Antibiotics
now browsing by category
Common Drug Used by Pork Industry Has Human Cancer Risk
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/11/22/carbadox.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola November 22, 2023
STORY AT-A-GLANCE
- November 7, 2023, the U.S. Food and Drug Administration announced it is considering withdrawing approval for the antibiotic carbadox, which is added to pig feed to prevent infections and fatten up the animals, due to cancer concerns
- The drug has been banned in the European Union since 1999, and in Canada since 2006. China, Brazil, Australia and the UK have also banned it due to concerns over its cancer risks
- In 2014, the United Nation’s Codex Committee on Residues of Veterinary Drugs in Foods determined that there is no safe level of residues of carbadox or its metabolites in food that represents an acceptable risk to consumers
- Carbadox has been shown to cause liver cancer and birth defects in lab animals, and have long-lasting impacts on the gut microbiome of swine, even after the drug is withdrawn
- A 2017 study found carbadox induced transducing bacteriophages with resistance genes to tetracycline, aminoglycoside and beta-lactam antibiotics — three classes of drugs that are commonly used in human medicine. The findings effectively dismisses the drugmaker’s and the National Pork Producers Council’s argument that since carbadox is not used in human medicine, it won’t contribute to drug resistance in humans
Livestock raised in confined animal feeding operations (CAFOs) are routinely given a range of veterinary drugs to prevent disease, and some of those drugs could potentially impact the health of those who eat their meat.
November 7, 2023, the U.S. Food and Drug Administration announced it is considering withdrawing approval for the antibiotic carbadox1 (brand name Mecadox), which is added to pig feed to prevent infections and fatten up the animals, due to cancer concerns. As noted in the Federal Register:2
“The Food and Drug Administration … Center for Veterinary Medicine (CVM), is proposing to withdraw approval of all new animal drug applications (NADAs) providing for use of carbadox in medicated swine feed …
This action is based on CVM’s determination that there is no approved regulatory method to detect the residue of carcinogenic concern in the edible tissues of the treated swine.”
How a Carcinogen Ended Up Being Used for Decades
Under the Delaney Clause in Section 512 of the Federal Food, Drug, and Cosmetic Act, an animal drug cannot gain FDA approval if it has been found to “induce cancer when ingested by man or animal.” In the case of carbadox, the drug was known to cause liver cancer3 and birth defects4 in lab animals.
CVM still approved it under an exception to the Delaney Clause, known as the Diethylstilbestrol “DES” Proviso, which allows a carcinogenic drug to be approved if, under the conditions for use, the drug is found to not have an adverse effect on the animals being treated, and if no drug residues can be found “by an approved regulatory method in any edible tissues of, or food from, the animal.”5 As explained by the FDA:6
“In 1998, the FDA’s Center for Veterinary Medicine (CVM) approved the most recent testing method for carbadox based on information available to CVM at that time.
The method relied on measuring the noncarcinogenic residue quinoxaline-2-carboxylic acid (QCA) as a marker to demonstrate when the residue of carcinogenic concern in the edible tissue of carbadox-treated animals dropped to a level that satisfied the DES Proviso.
However, subsequent information showed that carcinogenic residues of carbadox persist longer than previously known. This means that noncarcinogenic QCA is not a reliable marker …
Specifically, because there is no established relationship between noncarcinogenic QCA measured by the 1998-approved method and the residue of carcinogenic concern, the 1998-approved method does not allow FDA to determine whether the residue of carcinogenic concern can be found in any edible tissue of, or food derived from, the treated animals.
Accordingly, in November 2023, FDA revoked the 1998-approved method. There is currently no approved method for carbadox. Without an approved method, the second prong of the DES Proviso exception to the Delaney Clause, which requires that ‘no residue of such drug will be found …, in any edible portion of such animals after slaughter or in any food yielded by or derived from the living animals,’ is not met.”
Action Long Overdue
The thing is, FDA has known the original testing method was inadequate for seven years, if not more. In its 2016 proposal to withdraw the drug, the FDA even noted that:7
“Continued approval of carbadox would expose humans to concentrations of total residues of carcinogenic concern that are approximately 30 times higher (for the approved 42-day withdrawal period) or 11 times higher (for the approved 70-day withdrawal period) than the 0.915 ppb concentration of total residues of carcinogenic concern in liver that would be considered safe.”
Mind you, two years before that, in 2014, the United Nation’s Codex Committee on Residues of Veterinary Drugs in Foods determined that “there is no safe level of residues of carbadox or its metabolites in food that represents an acceptable risk to consumers.”8
There is no safe level of residues of carbadox or its metabolites in food that represents an acceptable risk to consumers. ~ UN Codex Committee on Residues of Veterinary Drugs in Foods
Still, nothing happened. It’s unclear why the agency didn’t follow through to remove the drug in 2016. The European Union banned carbadox in 1999 and Canada followed suit in 2006.9 The drug has also been banned in China, Brazil, Australia and the U.K.
According to the National Pork Producers Council, removal of the drug could result in millions of pigs being lost to swine dysentery, for which the drug is being used. However, if carbadox is so essential, how are the pork industries in the EU, Canada and China surviving? Clearly, there must be other alternatives available.

Download this Article Before it Disappears
Carbadox Has Long-Lasting Impact on Swine Gut
While carbadox does not appear to cause cancer in pigs, it has been shown to have long-lasting impacts on their gut microbiome. As reported in a 2014 study:10
“Six pigs (initially 3-weeks old) received feed containing carbadox and six received unamended feed. After 3-weeks of continuous carbadox administration, all pigs were switched to a maintenance diet without carbadox. DNA was extracted from feces (n = 142) taken before, during, and following (6-week withdrawal) carbadox treatment.
We found that carbadox altered bacterial membership and community structure relative to non-medicated pigs, including a reduction in total bacteria … [R]esults show that the swine gut bacterial community changes over time, and that carbadox influences these microbiotas even several weeks after its removal.”
Carbadox May Confer Antibiotic Resistance to Humans
A 2017 study11 by Johnson et al. confirmed that carbadox has profound effects on the gut microbiome of swine. Importantly, they also found the drug induced transducing bacteriophages with resistance genes to tetracycline, aminoglycoside and beta-lactam antibiotics — three classes of drugs that are commonly used in human medicine.
Bacteriophages have been described as “the viruses of bacteria,”12 in that they infect cells and mediate horizontal gene transfers by ejecting bacterial DNA. Commenting on the finding, Lance Price with the Milken Institute School of Public health wrote:13
“[The] findings underscore the potential unforeseen consequences of using antibiotics in livestock production and call into question our current methods for classifying whether or not a veterinary drug has relevance to human health …
[T]here are drugs that are used exclusively in livestock, such as the third-generation cephalosporin ceftiofur or … enrofloxacin. These two drugs … are never used in human medicine, but bacteria that evolve resistance to these drugs are also resistant to their human medicine analogs, ceftriaxone and ciprofloxacin, respectively.
Large-scale, real-world studies have demonstrated that veterinary use of these antimicrobials can lead to resistant infections in people … Beyond these shared analogs, there are those that belong to antibiotic classes that are used exclusively in food animals, including ionophores and … carbadox …
Carbadox has a checkered history in livestock production … Because it is not considered medically important in human medicine, the drug can be used in livestock without veterinarian oversight …
However, the study by Johnson et al. indicates that using carbadox in food animals may not only increase the risk for cancer and birth defects, but it may also fuel the transmission of phage-encoded antimicrobial resistance genes. Carbadox is genotoxic and mutagenic and thus a potent inducer of the SOS pathway and prophage …
Paradoxically and relevant to the question of whether carbadox should be considered medically important, some of the transferred genes coded for resistance to antibiotic classes that are commonly used in human medicine, including tetracyclines, aminoglycosides, and beta-lactams …
[I]n actual production settings, the drug would frequently be accompanied or immediately followed by other antibiotics. For some applications, the drug sponsor actually recommends using carbadox in conjunction with oxytetracycline, which would likely fuel the expansion of bacterial populations that acquire tetracycline resistance genes as a result of the carbadox-induced phage transmission.
Future studies will have to be conducted to determine whether carbadox acts synergistically with other drugs to encourage the rapid emergence of pathogens resistant to the antibiotics administered along with carbadox.”
Johnson et al.’s findings effectively dismisses the drugmaker’s and the National Pork Producers Council’s argument that since carbadox is not used in human medicine, it won’t contribute to drug resistance in humans.
Other Potentially Hazardous Swine Drugs
Aside from carbadox, which is used in about 40% of hogs raised in the U.S.,14 many herds are also routinely treated with customizable mRNA-based “vaccines.” Considering health authorities insist the COVID shots are safe, it’s no wonder they also insist there are no problems associated with eating mRNA-treated meat. But can we trust them?
Livestock such as swine are routinely vaccinated against several diseases,15 and many of these vaccines must be administered at specific times to ensure there’s no residue left in the meat. When using the mRNA platform, however, there’s no time limit. So, just when are swine receiving these customized mRNA shots? And could there be mRNA in the pork you buy?
Vaccines are nearly always given in the hindquarter of the animal, and according to mRNA jab developers, the mRNA remains at the injection site. This theory has long since been proven false, as the mRNA in the COVID jab gets has been shown to be distributed throughout the human body.
But it makes sense that the mRNA might be more concentrated at the injection site. In livestock, this could be bad news, seeing how the hindquarters are usually where the prime cuts of meat come from.
So, knowing whether there’s any mRNA left in the animal at the time of slaughter is important. At present, we have no way of knowing this. We don’t even know exactly how long the synthetic lipid-enveloped mRNA stays in the body.
We also don’t know how long the antigen produced by the animal’s cells in response to a customized mRNA shot sticks around, and whether ingesting that antigen might have repercussions for human health.
Stanford researchers found the spike protein produced in response to the COVID shot remains in the human body for at least 60 days,16,17 and the spike protein is what’s causing most of the health problems associated with the jab.
Could the same be true for mRNA jabs used in animals? Hogs can be killed anywhere from the age of 6 weeks to 10 months, which doesn’t allow a whole lot of time for the mRNA and/or antigen to get flushed out.18
Due to the uncertainties involved, I strongly recommend avoiding pork products. Pork is also very high in linoleic acid, a harmful omega-6 fat that drives chronic disease, which is yet another reason to avoid it.
