintain necessary calcium levels in your blood, which is crucial for vital functions such as muscle contraction, blood clotting and nerve transmission, but can lead to weakened bones and an increased risk of conditions like osteoporosis.
“Animal foods, like meat, fish, eggs and dairy are the most nutrient-dense foods you can eat. However, there’s one downside to an animal-based diet, and that’s the high acid load,” DiNicolantonio says. The solution, according to DiNicolantonio, is to balance the acid from animal foods with base.
Carnivore Diet Linked to Negative Calcium Balance Since 1930
DiNicolantonio cites a study published in 1930,2 which details Arctic explorer Vilhjalmur Stefansson’s journey of eating only meat for a year.3 Over 12 periods of recorded data, “calcium balance was negative every single time,” DiNicolantonio says. “All this proves is that since 1930 we have known that consuming an all-meat diet — a carnivore diet — leads to negative calcium balance.”4
Another example included 10 healthy participants who consumed a strict low-carb diet for two weeks, then another carb-restricted diet for four weeks that was high in animal protein.
This led to a decrease in calcium balance, with the researchers concluding, “Consumption of an LCHP [low-carbohydrate high-protein] diet for 6 weeks delivers a marked acid load to the kidney, increases the risk for stone formation, decreases estimated calcium balance, and may increase the risk for bone loss.”5
The participants were still in positive calcium balance in this case, however, which DiNicolantonio says is only because they were consuming more than 800 milligrams (mg) of calcium a day:6
“You may not go in negative calcium balance if you’re consuming over 800 milligrams of calcium and you’re consuming a multivitamin, which likely contains vitamin D, which increases the absorption of calcium, you may not go in negative balance. But it still increased the propensity by significantly increasing the urinary calcium level by about 100 milligram a day.
… so if you’re on a carnivore diet you likely want to consume somewhere around 16 ounces of milk or three slices of cheddar cheese or a mixture of the two to give you about 600 milligrams of calcium because then you’ll get about another 81 milligrams of calcium from consuming 1.5 pounds of meat — which is what most people do consume on an animal-based or carnivore diet — around 1.5 pounds, maybe 2 pounds, of meat per day.”
Other research, published in Calcified Tissue International, found that when acid levels were higher, due to increased dietary protein intake, people had more acid in their bodies and lost more calcium in their urine.7 Meanwhile, research shows high-protein diets can cause increased calcium loss in urine, or calciuria.
In a study of 39 premenopausal women who lowered their protein intake to U.S. recommended dietary allowance levels, acid excretion, calciuria and bone resorption were reduced, suggesting that lower protein consumption might reduce bone loss.8 But as DiNicolantonio said:9
“Now don’t confuse this — I am not recommending nor do I think it is good to consume a low-protein diet. The object really, and what I do, is I consume a high animal protein diet. I just offset it with base, because we know low-protein diets aren’t good for bone health. So, you want to have a good protein intake.”
The Problem With a High Acid Load in Your Body
Diets high in animal proteins can produce excess acid in your body. To neutralize the excess acid, your body uses alkaline minerals, primarily calcium. This calcium is often mobilized from your bones, leading to a decrease in bone density over time. High acid levels also increase calcium excretion through urine, further depleting your body’s calcium reserves, which can exacerbate bone loss. DiNicolantonio explains:
“When we consume animal foods it forms a lot of hydrogen ions (H+) or acid in the body, which must be balanced with base (citrate or bicarbonate). If we don’t balance the acid with base, then the body must strip connective tissue and muscle to form ammonia so that the kidneys can eliminate the acid.
Additionally, producing ammonia to eliminate the acid is detrimental to the kidneys. Furthermore, the body will need more positively charged ions (like sodium, calcium, magnesium and potassium) to eliminate the negatively charged sulfate that comes from animal foods (animal foods contain a lot of sulfur-containing amino acids).
If you aren’t getting enough positively charged ions in your diet, then the body will strip bone for those alkaline minerals. Additionally, a high acid load in the body activates osteoclasts to break down bone and it lowers the pH in the interstitial fluid (the fluid that surrounds our cells), which can cause insulin resistance. In other words, if you don’t balance the acid from animal foods with base you can cause:
- Kidney damage
- Insulin resistance
- Bone breakdown
- Mineral loss
- Kidney stones”

Save This Article for Later – Get the PDF Now
Metabolic Acidosis Drives Chronic Disease
Metabolic acidosis happens when your body produces too much acid or your kidneys are not removing enough acid from your body. High intake of animal protein can increase the production of sulfuric acid due to the metabolism of sulfur-containing amino acids found in meat, poultry and fish. According to DiNicolantonio:10
“Metabolic acidosis is a chronic condition that many people in the Western world have but do not realize it … A normal healthy body has numerous buffering systems to combat acid accumulation.
However, if your buffering capacity is reduced or cannot meet the acid load, then harms can ensue such as a breakdown of muscle, connective tissue and bone … Animal protein is the largest source of dietary acid as it is high in the sulfur-containing amino acids methionine and cysteine, which leads to the formation of sulfuric acid and hydrogen ions in the body.”