- 1, 5, 6 FDA Carbadox Q&A
- 2 Federal Register November 7, 2023
- 3 WHO, Carbadox 2003
- 4, 13 mBio September-October 2017; 8(5): e01490-17
- 7 Federal Register April 12, 2016
- 8 FDA April 8, 2016, Download the linked Codex Committee Report, page 38
- 9 Consumerfed.org February 28, 2022 Letter to FDA Commissioner
- 10 Frontiers in Microbiology 2014; 5: 276
- 11, 14 mBio August 8, 2017; 8(4):e00709-17
- 12 PLoS Pathogens August 2019; 15(8): e1007878
- 15 Swine Vaccine Protocol
- 16 Cell January 24, 2022; 185(6): 1025-1040.E14
- 17 Clark County Today February 14, 2022
- 18 FAO Meat Cutting
Nourishing Gut Bacteria Is Critical for Health, Well-Being
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/08/13/nourishing-gut-bacteria.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked August 13, 2023
STORY AT-A-GLANCE
- One of the best and least expensive ways to optimize your gut microbiome is to eat traditionally fermented and fiber-rich foods. Probiotic supplements can also be beneficial
- One of the reasons a healthy diet is able to influence your health is by creating an optimal environment for beneficial bacteria in your gut, while decreasing pathogenic or disease-causing bacteria, fungi, and yeast
- If you have to take an antibiotic, be sure to also take a high-quality probiotic. To ensure the bacteria’s survival, take the probiotic a few hours before or after taking the antibiotic
Editor’s Note: This article is a reprint. It was originally published March 13, 2016.
Barely a day goes by without some type of media announcement noting the importance of your gut flora.
One of the best and least expensive ways to optimize your gut microbiome is to eliminate sugars and processed sugars and eat traditionally fermented foods, but probiotic supplements can also be beneficial.
Greg Leyer,1 who has a Ph.D. in food microbiology, is head of scientific affairs at Chr Hansen, a global, differentiated bioscience company that develops natural ingredient solutions for the food, nutritional, pharmaceutical and agricultural industries, and he’s been passionate about probiotics and health for more than two decades:2
“I got interested in microbiology and spent my graduate research career looking at pathogenic bacteria, those bacteria we want to avoid and that make us sick,” he says.
“In the course of doing those studies, I became aware that not all bacteria are bad and became intrigued in this whole concept of probiotics … My first post-graduate job was in the area of developing probiotics for infant nutrition. That was 21 years ago.
I’ve been in the probiotic research development field ever since, and have seen the clinical research and the market just explode.”
Nourishing Your Microbiome Begins With Real Food
Mounting evidence reveals there’s more to nutrition than previously thought — a large component of it actually revolves around nourishing the health-promoting bacteria in your body, thereby keeping harmful microbes in check.
Probiotics are supplements designed to increase your beneficial bacteria, the largest concentration of which is found in your gut. Different types of bacteria live in different locations in your gastrointestinal tract. You also have bacteria residing in other areas of your body, such as your mouth and skin.
While probiotic supplements have their benefits and their place, it’s important — before taking a supplement — to optimize the conditions where these beneficial bacteria grow.
One of the reasons a healthy diet is able to influence your health is by the fact that it helps create an optimal environment for beneficial bacteria in your gut, while decreasing pathogenic or disease-causing bacteria, fungi, and yeast.
“Healthy eating” basically amounts to eating real food, which means avoiding processed foods and staying away from sugars, because few things fertilize and accelerate the growth of pathogenic microbes better than sugar. As noted by Leyer:
“In studies done in people all over the world, you’ll see different microbial communities residing in people that have different dietary intakes. You want to provide foods that are going to nourish this healthy community of bacteria in your gastrointestinal tract.
Sugars aren’t selective. Bacteria like sugars, but the bad bacteria love sugars. Eating real food, complex carbohydrates, fiber, and things like that, are more selective. Simply put, the pathogenic bacteria don’t utilize non-fiber carbs as efficiently. It’s more difficult for them to grow with complex carbohydrates as an energy source.”
The Importance of Probiotics When Taking an Antibiotic
Unfortunately, the U.S. Food and Drug Administration restricts supplement makers from making certain health claims; for example, you cannot market a probiotic saying, “This is useful to take after an antibiotic,” because that would imply that antibiotics might harm you in some way.
As a result of these restrictions, unless you spend a fair amount of time reading about the subject you may not be aware of many of the benefits of probiotics.
“There’s a lot of very compelling research that we’re not able to talk about on a product label,” Leyer notes. “One of the exciting areas is the role of healthy bacteria when co-prescribed with an antibiotic, and the effect it has on maintaining healthy populations in your gut.
Antibiotics are selective for bacteria and not viruses, but they’re not terribly selective for a particular type of bacteria. Antibiotics — and many studies have shown this — will have a tremendously disruptive effect on the overall microbial community.
They’ll kill the target organism that might be causing your infection which is a good thing … but they also do a lot of harm to the good bacterial populations that are there.
Studies have shown that when you co-administer probiotics with antibiotics and continue the probiotic administration even after stopping the antibiotic regimen, you’re quickly able to restore that microbial community to the healthy state it was prior to the antibiotic treatment.”

Download this Article Before it Disappears
Guidelines for Taking Probiotics With Antibiotics
If you’re taking an antibiotic, don’t simultaneously take the probiotic as the antibiotic is liable to simply kill the bacteria off. Instead, take them a few hours before or after taking the antibiotic. From the clinical research Leyer has done, this strategy appears to work quite well.
Saccharomyces yeast, a beneficial type of yeast, may also be helpful when taking a course of antibiotics, as it has also been shown to prevent antibiotic-associated diarrhea.
“Fifteen to 25% of people who take an antibiotic end up getting antibiotic-associated diarrhea.
Probiotics — I’ll include Saccharomyces in this group — have been shown to have tremendous benefits in reducing the risk of developing that kind of secondary complication of antibiotic treatment,” Leyer says.
The Hazards of Antibiotics in the Food Supply
Medical antibiotics are not the sole source of exposure. About 80% of all antibiotics sold in the U.S. are actually used in livestock production to fatten up the animals and prevent disease.
So, unless you’re buying organic grass-fed meats, you’re likely ingesting minute doses of antibiotics with each hamburger and steak you eat. This continuous low-dose exposure has the added downside of promoting antibiotic resistance. The role of antibiotics in promoting (rather than treating) disease is slowly gaining ground.
There’s no question that antibiotics have saved lives. But if you were to carefully analyze and objectively determine their true impact, you just might find they’ve done more harm than good. Leyer cites the book “Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues,” written by Dr. Martin Blaser, which presents the theory that many of our modern disease epidemics may be rooted in the disruptive effect modern foods have on our microbiota.
“Keeping your intestinal microflora healthy, consuming healthy, active, probiotic bacteria is a key component to maintaining, in my opinion, your overall health,” Leyer says.
Probiotics for the Prevention of Leaky Gut, and More
Leaky gut results when there’s a disruption in the interconnections between the cells in your intestines. Little holes or tears can develop, allowing food particles to enter your blood stream, which can cause an autoimmune response.
It’s a serious problem, and I’ve known a number of people who nearly died from it. There are a number of causes for leaky gut, but whatever the cause, one of the most powerful remedies is to consume homemade organic bone broth and fermented vegetables. Certain probiotic supplements can also be helpful. According to Leyer:
“I am familiar with the evidence behind certain probiotics and their ability to prevent or lessen leaky gut. The issue with leaky gut is that you’re getting things into the circulation system that aren’t supposed to be there. Lipopolysaccharides (LPS) … are inflammatory components from gram-negative bacteria … [LPS] is a diagnostic test to look for leaky gut.
What we’re finding is that subchronic levels of LPS circulating in the blood causes this chronic inflammation cascade. Chronic inflammation seems to be at the root of a lot of disease states … One that is front and center is Type 2 diabetes and insulin resistance.
There’s been some really intriguing work with probiotics maintaining tight-junction barrier, reducing leaky gut, reducing circulating LPS, and affecting insulin sensitivity through downplaying this inflammation.”
Probiotics have also been extensively tested for their immunological functions. For example, in the elderly, probiotics can help boost activity of immune cells that fight off cancer cells. The mechanism involved here is an orchestration of immune chemical messengers called cytokines. But there’s still much to be learned about the exact mechanisms by which probiotics influence health.
“There are some areas in the probiotic science where the mechanisms are becoming better understood. And there are some areas in probiotic science that is more theory than really causal right now.
But the more layers of the onion you peel back, the more you understand this is an incredibly complicated web of information from gut to human, to nervous system to immune system. This complex interplay is at the heart of probiotic mechanisms and one reason it is not so simple to clearly identify.” Leyer explains.
Probiotics and the Gut-Brain Axis
It’s become quite clear that the benefits of probiotics transcend the gut. More recent studies have delved into the role of gut bacteria in the workings of the gut-brain axis, and how they benefit your mental and psychological health. Anxiety, depression and other mood disorders are increasingly recognized as being, in part, related to an unbalanced microbiome.
Probiotics appear to have the ability to make compounds called neuropeptides that interact directly with your brain. Probiotics certainly influence your immune system by way of modulating inflammation, which has interactions with and can cross the blood-brain barrier.
“There’s an interesting study where people gave infants probiotic bacteria for the first two years of their life,” Leyer says. “They were really looking at the ability of this probiotic to ward off the incidence of atopic eczema or skin rashes.
When the kids were 13 years old, they went back and said, ‘Okay. Let’s look at autistic spectrum disorder, attention-deficit hyperactivity disorder (ADHD), and [other] psychological kind of issues and ask if there is a relationship between those children who were administered the probiotic early in life, and incidence.’
Of the kids that took the probiotic, none had developed any kind of autistic spectrum disorders; 17% of those that did not get probiotics developed autistic spectrum disorders. The study wasn’t designed to look at ADHD or autism, but it’s an interesting way to look back in time and say:
Here’s a population of people that were essentially imprinted with probiotic bacteria at a very young age. We now understand better that there’s this developmental window in young people that’s critically important for longer term health.”
Beware of ‘Probiotic’ Junk Food
As a general rule, I believe most people would be able to obtain most of their nutritional support from real food. This is certainly the case with beneficial bacteria, because there are a lot of good fermented foods that provide them.
One of my biggest pet peeves when it comes to probiotic foods is yogurt, because most of them are nothing more than creamy junk food. The Cornucopia Institute has published a Yogurt Buyer’s Guide and Scorecard3,4 where you can learn more about your favorite brands.
Many who seek to improve their health buy commercial yogurt from the grocery store, thinking they’re doing something good for themselves when in reality they’re not. They’d be far better off taking a probiotic supplement, as then they’d avoid added sugars and other unhealthy additives. The exception to that rule is traditionally cultured yogurt made from organic raw milk.
Commercial yogurts often contain upwards of 25 to 30 grams of sugar per serving, which meets or exceeds the daily recommended amount of sugar for the whole day!
The amount of probiotics you’ll get from commercial yogurt is also far lower than what you’d get from a high-quality probiotic supplement. A commercial yogurt might give you a million probiotic cells, which sounds like a lot, but if you take a quality-made supplement you’re getting tens of billions of probiotics — three orders of magnitude greater amounts. So in that respect, a supplement is clearly easier and more cost-effective.
“The other thing you have to consider is that in a yogurt, you’ve got a very acidic condition that’s degrading the quality of the probiotics over the course of the shelf life of that yogurt. In a quality-made dietary supplement, these probiotics are essentially in suspended animation or dormant until you consume them; they come back to life when you swallow the capsule.” Leyer notes.
Probiotic Guidelines
Many tend to imagine that taking probiotics is like planting seeds in your garden. They grow, reproduce, and all you basically have to do is “seed and feed” them. But that’s actually not the case. Your intestinal tract contains thousands of different bacterial types, not to mention fungi and viruses. It’s a challenging environment with lots of competition.
Probiotics have developed the ability to withstand normal concentrations of stomach acid and bile in the small intestine, and live there, but they don’t live and thrive there forever. As noted by Leyer:
“When you stop taking the probiotics, studies show that you start seeing less and less of that probiotic residing there. It will decline to this baseline level similar to where it was before you started taking a probiotic supplement.
On the immune side, there are studies that show that immune benefits decline within a few days after stopping taking the probiotics. So it’s really important to maintain a continual onslaught of these healthy bacteria.”
Factors to look for when trying to identify a high-quality probiotic supplement include the following:
| Make sure it’s a reputable brand. If you trust the products made by a company, perhaps they’re doing a great job making their probiotics as well. |
| Look for a potency count (colony forming units or CFUs) of 50 billion or higher. That’s the number of bacteria being delivered per dose. |
| Declaration of shelf life, i.e. the shelf life of the CFUs. Avoid capsules that only declare the CFUs at time of manufacture. Food products should be in resealable packaging and stored as directed. |
| Look for a product containing multiple species of bacteria, as high diversity tends to be associated with better health. That said, products containing species of Lactobacillus and Bifidobacteria are generally recommended.
Examples would be Lactobacillus acidophilus and Lactobacillus plantarum. These organisms predominantly reside in the small intestine or the upper gastrointestinal tract (GI) where a vast majority of your immune cells reside. Bifidobacteria, on the other hand, reside in the large intestine or the lower bowel, which is another critical location associated with health. Bifidobacterium lactis, Bifidobacterium longum, and Bifidobacterium bifidum are important ones. |
| Look for non-GMO brands. |
| Confirm that they’re manufactured according to current Good Manufacturing Practices (cGMP).5 |
Optimize Your Microbiome for a Disease Prevention Strategy
As noted by Leyer, “probiotic consumption for health and wellness is here to stay.” A tremendous amount of research shows that the microbial community in your body has a wide ranging influence over your health. “The days of ‘all bacteria are bad’ are long gone,” Leyer says. “Eating clean and natural foods, nourishing your gut, and having a healthy intestinal community are really at the core of wellness.”
I also firmly believe that applying this knowledge can make a distinct and positive difference in your health, boosting not only your immune function, but also your neurological function and mood. Best of all, supporting your microbiome isn’t very complicated. You do need to take proactive steps to implement certain key strategies while actively avoiding other factors though. So to optimize your microbiome, consider the following recommendations:
| Do | Avoid |
|---|---|
| Eat plenty of fermented foods — Healthy choices include lassi, fermented grass-fed organic milk such as kefir, natto (fermented soy), and fermented vegetables. | Antibiotics, unless absolutely necessary, and when you do, make sure to reseed your gut with fermented foods and/or a high quality probiotic supplement.6,7 |
| Take a probiotic supplement — Although I’m not a major proponent of taking many supplements (as I believe the majority of your nutrients need to come from food), probiotics is an exception if you don’t eat fermented foods on a regular basis. | Conventionally-raised meats and other animal products, as CAFO animals are routinely fed low-dose antibiotics, plus genetically engineered grains loaded with glyphosate, which is widely known to kill many bacteria. |
| Boost your soluble and insoluble fiber intake, focusing on vegetables, nuts, and seeds, including sprouted seeds. | Chlorinated and/or fluoridated water — Especially in your bathing such as showers, which are worse than drinking it. |
| Get your hands dirty in the garden — Exposure to bacteria and viruses can serve as “natural vaccines” that strengthen your immune system and provide long-lasting immunity against disease.
Getting your hands dirty in the garden can help reacquaint your immune system with beneficial microorganisms on the plants and in the soil. According to a 2014 report,8 lack of exposure to the outdoors can in and of itself cause your microbiome to become “deficient.” |
Processed foods — Excessive sugars, along with otherwise “dead” nutrients, feed pathogenic bacteria.
Food emulsifiers such as polysorbate 80, lecithin, carrageenan, polyglycerols, and xanthan gum also appear to have an adverse effect on your gut flora.9 Unless 100% organic, they may also contain GMOs that tend to be heavily contaminated with pesticides such as glyphosate. Artificial sweeteners have also been found to alter gut bacteria in adverse ways.10 |
| Open your windows — For the vast majority of human history the outside was always part of the inside, and at no moment during our day were we ever really separated from nature.
Today, we spend 90% of our lives indoors. And, although keeping the outside out does have its advantages it has also changed the microbiome of your home. Research11 shows that opening a window and increasing natural airflow can improve the diversity and health of the microbes in your home, which in turn benefit you. |
Agricultural chemicals, glyphosate (Roundup) in particular is a known antibiotic and will actively kill many of your beneficial gut microbes if you eat foods contaminated with Roundup. |
| Wash your dishes by hand instead of in the dishwasher — Research has shown that washing your dishes by hand leaves more bacteria on the dishes than dishwashers do, and that eating off these less-than-sterile dishes may actually decrease your risk of allergies by stimulating your immune system. | Antibacterial soap, as they too kill off both good and bad bacteria, and contribute to the development of antibiotic resistance. |
- 1 Greg Leyer
- 2 The Power of Probiotics Mercola Transcript
- 3 Cornucopia Institute Yogurt Buyers Guide
- 4 Cornucopia Institute Yogurt Report November 19, 2014
- 5 FDA.gov, Current Good Manufacturing Practices
- 6 Science News March 19, 2015
- 7 Cell Reports March 19, 2015 [Epub ahead of print]
- 8 BBC News August 26, 2014
- 9 Time February 25, 2015
- 10 Scientific American March 17, 2015
- 11 ISME Journal 2012 Aug;6(8):1469-79
Two-Thirds of Appendectomies May Be Unnecessary
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/08/11/appendectomy-alternatives.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked August 11, 2023

STORY AT-A-GLANCE
- Appendectomy is the most common emergency surgery performed in the U.S. Many doctors will even suggest prophylactic removal of the appendix when you’re having some other abdominal surgery done
- With the help of white blood cells known as innate lymphoid cells, the appendix acts as a reservoir for beneficial bacteria
- Once your body has successfully fought and rid itself of a gut infection, the bacteria emerge from the biofilm of the appendix to recolonize your intestines
- Research suggests nearly two-thirds of patients with appendicitis can be successfully treated with antibiotics alone
- In an earlier study, only two of 77 participants who received antibiotics ended up requiring surgery within 24 hours, and only one-third of participants needed an appendectomy after being discharged, due to lack of improvement
Editor’s Note: This article is a reprint. It was originally published October 17, 2018.
You’ve probably heard that your appendix is a useless organ, an artifact from our ancient past when early humans had to digest tree bark and other fibrous materials.1 However, modern medical science has again proven your body does not contain superfluous organs that serve no useful function.
Unfortunately, the idea that your appendix is little more than a nuisance and potential health risk has led to the routine removal of this organ. Many doctors will even suggest prophylactic removal of the appendix when you’re having some other abdominal surgery done. As noted in a 2017 paper:2
“Appendectomy is the most common emergency surgery performed in the USA. Removal of a noninflamed appendix during unrelated abdominal surgery (prophylactic or incidental appendectomy) can prevent the downstream risks and costs of appendicitis. It is unknown whether such a strategy could be cost saving for the health system.”
Based on hypothetical patient cohorts aged 18 to 80, the researchers concluded that people under the age of 30 could save about $130 over their lifetime by undergoing prophylactic appendectomy during other elective abdominal surgery. However, considering the potential benefits of keeping your appendix, saving $130 over a lifetime doesn’t seem very good value proposition.
Your Appendix Has an Immune Function
Your appendix is found in the lower right portion of your abdomen. This small, slimy, finger-shaped organ is attached to the cecum, a small pouch that’s part of the intestines (the cecum is considered to be the beginning of the large intestine) and is part of your gastrointestinal tract.3
According to scientists in France and Australia, your appendix actually plays an important role in your immunity. Published in Nature Immunology, their study showed that the appendix — with the help of white blood cells known as innate lymphoid cells (ILCs) — works as a reservoir for beneficial bacteria (probiotics), which are essential for good gut health and healing from infections.4
When certain diseases (or use of antibiotics) eliminate the healthy bacteria in your gut, the appendix works as a storage unit for some of these probiotics. The researchers say that these findings should make people rethink whether the appendix is “irrelevant” to their health.
Once your body has successfully fought and rid itself of the infection, the bacteria emerge from the biofilm of the appendix to recolonize your gut, bringing it back to a healthy state. According to Gabrielle Belz, a professor at Melbourne’s Walter and Eliza Hall Institute:5
“We’ve found that ILCs may help the appendix to potentially reseed ‘good’ bacteria within the microbiome — or community of bacteria — in the body. A balanced microbiome is essential for recovery from bacterial threats to gut health, such as food poisoning.”