Even low-grade metabolic acidosis can lead to:11
| Type 2 diabetes | Insulin resistance12 | Increased gluconeogenesis |
| High blood pressure | Bone loss | Osteoporosis and osteopenia |
| Sarcopenia | Muscle loss | Gout |
| Fibromyalgia | Declines in kidney function | Dehydration |
| Decreased exercise performance | Kidney stones | Mineral deficiencies |
DiNicolantonio points out that the average western diet leads to a net acid excretion of 50 to 100 milliequivalents (mEq) per day (milliequivalent measures the concentration of ions in a solution). However, “The kidneys of a healthy person can only excrete 40-70 mEq of acid per day before acid is retained in the body,” he says. “Most Americans are consuming diets that produce this much acid or more per day.”13
Further, “Animal-based or carnivore diets typically provide 150-250 mEq of acid per day, which means that these types of diets lead to significant acid retention unless exogenous bicarbonate forming substances are being consumed (bicarbonate mineral waters or supplements, fruits or vegetables).”14
How to Balance Dietary Acid With Base
What you eat affects your body’s acid base balance, and maintaining a diet that balances acid and alkaline foods can help protect your health.
“Animal protein, particularly, meat, eggs and cheese, is what leads to the formation of large amounts of acid in the body,” DiNicolantonio says. “Fruits and vegetables are high in organic anions like citrate, malate and gluconate, which get converted to bicarbonate in the body. Bicarbonate is the base in our body that neutralizes the acid.”15
While I don’t recommend vegan or vegetarian diets, including more fruits and vegetables, which are alkaline, can help counteract acid load. DiNicolantonio says, “I personally try to neutralize the acid from my diet by calculating how much acid is going to be produced from the foods I consume.” For example:
| Parmesan cheese: 34.2 | Other cheeses: 18-29 | Egg yolks: 23.4 |
| Processed meats: 10 to 13.2 | Fish: 10.8 | Chicken: 8.7 |
| Pork: 7.9 | Beef: 7.8 | Grains: 3.7 to 6.5 |
| Broccoli: -1.2 | Apples: -2.2 | Lemon juice: -2.5 |
| Potatoes/cauliflower: -4.0 | Zucchini: -4.4 | Carrots/celery: -5.0 |
| Bananas: -5.5 | Spinach: -14 | Raisins: -21 |
As a rule, protein should make up about 15% of your daily calories. More specifically, most adults need about 0.8 grams of protein per pound of ideal body weight (the weight you would ideally be, not necessarily the weight you are now), or for Europeans, approximately 1.76 grams of protein per kilo.
For example, if your ideal weight is 135 pounds, your protein requirement would be 108 grams. Divided into two meals, that would be 54 grams per meal. For reference, there’s approximately 7 grams of protein in each ounce of steak, so a 5-ounce steak would give you 35 grams of high-quality protein. For children, the average amount per meal is around 5 to 10 grams, while young adults typically can get away with 20 grams per meal.
For most normal-weight adults, 30 grams per meal is really the minimum you need to stimulate muscle protein synthesis. The key is to balance the acid load from animal foods in your diet with natural compounds that help neutralize the acid. In addition to fruits and vegetables, DiNicolantonio recommends:16
- Sodium citrate — 5 grams (g) suppresses 60 mEq of acid. Should be taken with food.
- Potassium citrate — 3 g suppresses 30 mEq of acid. Typically, no more than 3 g is taken with each meal.
- Bicarbonate mineral waters (low in sulfate) — 1 mEq of bicarbonate inhibits 1 mEq of acid. “Typically, the bicarbonate levels are fairly low and should not affect stomach pH. There is a slow accumulation of bicarbonate in the body when drinking bicarbonate mineral waters and this is a better option than sodium or potassium bicarbonate supplements.”
You can find more details in DiNicolantonio’s video overview of acid base balance.17
- 1 YouTube, Dr. James DiNicolantonio, High animal protein increases the propensity for negative calcium balance May 23, 2024
- 2 Journal of Biological Chemistry July 1, 1930, Volume 87, Issue 3, Pages 651-668
- 3 Atlas Obscura August 28, 2018
- 4 YouTube, Dr. James DiNicolantonio, High animal protein increases the propensity for negative calcium balance May 23, 2024, 5:38
- 5 Am J Kidney Dis. 2002 Aug;40(2):265-74. doi: 10.1053/ajkd.2002.34504
- 6 YouTube, Dr. James DiNicolantonio, High animal protein increases the propensity for negative calcium balance May 23, 2024, 12:46
- 7 Calcif Tissue Int. 1979 Nov 6;28(3):233-8. doi: 10.1007/BF02441241
- 8 J Clin Endocrinol Metab. 2004 Aug;89(8):3801-7. doi: 10.1210/jc.2003-032016
- 9 YouTube, Dr. James DiNicolantonio, High animal protein increases the propensity for negative calcium balance May 23, 2024, 21:29
- 10, 13, 14, 15 Open Heart 2021;8:e001730. doi: 10.1136/openhrt-2021-001730
- 11 Open Heart 2021;8:e001730. doi: 10.1136/openhrt-2021-001730, Box 2
- 12 Open Heart 2021;8:e001788. doi: 10.1136/openhrt-2021-001788
- 16 Open Heart 2021;8:e001730. doi: 10.1136/openhrt-2021-001730, Table 2
- 17 YouTube, Dr. James DiNicolantonio, Acid Base Balance: The Benefits of Sodium/Potassium Bicarbonate April 20, 2024