Despite such findings, other research6 suggests prophylactic appendectomy “is ethically justifiable, as there are few complications,” and “allows early detection of malignancies.” In this case, 10 cases of cancer were found as a result of prophylactic appendectomy on 173 patients.
In the end, it may be an issue of personal choice after considering the pros and cons of removing this organ. Personally, I believe having the ability to repopulate your gut with beneficial bacteria after infection is a significant health benefit that I would be reluctant to eliminate unless absolutely necessary. And, research suggests surgery may not even be necessary in most cases of appendicitis either.
Two-Thirds of Appendicitis Cases Do Not Require Surgery
According to a Finnish study,7,8,9,10 nearly two-thirds of patients with appendicitis can be successfully treated with antibiotics alone. In the U.S., an estimated 300,000 appendectomies are performed each year, which means some 199,800 people undergo surgery unnecessarily.
Not that antibiotics are without their side effects in damaging the microbiome, but it appears to be the lesser of two evils in this setting. Overall, the lifetime risk of appendicitis in the U.S. is 1 in 15.11 As reported by Live Science:12
“The study looked at data from more than 250 adults in Finland who had appendicitis … and were treated with antibiotics. This group was compared with another 270 adults who had surgery for appendicitis. All of the participants were followed for five years.
At the end of the study, nearly two-thirds of people who received antibiotics (64 percent) were considered ‘successfully treated,’ meaning they didn’t have another attack of appendicitis. The other 36 percent eventually needed surgery to remove their appendix, but none of them experienced harmful outcomes from the delay …
It’s important to note that all patients in the study had uncomplicated appendicitis, meaning their appendix had not burst, which was confirmed with a CT scan. (Patients with a burst appendix would indeed need surgery.)”
In an accompanying editorial,13 deputy editor of JAMA, Dr. Edward Livingston, noted that these findings “dispel the notion that uncomplicated acute appendicitis is a surgical emergency.”
Interestingly, of the 100 patients in the antibiotic group that later went on to have surgery anyway, seven of them actually had no evidence of appendicitis at the time of surgery — a finding that hints at underlying skepticism and an ingrained idea that it’s better to just take the appendix out to be done with it once and for all.

Download this Article Before it Disappears
Pros and Cons of Antibiotic Treatment
The antibiotic treatment group also had fewer complications than the surgical intervention group — about 1 in 4 surgical patients suffered some sort of postoperative complication, ranging from abdominal pain to surgical wound infections — and those who received antibiotics took on average 11 fewer days off from work (surgical patients took on average 22 days off from work).
Cost is also a factor, as surgery is far more expensive than a round of antibiotics. In this study, antibiotic treatment consisted of intravenous antibiotics for three days, followed by oral antibiotics for seven days.
On the downside, antibiotic treatment for suspected appendicitis could exacerbate the emergence of drug-resistant superbugs, so wanton use of antibiotics is not necessarily ideal either. Dr. Paulina Salminen, a surgeon at the University of Turku in Finland who led the study, told The New York Times:14
“If I have a CT scan, and I can see that the appendicitis is uncomplicated, I would discuss with the patient the possible results of antibiotic treatment alone or surgery. Then we would make a joint, unbiased decision about what would be best.”
Other Supporting Research
This isn’t the first time researchers have found antibiotics can do the job well enough that surgery becomes unnecessary. A 2014 study15 published in the Journal of the American College of Surgeons reviewed 77 uncomplicated cases of acute appendicitis that met certain criteria.
Here, 30 of the patients were given intravenous antibiotics for 24 hours and oral antibiotics for a week instead of surgery. Those whose condition did not improve after the first 24 hours had their appendix removed surgically at that time.
Of the 77 participants, only two required surgery within 24 hours, while a third needed an appendectomy after being discharged due to lack of improvement. However, none of the patients experienced complications.
The other 27 participants who received antibiotics missed fewer days of school and went back to their normal activities much sooner than those who underwent an appendectomy.
Nationwide Children’s Hospital professor of surgery and senior study author Dr. Katherine J. Deans said,16 “It’s so dogmatic to operate for appendicitis that it requires a huge paradigm shift. But there are choices. It may be safe to wait.”
Signs and Symptoms of Appendicitis
While the proper course of treatment may be up for debate, what’s clear is that appendicitis can be a serious condition that needs to be addressed. In short, appendicitis is inflammation in the appendix, usually caused by pathogenic bacteria.
Once these harmful bacteria multiply rapidly, it can lead to swelling and formation of pus in the organ.17 Hallmark symptoms of appendicitis include intense and progressively worsening pain in the lower, right-side quadrant of your torso, nausea and vomiting. It can occur at any age, although people ages 10 to 30 tend to be more susceptible.18
If you suspect that you or someone you know is suffering from an inflamed appendix, do seek immediate medical attention. If not addressed, the swollen appendix can rupture and may be fatal.
Just remember that surgical intervention may not be necessary if you have a case of uncomplicated appendicitis. A round of antibiotics may be enough. In this case, also remember to restore the balance of your gut microbiome with a high quality probiotic supplement, after you’ve finished the antibiotics.
Surgical Alternatives
When it comes to surgery, there are two main types of appendectomy,19 both of which are performed under general anesthesia. Depending on the progression of the inflammation and the condition of your appendix, your doctor will determine which of these two will be preferable:20
• Laparoscopy — Also known as “keyhole surgery,” this is the preferred procedure today because of its quicker recovery time. It is also recommended for obese or elderly patients.21 In the Finnish study above, all surgeries were open; hence the extended recovery time (22 days) among the surgical patients.
Three or four small incisions are made on the abdomen, and then special instruments and small surgical tools are inserted and used to remove the appendix. Afterward, dissolvable stitches (or regular ones that your physician will have to remove after several days) will be used to close the incisions.
• Open surgery — If the appendix has already ruptured, if you’ve previously had an open abdominal surgery or if your physician isn’t experienced in keyhole surgery, this is the recommended procedure.
A single, larger incision is done in the lower right side of your abdomen, so the appendix can be removed. However, if peritonitis (infection of the abdominal lining) has already occurred, a long cut in the middle of the abdomen may be necessary. This is called laparotomy.
Normal activities can be resumed in a couple of weeks, but strenuous activities must be avoided for four to six weeks after the surgical procedure to allow enough time for your body to heal. As with any surgical procedure, an appendectomy can still predispose you to certain risks and complications, such as bleeding, infection, injury to other organs, blocked bowels and side effects of general anesthesia.
Natural Treatments for Appendicitis
There are some natural techniques that can help you deal with the pain that comes with appendicitis, but remember that you should not rely on these solely to treat this condition. They should only be used as an adjunct and with the approval of your physician. Natural remedies that may be useful when the infection is detected at an early stage include:22,23
| Castor oil pack — This can help relieve the appendiceal blockage and reduce inflammation. To prepare this, simply fold a large cloth, pour 2 tablespoons of castor oil on it and then apply it to your abdomen while lying down.
You can repeat this three times a week for two or three months. Taking castor oil orally may also help relieve constipation and improve bowel movements. |
| Ginger — This root can reduce inflammation and pain, while alleviating vomiting and nausea. Drink fresh ginger tea twice or thrice daily or massage ginger oil on your abdomen for a few minutes daily. |
| Garlic — It’s a potent anti-inflammatory that can alleviate inflammation and pain. Eat two to three raw cloves on an empty stomach per day. |
| Fenugreek seeds — They help prevent the intestinal waste and excess mucus from accumulating, which can reduce the risk of the problem becoming severe. Fenugreek seeds also help alleviate pain. |
| Fresh lemon — Mixed with a small amount of honey, lemon helps prevent indigestion and constipation, relieves pain and boosts your immunity. |
| Basil — It helps bring down the fever that may come with appendicitis. It’s also great for relieving indigestion and intestinal gas. Boil a handful of fresh basil leaves with a teaspoon of grated ginger and then drink the concoction twice a day for two days. |
| Vegetable juice — A mixture of beets, cucumber and carrot juice may be helpful for patients with appendicitis. |
Fasting as Treatment for Uncomplicated Subacute Appendicitis
A case study24 presented by the TrueNorth Health Center also demonstrates how fasting may address appendicitis without further drug intervention. In this case, a 46-year-old man with uncomplicated appendicitis — confirmed through a sonogram — refused surgical and drug treatment, which led the doctors to prescribe medically supervised water-only fasting for seven days. According to the case report:
“The patient was monitored daily by on-site physicians in a residential facility. Twice-daily interviews and examinations were performed throughout the fast. Vital signs were taken once in the morning for the duration of the patient’s stay as well as a urinalysis performed every five days.
The seven-day fast was followed by a four-day gradual introduction of food consisting of juice, fruits and raw and steamed vegetables.
After the careful refeeding period, the abdominal pain was much improved … Follow-up laboratory tests revealed a normal white blood cell count … At three-month follow-up, the patient reported compliance to recommendations and no further abdominal pain.
The patient reported that he had been able to resume his normal exercise regimen of running four hours per week … At one-year follow-up, the patient reported no return of the abdominal pain over the year. He had resumed full exercise and had even completed a triathlon …
At two-year follow-up, the patient reported compliance to the lifestyle recommendations, continued to be free of right lower quadrant pain, and still had no recurrence of symptoms since the original presentation.”
- 1 Medical News Today, “Appendicitis: Why It Happens and How It Is Treated” August 2, 2016
- 2 Surgical Endoscopy 2017 Sep;31(9):3596-3604
- 3 Everyday Health, “What Is the Appendix?” July 22, 2014
- 4 Nature Immunology, November 30, 2015; 17, 179-186
- 5 Science Daily, Immune Cells Make Appendix ‘Silent Hero’ of Digestive Health, November 30, 2015
- 6 Zentralbl Chir. 2017 Dec;142(6):607-613
- 7 JAMA 2018;320(12):1259-1265
- 8 Popular Science September 27, 2018
- 9 Good News Network September 30, 2018
- 10 ARS Technica September 26, 2018
- 11 Annals of Surgery August 2017; 266(2): 237-241
- 12 Live Science September 27, 2018
- 13 JAMA 2018;320(12):1245-1246
- 14 New York Times September 25, 2018
- 15 Journal of the American College of Surgeons, August 2014; 219(2): 272–279
- 16 The New York Times, Treating Appendicitis Without Surgery, April 25, 2014
- 17 Mayo Clinic, Appendicitis Causes, August 20, 2014
- 18 Mayo Clinic, Appendicitis Definition, August 20, 2014
- 19, 20 NHS Choices, Treating Appendicitis, January 3, 2016
- 21 Mayo Clinic, Appendicitis Treatment and Drugs, August 20, 2014
- 22 Knoji, 15 Home Remedies to Cure Appendicitis — Relieve Pain and Inflammation of the Appendix Naturally
- 23 Top 10 Home Remedies, Home Remedies for Appendicitis
- 24 The Journal of Alternative and Complementary Medicine 2011; 17(3): 1-3 (PDF)
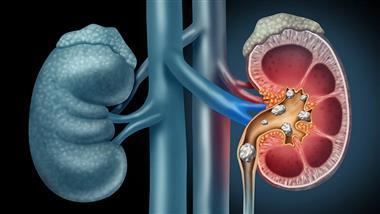
Antibiotics Linked to Increased Risk of Kidney Stones
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/07/24/oral-antibiotics-and-kidney-stones.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked July 24, 2023
STORY AT-A-GLANCE
- Five classes of oral antibiotics have been identified as risk factors for kidney stones: broad-spectrum penicillins, fluoroquinolones, nitrofurantoin, cephalosporins and sulfas
- The association is most pronounced among younger children, and remains statistically significant for up to five years after exposure, except for broad-spectrum penicillin
- Between 1997 and 2012, the annual incidence of kidney stone disease rose by 16%. The highest increase was seen in 15- to 19-year-olds, among whom the incidence rate increased 26% per 5 years
- Previous studies have found an association between oral antibiotics and inflammatory bowel disease (IBD) and colorectal cancer, likely due to disruption of gut microbiome
- Fluoroquinolones, which are frequently prescribed for upper respiratory infections and urinary tract infections (UTIs) have been linked to an increased risk for aortic dissection (tears in the aorta), which can be fatal
According to research1 published in the Journal of the American Society of Nephrology (JASN) in 2018, oral antibiotics are a risk factor for kidney stones. Health records for 13 million children and adults in the U.K. were reviewed, showing that exposure to five classes of oral antibiotics were associated with kidney stones within three to 12 months post-use. The adjusted odds ratio of kidney stones was:
- 1.27 for broad-spectrum penicillin
- 1.67 for fluoroquinolones
- 1.70 for nitrofurantoin/methenamine
- 1.88 for cephalosporins
- 2.33 for sulfas
The association was most pronounced among younger children and remained statistically significant for up to five years after exposure, with the exception of broad-spectrum penicillin. The authors concluded that:2
“Oral antibiotics associated with increased odds of nephrolithiasis [kidney stones], with the greatest odds for recent exposure and exposure at younger age. These results have implications for disease pathogenesis and the rising incidence of nephrolithiasis, particularly among children.”
Kidney Stones in Children Are on the Rise
If this link is true, then we’d expect to see rising rates of kidney stones in young patients, and that’s precisely what we’re seeing. As reported by NBC News, July 8, 2023,3 data show kidney stones are “now occurring in younger people, particularly among teenage girls,” and “diets high in ultraprocessed foods” and “increased use of antibiotics early in life” are thought to be among the key contributors to this trend.
Between 1997 and 2012, kidney stones during childhood doubled.
According to research4 published in the Clinical Journal of the American Society of Nephrology in 2016, between 1997 and 2012, the mean annual incidence of kidney stone disease across age groups increased 1% annually, from 206 to 239 per 100,000 persons.
The highest increase was seen in 15- to 19-year-olds, among whom the incidence rate increased 26% per 5 years. Within this age group, incidence was 52% higher among girls. In men, kidney stones became more common after age 25. According to the authors:5
“These changes in incidence resulted in doubling of the risk of nephrolithiasis during childhood and a 45% increase in the lifetime risk of nephrolithiasis for women over the study period.”
Oral Antibiotics Associated With Inflammatory Bowel Disease
As noted by the JASN authors,6 previous studies have found an association between oral antibiotics and inflammatory bowel disease (IBD), which is thought to be due to a disruption of gut microbiome.
In May 2022, research7 linking oral antibiotics and IBD was presented at the Digestive Disease Week conference in San Diego, California. Here, the researchers analyzed the health records of more than 2.3 million older adults, aged 60 to 90, who were part of the Danish National Patient Register and the Danish National Prescription Register.
On average, use of antibiotics was associated with a 64% increased risk of developing IBD, and the risk increased with additional doses.8 Compared with those who had taken no antibiotics in the previous five years:9
- One prescription for antibiotics was associated with a 27% increased risk of IBD
- Two prescriptions increased risk by 55%
- Three prescriptions increased risk by 67%
- Four prescriptions increased risk by 96%
- Five or more prescriptions increased risk by 236%
Adults who had been prescribed antibiotics one to two years prior to IBD diagnosis had the highest risk. And, while all classes of antibiotics were associated with increased IBD risk, fluoroquinolones, which include brand names Cipro and Levaquin, had the strongest association.10
Interestingly, a very recent study that was just published found that niacinamide may be very useful in the treatment and prevention of IBD11 by converting to NAD+ as a cofactor to produce more ATP in the mitochondria. I have written two reviews that discussed the many other benefits of niacinamide to increase NAD+.

Download this Article Before it Disappears
Fluoroquinolones Linked to Fatal Heart Condition
Fluoroquinolones, which are frequently prescribed for upper respiratory infections and urinary tract infections (UTIs) have also been shown to harm your heart. In December 2018, the U.S. Food and Drug Administration issued a safety announcement12 about fluoroquinolones after four studies linked the antibiotic to an increased risk of tears in the aorta (aortic dissection), which can be fatal.13
The aorta is the main artery in your body supplying oxygenated blood to your circulatory system. The artery comes from the left side of your heart and runs down the front of your backbone. The review by the FDA found fluoroquinolone antibiotics increase the risk of rupture following an aortic aneurysm (i.e., enlargement of the aorta to more than 1.5 times its normal size).
The finding led the FDA to caution against the use of fluoroquinolone antibiotics in those at risk unless there are no other treatment options available. Specifically, the antibiotic should not be used by:
- Those who are at risk for aortic aneurysm
- Those suffering peripheral atherosclerotic vascular disease or high blood pressure
- The elderly
- Those with Ehlers-Danlos syndrome or Marfan syndrome (genetic disorders)
Antibiotics Linked to Colorectal Cancer
Researchers have also linked the use of antibiotics to an increased risk of colorectal cancer. As reported by Live Science in 2014:14
“… researchers looked at the medical records of more than 22,000 colorectal cancer patients in the United Kingdom, and followed them for an average of six years … The researchers compared the amount of antibiotics the patients had taken at least six months before being diagnosed with cancer, to the amount of antibiotics taken by a group of about 86,000 healthy people.
After controlling for known risk factors for colorectal cancer — including obesity, diabetes, smoking and alcohol consumption — the results showed people who had taken antibiotics, including penicillins, quinolones and metronidazole, were 8% to 11% more likely to develop colorectal cancer … possibly through the effects of the drug on colon bacteria …”
A 2016 study15 also concluded that use of antibiotics was associated with an increased risk of colorectal cancer, especially when used frequently, and research16 published in 2017 found that women who had used antibiotics for two months or more were at an increased risk of developing colon polyps, which can be a precursor to colorectal cancer.
Those who used the drugs for a total of at least two months in their 20s and 30s had a 36% increased risk of polyps compared to those who did not, and women who used them for at least two months in their 40s and 50s had a 69% increased risk.
Antibiotics Fuel Chronic Disease by Decimating Your Microbiome
In the article I wrote in February of this year “The New Endangered Species: The Human Gut Microbiome,” I reviewed the documentary film “The Invisible Extinction,” which highlights the work of microbiologists Dr. Martin Blaser and Gloria Dominguez-Bello, who are investigating the links between chronic diseases and the loss of bacterial diversity in the human gut.
Overuse of antibiotics is a major driver of this loss. Elective C-sections and processed foods also contribute to the destruction of our microbiome. According to research published in the Cleveland Clinic Journal of Medicine in 2018,17 Americans have already lost half of their microbial diversity, which is why the risks of antibiotics must be carefully weighed against the benefits prior to use.
Many ‘Health Foods’ Also Contribute to Kidney Stones
As mentioned, diet can also play a significant role in kidney stone development, and processed foods aren’t the only culprits. Oxalate (oxalic acid with calcium attached) account for about 80% of all kidney stones, and high-oxalate foods such as spinach, Swiss chard and beet greens are touted as “superfoods.”
Another high-oxalate food is almonds, which you can easily “overdose” on if you’re eating bread made with almond flour or drinking almond milk, or if you’re on a keto or paleo diet, as they both tend to rely heavily on almonds. Other foods high in oxalate include peanut butter, wheat bran, potatoes, rice bran and dark chocolate.
If you’re prone to kidney stones, these are all foods that need to be avoided as much as possible. High-oxalate foods can also contribute to many other troublesome health problems, as discussed in my December 2022 interviewed with Sally Norton, author of “Toxic Superfoods.”
For example, aside from calcium oxalate kidney stones, other symptoms you might experience if you’re exposed to excessive amounts of oxalate include:
| Itchy rashes | Interstitial cystitis (frequent urination and bladder pain) |
| Poor or slow wound healing | Frail skin that bleeds easily (as your connective tissues are being damaged) |
| Joint pain | Osteoporosis (as the oxalates are extracting minerals from your bones) |
| Calcium deposits | Digestive problems |
| Neurological problems ranging from bad mood and klutziness to tremors | Poor sleep |
| Rheumatologically muscle pains like fibromyalgia | Vision problems such as near-sightedness, cataracts and poor night vision |
| Dental plaque or tartar |
The Antidote to Oxalates
Now, there is an “antidote” to oxalates that can be helpful if you’re prone to kidney stones. That antidote is citrate. I take citrates every day: magnesium citrate, calcium citrate and potassium citrate, typically with meals. This way absorption of any oxalates in the meal will be impaired. Aside from citrate supplements, raw grass-fed milk, sardines and lemon juice are great options. As explained by Norton in our December 2022 interview (see link above):
“You definitely need calcium and magnesium with high oxalate meals … The citrates in the minerals are especially important for … getting over the chronic illness of having an oxalate overload in your body. So, if you’re past the age of 10 and grew up on standard foods, you’ve got some degree of deposits in your bone marrow, your joints and glands …
The biggest biohack is calcium [citrate] because calcium promotes the clearing [of oxalate]. Some people can’t even tolerate the calcium because their body is so eager to upchuck this mess from its tissues that calcium gives it too much permission.”
Protect and Support Your Microbiome
Seeing how destruction of your microbiome with antibiotics can contribute to kidney stones, this is another area to pay close attention to. Consider the following to protect your microbiome as much as possible:
|
Do |
| Eat plenty of fermented foods — Healthy choices include lassi, fermented grass-fed kefir, natto (fermented soy) and fermented vegetables. |
| Take a probiotic supplement — If you don’t eat fermented foods on a regular basis, a probiotic supplement can be useful. |
| Boost your soluble and insoluble fiber intake, focusing on vegetables and seeds, including sprouted seeds. |
| Get your hands dirty in the garden — Exposure to bacteria and viruses in soil can help strengthen your immune system and provide long-lasting immunity against disease. |
| Open your windows — Research shows opening a window and increasing natural airflow can improve the diversity and health of the microbes in your home, which in turn benefit you.18 |
| Wash your dishes by hand instead of in the dishwasher — Research has shown washing your dishes by hand leaves more bacteria on the dishes than dishwashers do. Eating off these less-than-sterile dishes may decrease your risk of allergies by stimulating your immune system.19 Additionally, many dishwasher detergents have dangerous chemicals so if you do use detergent be careful to select a nontoxic one. |
|
Avoid |
| Antibiotics, unless absolutely necessary. If you do use them, make sure to reseed your gut with fermented foods and/or a high-quality probiotic supplement. |
| Foods that are high in oxalates. |
| Conventionally-raised meats and other animal products, as CAFO animals are routinely fed low-dose antibiotics. |
| Chlorinated and/or fluoridated water — This includes during bathing or showering. |
| Processed foods — Excessive sugars, along with otherwise “dead” nutrients, feed pathogenic bacteria. Food emulsifiers such as polysorbate 80, lecithin, carrageenan, polyglycerols, and xanthan gum may have an adverse effect on your gut flora. |
| Agricultural chemicals — Glyphosate is a widely used herbicide that and could potentially kill many of your beneficial gut microbes if you eat foods contaminated with it. |
| Antibacterial soap, as it kills off both good and bad bacteria and contributes to the development of antibiotic resistance. |
- 1 JASN June 2018; 29(6): 1731-1740
- 2, 6 JASN June 2018; 29(6): 1731-1740, Conclusion
- 3 NBC News, July 8, 2023
- 4, 5 Clinical Journal of the American Society of Nephrology March 2016; 11(3): 488-496
- 7, 8, 10 University of Minnesota, Center for Infectious Disease Research and Policy May 13, 2022
- 9 EurekAlert! May 13, 2022
- 11 Nutrients. 2023 Jul; 15(13): 2992. NAD+ Precursors and Intestinal Inflammation: Therapeutic Insights Involving Gut Microbiota
- 12 FDA Safety Announcement December 20, 2018
- 13 NBC News December 20, 2018
- 14 Live Science June 3, 2014
- 15 Dig Dis Sci. 2016 Jan;61(1):255-264
- 16 Gut April 4, 2017; 67(4): 672-678
- 17 Cleveland Clinic Journal of Medicine 2018; 85(12): 928-930
- 18 ISME Journal 2012 Aug;6(8):1469-79
- 19 Pediatrics February 23, 2015; 135(3): e590-e597
From spice rack to superhero: How ginger puts infection-fighting white blood cells on “high alert”
Reproduced from original article:
https://www.naturalhealth365.com/from-spice-rack-to-superhero-how-ginger-puts-infection-fighting-white-blood-cells-on-high-alert.html
by: July 11, 2023
 (NaturalHealth365) Experts warn that antibiotic resistance, in which disease-causing bacteria become immune to the drugs meant to defeat them, is reaching dangerous levels worldwide. In fact, even the Centers for Disease Control reports that this emerging public health crisis caused over 5 million deaths around the globe in 2019 alone. As scientists scramble to identify natural products that can serve as alternatives to antibiotics, a common kitchen spice – ginger – is giving rise to new hope.
(NaturalHealth365) Experts warn that antibiotic resistance, in which disease-causing bacteria become immune to the drugs meant to defeat them, is reaching dangerous levels worldwide. In fact, even the Centers for Disease Control reports that this emerging public health crisis caused over 5 million deaths around the globe in 2019 alone. As scientists scramble to identify natural products that can serve as alternatives to antibiotics, a common kitchen spice – ginger – is giving rise to new hope.
Ginger root, prized in the Ayurvedic and traditional Chinese medicine healing systems, has long been believed to support immune system health. Now, a new scientific study shows that a compound found in ginger can boost the readiness of white blood cells to fight infection. Let’s look at the intriguing mechanisms that allow ginger to put the body’s defense system on high alert.
Compound in ginger gives the “all hands on deck” signal to infection-fighting immune cells
The study, conducted at the Technical University of Munich and published in Molecular Nutrition and Food Research, examined the effect of gingerol – a pungent compound found in ginger – on immune cells known as neutrophil granulocytes. Often referred to as the “first line of defense” against infection, neutrophils destroy disease-causing bacteria and other pathogens by engulfing them, a process known as phagocytosis. (For good measure, neutrophils release anti-microbial enzymes as well).
The researchers found that gingerol seemed to enhance the inclination of neutrophils to attack pathogens. In other words, gingerol helped to “prime” the neutrophils, moving them from a resting state to a “ready to go” state. When researchers exposed cells to a peptide that mimics bacterial infection, they found that cells stimulated by the gingerol reacted about 30 percent more strongly than untreated cells.
Even modest amount of gingerol triggers beneficial response
The scientists found that the gingerol worked through a specific receptor, TRPV1, located on the neutrophils. (TRPV1 is also the receptor for capsaicin, the active component of chili peppers). And the team found that even very low concentrations of gingerol were enough to modulate cell activity. This supports the assumption that even modest amounts of gingerol – such as the amount found in a liter of ginger tea – could help “tweak” the immune system for the better. In addition, the ginger compounds appeared to enter the blood rapidly (roughly 30 to 60 minutes after consuming a liter of ginger tea).
While more research is needed to further unlock the infection-fighting capabilities of ginger and its compounds, the study provides a fascinating peek into the process. Additionally, it supports what forward-thinking doctors and herbal healers have always maintained: ginger enhances the ability of the immune system to target and destroy invading bacteria.
Ginger combats the microbial culprits responsible for common illnesses
In addition to promoting immune system defense against pathogens, gingerol has antibacterial, antifungal, and antiviral properties of its own. In a 2017 review published in the International Journal of Molecular Science, the authors cited laboratory studies showing that gingerol significantly inhibited the growth of multiple pathogens – including salmonella (a common food-borne microbe that causes diarrhea, fever, and stomach pains), E. coli, P. gingivalis (implicated in gum disease) and P. aeruginosa.
Most impressive of all, gingerol has been shown to work against methicillin-resistant staphylococcus aureus – the bacteria commonly known as MRSA. While ginger is not a silver bullet against pathogens, it appears to be able to discourage their growth – and to do so without contributing to the scourge of antibiotic resistance.
Elevate recipes with ginger while supporting immune health
You can access the benefits of ginger – and its lemony, spicy flavor – in a variety of ways. Employ it fresh or powdered in poultry, beef, and seafood recipes, or add the sliced or minced root to salads, salsa, and marinades. You can also partake in a zingy ginger shot, nibble on pickled ginger, or ginger in a fresh juice. (Ginger partners particularly well with apple, carrot and lemon juices).
To make a spicy, energizing ginger tea, wash and thinly slice a two-inch piece of fresh ginger root, then add to hot water and boil for ten to 30 minutes. Strain, allow the mixture to cool, and then sip away. If desired, you can sweeten it with raw honey and add a splash of lemon juice. (By the way, scientists report that ginger stimulates an enzyme in saliva that breaks down sulfur compounds, resulting in fresher breath. Is there no end to the benefits of this versatile spice?)
Many holistic doctors advise ginger to reduce pain and inflammation. Multiple studies have supported its use in treating osteoarthritis and menstrual cramps, and a 2020 review published in Cytokine credited it with lowering inflammatory markers such as C-reactive protein. Ginger is also advised to regulate blood sugar, promote healthy digestion, ease nausea, and protect against cognitive decline and Alzheimer’s disease.
Supplementary ginger is available in the form of capsules, tablets, tinctures, and extracts. Holistic healthcare providers typically advise amounts of 500 mg two or three times a day but check with your own doctor before supplementing.
No doubt, this new study suggests that natural herbs offer a safe way to eliminate the threat of antibiotic resistance, especially when used with other healthy lifestyle choices. So, go ahead and add this hard-working herb to your diet and enjoy the health benefits today.
Sources for this article include:
Onlinelibrary.wiley.com
Sciencedaily.com
Sciencedaily.com
Clevelandclinic.org
NIH.gov
WHO.int
CDC.gov
NIH.gov
Health News in Review: A New C. difficile Treatment, New AMA Medical Education, and New Insights into Ribosome Oxidation and the Free Radical Theory of Aging
Reproduced from original OMNS article (OrthoMolecular News Service):
http://orthomolecular.org/
Subscribe to the free Orthomolecular Newsletter: http://orthomolecular.org/subscribe.html
Go to the OMNS Archive: http://orthomolecular.org/resources/omns/index.shtml
Orthomolecular Medicine News Service, May 22, 2023
by Michael Passwater
OMNS (May 22, 2023) On April 26, 2023, the FDA approved Vowst for the prevention of recurrence of Clostridioides (formerly known as Clostridium) difficile infection (CDI). [1] There are approximately 500,000 cases of CDI each year in the United States, leading to 10,000 – 15,000 deaths per year. It is the most common hospital acquired infection. [2] C. diff is considered an opportunistic infection since it tends to only cause disease in people with weakened immune systems such as HIV/AIDS patients and transplant patients taking immunosuppressive medications, or people who have had their normal intestinal bacteria (“gut microbiome”) killed by antibiotics. Clindamycin, Fluoroquinolones, and Cephalosporins are the classes of antibiotics most commonly associated with C. diff and other forms of antibiotic associated diarrhea (AAD). The lack of host immune challenge or competition from healthy bacteria allows the invading C diff. bacteria to proliferate and cause illness. Interestingly, standard treatment for CDI is to administer additional antibiotics. Given their weakened, microbiome depleted state, it may not be surprising that people who have had CDI are more likely to suffer from the illness again.
The FDA granted the Vowst drug application “Priority,” “Breakthrough Therapy,” and “Orphan” status. The only alternative treatment recognized by the FDA for recurrent CDI is Rebyota, which the FDA approved Nov 30, 2022. [3] Both Rebyota and Vowst are fecal microbiota products, meaning they come from screened human donors of fecal matter (stool). Reboyta is administered rectally in a single dose. Vowst is administered orally as 4 pills per day for 3 days. Clinical trials with Reboyta showed a 71% success rate compared to a 58% success rate for a placebo, and Vowst showed an 87% success rate compared to a 60% success rate with a placebo. From both treatments, there is an unquantified risk of infectious disease transmission and food allergies due to the possibility of food particles and other fecal materials from the donor persisting in the finished product. One industry expert predicted the cost of a course of treatment with Vowst might be nearly $20,000. [4]
The concept of fortifying or replacing healthy bacteria in the intestines is not novel. Anecdotal, observational, and prospective clinical trials have suggested effectiveness and safety of a variety of probiotics and fermented foods for the prevention and treatment of AAD, including CDI. [5-23] In 2017, a Cochrane analysis of 31 clinical trials concluded there was moderate evidence of effectiveness and safety for probiotics. The analysis noted that more adverse events were seen in patients receiving placebos than patients receiving probiotics. These reviewers acknowledged the need for further studies, but felt the existing evidence was adequate to recommend advising hospitalized patients of the benefits and risks of probiotics. [24] In 2018, the Journal of the American Medical Association (JAMA) published a review of probiotic use with similar conclusions of efficacy and safety as the Cochrane analysis. [25] Maintaining adequate intestinal flora, especially during and after antibiotic treatment, is important for health. Healthy intestinal bacteria crowd out disease causing bacteria, produce vitamins, fatty acids, and other nutrients essential for a healthy body, and modulate the immune system.
Medical Education
The American Medical Association Education Hub (AMA Ed Hub) now offers a “Nutrition and Health” program with 48.5 continuing medical education units. Promotional material for the program states:
“Traditional medical models have discounted the importance of nutrition in health and in the prevention and management of a variety of health conditions, including cardiovascular disease, cancer, diabetes, and obesity. Recent overwhelming evidence has led to increased attention to nutrition as a core element of health, health equity and health care.” (AMA Ed Hub)
Overwhelming evidence, indeed! Although the program is not perfect, and has a distinct anti-supplement bias, it is a step in a healthy direction for American medicine. https://edhub.ama-assn.org/course/303
Those further along in their understanding of nutrition may prefer these educational resources:
International Society of Orthomolecular Medicine online learning: https://isom.ca/online-learning
The Riordon Clinic video library: https://riordanclinic.org/video-gallery
Free Radicals
In 1956, Denham Harman, MD, PhD, published the free radical theory of aging. [26] He suggested that highly reactive oxygen and nitrogen biomolecules generated by cellular respiration and stress caused many of the diseases of aging through destructive actions on cells and tissues. The term “free radical”, now more commonly called reactive oxygen and nitrogen species (RONS), refers to the unpaired electron in an oxygen or nitrogen molecule – an energy state that is not sustainable. [27] The molecule will steal an electron from the first thing it encounters, whether that is a nucleic acid, a protein, or a lipid, and cause a molecular chain reaction through the cell. “Antioxidants” are able to absorb or buffer the free radical by donating an electron to prevent or stop the chain reaction.
Dr. Harman suggested a low calorie, nutrient dense diet and supplementation with one or more inhibitors of oxidation could extend human life by 5 years or more. [28] His theory was met with ridicule and largely dismissed. Oxidative stress and, correspondingly, antioxidants, were not considered important to human health in that era. Even as supportive evidence steadily grew over the decades, criticism persisted. However, RONS have been generally accepted as important factors in many human biological processes. While not a complete explanation of all causes of aging and disease, Dr. Harman’s theory has helped advance our understanding of biochemistry. The evidence associating strong antioxidant capacity with wellness and longevity, and the number of diseases associated with oxidative stress continues to grow [29-35]. Dr. Harman never received a Nobel Prize, but he was nominated 6 times for the award.
Adding additional support to Dr. Harman’s concepts and the involvement of RONS and their neutralization in fundamental mechanisms preventing cellular damage, scientists at UF Scripps recently published insights into the mechanisms used by intracellular ribosomes to absorb free radical damage in a controlled fashion and replace the damaged proteins to restore the function of the ribosome. [36] Ribosomes are the factories that build all proteins. Ribosomes constitute roughly half of the mass of each cell in the human body. The ability of small segments of these critical organelles to “take a hit” to protect the rest of the ribosome is similar to the function of a bumper on an automobile. It is easier to repeatedly replace two proteins (Rps26, Rpl10) than to risk loss of an entire ribosome. Of note, the “bumper proteins” absorbing the free radical hits are rich in the sulfur containing amino acid cysteine, and zinc ions are critical for the bumper protein replacement process. The UF Scripps press release notes that the work could have implications for “cancer, the aging process, and growth and development.” If the damage control mechanism is overwhelmed by an excess of free radicals or if the cell lacks adequate repair materials, widespread ribosomal damage results, and therefore absent or altered protein production ensues which may lead to disease.
Summary
It is good to have choices. As the cost of health care in the United States continues to rise, while outcome measures such as lifespan continue to decline, a critical review of all available options to restore health and remain well is warranted. Informed choice allows wise selection of foods, vitamin and mineral supplements, activities, or prescriptions to address health concerns.
It is also encouraging to see the AMA recognize the key role of nutrition in human health – including serious diseases such as cardiovascular disease and cancer, and to provide increased access to nutrition education for physicians. Hopefully the new AMA “Nutrition and Health” program and similar ones will increase interest in the value of nutrition among healthcare providers and patients. As Hippocrates advised, “Let food be thy medicine and medicine be thy food.”
Continued careful research into the wondrous intricacies of human genetics and biochemistry increases our understanding of the connections between nutrients that serve as substrates, enzymes, and cofactors and the optimization of wellness. These mechanistic insights further inform choice.
“The doctor of the future will give no medication but will interest his patients in the care of the human frame, diet, and in the cause and prevention of disease” -Thomas A. Edison
References
1. FDA (2023) FDA Approves First Orally Administered Fecal Microbiota Product for the Recurrence of Clostridioides difficile Infection. https://www.fda.gov/news-events/press-announcements/fda-approves-first-orally-administered-fecal-microbiota-product-prevention-recurrence-clostridioides
2. CDC (2010) Clostridioides difficile Infection. https://www.cdc.gov/HAI/organisms/cdiff/Cdiff_infect.html
3. FDA (2022) FDA Approves First Fecal Microbiota Product. Nov 30, 2022. https://www.fda.gov/news-events/press-announcements/fda-approves-first-fecal-microbiota-product
4. Reuters (2023) US FDA approves Seres Therapeutics’ pill for deadly C. difficile infections. April 26, 2023. https://www.reuters.com/business/healthcare-pharmaceuticals/us-fda-approves-seres-therapeutics-pill-deadly-c-difficile-infections-2023-04-26
5. Kalakuntla AS, Nalakonda G, Nalakonda K, et al. (2019) Probiotics and Clostridium Difficile: A Review of Dysbiosis and the Rehabilitation of Gut Microbiota. Cureus. 11:e5063. https://pubmed.ncbi.nlm.nih.gov/31516774
6. Strohl M and Dyer D (2019) Diet and C. Difficile. Oncology Nutrition. https://www.oncologynutrition.org/erfc/eating-well-when-unwell/surgery/diet-and-c-difficile
7. Valdovinos MA, Montijo E, Abreu AT, et al. (2017) The Mexican consensus on probiotics in gastroenterology. Rev Gastoenterol Mex. 82:156-178. https://pubmed.ncbi.nlm.nih.gov/28104319
8. Cameron D, Hock QS, Kadim M, et al (2017) Probiotics for gastrointestinal disorders: proposed recommendations for children of the Asia-Pacific region. World J Gastroenterol. 23:7952-7964. https://pubmed.ncbi.nlm.nih.gov/29259371
9. Shen NT, Maw A, Tmanova LL, et al.(2017) Timely use of probiotics in hospitalized adults prevents Clostridium difficile infection: a systematic review with meta-regression analysis. Gastroenterology. 152:1889-1900. https://pubmed.ncbi.nlm.nih.gov/28192108
10. Sebastián Domingo JJ (2017) Review of the role of probiotics in gastrointestinal diseases in adults. Gastroenterol Hepatol. 40:417-429. https://pubmed.ncbi.nlm.nih.gov/28185664
11. Lewis PO, Lundberg TS, Tharp JL, Runnels CW. (2017) Implementation of global strategies to prevent hospital-onset Clostridium difficile infection: targeting proton pump inhibitors and probiotics. Ann Pharmacother. 51:848-854. https://pubmed.ncbi.nlm.nih.gov/28821215
12. Issa I, Moucari R. (2014) Probiotics for antibiotic-associated diarrhea: do we have a verdict? World J Gastroenterol. 20:17788-17795. https://pubmed.ncbi.nlm.nih.gov/25548477
13. Szajewska H, Canani RB, Guarino A, et al. (2016) Probiotics for the prevention of antibiotic-associated diarrhea in children. J Pediatr Gastroenterol Nutr. 62:495-506. https://pubmed.ncbi.nlm.nih.gov/26756877
14. Pace F, Pace M, Quartarone G. (2015) Probiotics in digestive diseases: focus on Lactobacillus GG. Minerva Gastroenterol Dietol. 61:273-292. https://pubmed.ncbi.nlm.nih.gov/26657927
15. Barker AK, Duster M, Valentine S, et al. (2017) A randomized controlled trial of probiotics for Clostridium difficile infection in adults (PICO). J Antimicrob Chemother. 72:3177-3180. https://pubmed.ncbi.nlm.nih.gov/28961980
16. Goldenberg JZ, Lytvyn L, Steurich J, et al. (2015) Probiotics For The Prevention Of Pediatric Antibiotic-Associated Diarrhea. Cochrane Database Syst Rev. 2015 Dec 22;(12):CD004827. https://pubmed.ncbi.nlm.nih.gov/26695080
17. McFarland LV (2007) Meta-Analysis Of Probiotics For The Prevention Of Traveler’s Diarrhea. Travel Med Infect Dis. 5:97-105. https://pubmed.ncbi.nlm.nih.gov/17298915
18. Basu S, Paul DK, Ganguly S, et al. (2009) Efficacy Of High-Dose Lactobacillus Rhamnosus GG In Controlling Acute Watery Diarrhea In Indian Children. J Clin Gastroenterol. 43:208-213. https://pubmed.ncbi.nlm.nih.gov/18813028
19. Guarino A, Guandalini S, Vecchio AL (2015) Probiotics For Prevention And Treatment Of Diarrhea. J Clin Gastroenterol. 49:S37-S45. https://pubmed.ncbi.nlm.nih.gov/26447963
20. Mu Q, Tavella VJ, Luo XM. (2018) Role Of Lactobacillus Reuteri In Human Health And Diseases. Front Microbiol. 9:757. https://pubmed.ncbi.nlm.nih.gov/29725324
21. Falagas ME, Betsi GI, Tokas T, Athanasiou S. (2006) Probiotics For Prevention Of Recurrent Urinary Tract Infections In Women. Drugs 66:1253-1261. https://pubmed.ncbi.nlm.nih.gov/16827601
22. Muresan AIP, Pop LL, Dumitrascu DL (2019) Lactobacillus Reuteri Versus Triple Therapy For The Eradication Of Helicobacter Pylori In Functional Dyspepsia. Med Pharm Rep. 92:352-355. https://pubmed.ncbi.nlm.nih.gov/31750434
23. Remes-Troche JM, Coss-Adame E, Valdovinos-Día MA, et al. (2020) Lactobacillus Acidophilus LB: A Useful Pharmabiotic For The Treatment Of Digestive Disorders. Therap Adv Gastroenterol. 13:1756284820971201. https://pubmed.ncbi.nlm.nih.gov/33281937
24. Goldenberg JZ, Yap C, Lytvyn L, et al. (2017) Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 12:CD006095. https://pubmed.ncbi.nlm.nih.gov/29257353
25. Goldenberg JZ, Mertz D, Johnston BC. (2018) Probiotics to Prevent Clostridium difficile Infection in Patients Receiving Antibiotics. JAMA. 320:499-500. https://pubmed.ncbi.nlm.nih.gov/30027207
26. Harman D (1956) Aging: a theory based on free radical and radiation chemistry. J Gerontol. 11:298-300. https://doi.org/10.1093/geronj/11.3.298. https://pubmed.ncbi.nlm.nih.gov/13332224
27. Weidinger A, Kozlov AV (2015) Biological Activities of Reactive Oxygen and Nitrogen Species: Oxidative Stress versus Signal Transduction. Biomolecules 5:472-484. https://pubmed.ncbi.nlm.nih.gov/25884116
28. Harman D (1992) Free radical theory of aging: history. EXS. 62:1-10. https://pubmed.ncbi.nlm.nih.gov/1450577
29. Andersen HR, Jeune B, Nybo H, et al. (1998) Low Activity of Superoxide Dismutase and High Activity of Glutathione Reductase in Erythrocytes from Centenarians. Age Ageing 27:643-648. https://pubmed.ncbi.nlm.nih.gov/12675104
30. C.A. Lang, Mills BJ, Lang HL, et al. (2002) High Blood Glutathione Levels Accompany Excellent Physical and Mental Health in Women Ages 60 to 103 Years. J. Lab. Clin. Med. 140:380-381. https://pubmed.ncbi.nlm.nih.gov/12486409
31. Aykac K, Ozsurekci Y, Yayla BCC, et al. (2021) Oxidant and antioxidant balance in patients with COVID-19. Pediatr Pulmonol. 56:2803-2810. https://pubmed.ncbi.nlm.nih.gov/34265172
32. Nar R, Çalış AG. (2018) Assessment of dynamic thiol/disulfide homeostasis in patients with asthma. J Lab Med. 42:99-104. https://www.degruyter.com/document/doi/10.1515/labmed-2017-0144/html
33. Erenler AK, Yardan T. (2017) Clinical utility of thiol/disulfide homeostasis. Clin Lab. 63:867-870. https://pubmed.ncbi.nlm.nih.gov/28627824
34. Erel Ö, Neşelioğlu S, Tunçay ME, et al (2021) A sensitive indicator for the severity of COVID-19:thiol. Turk J Med Sci. 51:921-928. https://pubmed.ncbi.nlm.nih.gov/33306332
35. Taylor, E.W. (2009) The oxidative stress-induced niacin sink (OSINS) model for HIV pathogenesis. Toxicology 278: 124-130. https://pubmed.ncbi.nlm.nih.gov/19857540
36. Yang Y-M, Jung Y, Abegg D, et al. (2023) Chaperone-directed ribosome repair after oxidative Damage. Mol Cell 83:1-11. https://pubmed.ncbi.nlm.nih.gov/37086725
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org
Find a Doctor
To locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource.
Editorial Review Board:
Albert G. B. Amoa, MB.Ch.B, Ph.D. (Ghana)
Seth Ayettey, M.B., Ch.B., Ph.D. (Ghana)
Ilyès Baghli, M.D. (Algeria)
Barry Breger, M.D. (Canada)
Ian Brighthope, MBBS, FACNEM (Australia)
Gilbert Henri Crussol, D.M.D. (Spain)
Carolyn Dean, M.D., N.D. (USA)
Ian Dettman, Ph.D. (Australia)
Susan R. Downs, M.D., M.P.H. (USA)
Ron Ehrlich, B.D.S. (Australia)
Hugo Galindo, M.D. (Colombia)
Gary S. Goldman, Ph.D. (USA)
Michael J. Gonzalez, N.M.D., Ph.D. (Puerto Rico)
William B. Grant, Ph.D. (USA)
Claus Hancke, MD, FACAM (Denmark)
Patrick Holford, BSc (United Kingdom)
Ron Hunninghake, M.D. (USA)
Bo H. Jonsson, M.D., Ph.D. (Sweden)
Dwight Kalita, Ph.D. (USA)
Felix I. D. Konotey-Ahulu, M.D., FRCP (Ghana)
Peter H. Lauda, M.D. (Austria)
Alan Lien, Ph.D. (Taiwan)
Homer Lim, M.D. (Philippines)
Stuart Lindsey, Pharm.D. (USA)
Pedro Gonzalez Lombana, M.D., Ph.D. (Colombia)
Victor A. Marcial-Vega, M.D. (Puerto Rico)
Juan Manuel Martinez, M.D. (Colombia)
Mignonne Mary, M.D. (USA)
Joseph Mercola, D.O. (USA)
Jorge R. Miranda-Massari, Pharm.D. (Puerto Rico)
Karin Munsterhjelm-Ahumada, M.D. (Finland)
Sarah Myhill, MB, BS (United Kingdom)
Tahar Naili, M.D. (Algeria)
Zhiyong Peng, M.D. (China)
Isabella Akyinbah Quakyi, Ph.D. (Ghana)
Selvam Rengasamy, MBBS, FRCOG (Malaysia)
Jeffrey A. Ruterbusch, D.O. (USA)
Gert E. Schuitemaker, Ph.D. (Netherlands)
Thomas N. Seyfried, Ph.D. (USA)
Han Ping Shi, M.D., Ph.D. (China)
T.E. Gabriel Stewart, M.B.B.CH. (Ireland)
Jagan Nathan Vamanan, M.D. (India)
Andrew W. Saul, Ph.D. (USA), Editor-In-Chief
Associate Editor: Robert G. Smith, Ph.D. (USA)
Editor, Japanese Edition: Atsuo Yanagisawa, M.D., Ph.D. (Japan)
Editor, Chinese Edition: Richard Cheng, M.D., Ph.D. (USA)
Editor, Norwegian Edition: Dag Viljen Poleszynski, Ph.D. (Norway)
Editor, Arabic Edition: Moustafa Kamel, R.Ph, P.G.C.M (Egypt)
Editor, Korean Edition: Hyoungjoo Shin, M.D. (South Korea)
Editor, Spanish Edition: Sonia Rita Rial, PhD (Argentina)
Editor, German Edition: Bernhard Welker, M.D. (Germany)
Associate Editor, German Edition: Gerhard Dachtler, M.Eng. (Germany)
Assistant Editor: Michael Passwater (USA)
Contributing Editor: Thomas E. Levy, M.D., J.D. (USA)
Contributing Editor: Damien Downing, M.B.B.S., M.R.S.B. (United Kingdom)
Contributing Editor: W. Todd Penberthy, Ph.D. (USA)
Contributing Editor: Ken Walker, M.D. (Canada)
Technology Editor: Michael S. Stewart, B.Sc.C.S. (USA)
Associate Technology Editor: Robert C. Kennedy, M.S. (USA)
Legal Consultant: Jason M. Saul, JD (USA)
Comments and media contact: drsaul@doctoryourself.com OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication.
Click here to see a web copy of this news release: https://orthomolecular.activehosted.com/p_v.php?l=1&c=284&m=283&s=a8c8fe7bea3fdaa4efae896c7612b3de
This article may be reprinted free of charge provided 1) that there is clear attribution to the Orthomolecular Medicine News Service, and 2) that both the OMNS free subscription link http://orthomolecular.org/subscribe.html and also the OMNS archive link http://orthomolecular.org/resources/omns/index.shtml are included.
Riordan Clinic | Orthomolecular.org
3100 N Hillside Ave
Wichita, Kansas 67219
United States
Can Broccoli Help Your Gut?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/04/24/can-broccoli-help-your-gut.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked April 24, 2023
STORY AT-A-GLANCE
- Evidence reveals that compounds in broccoli help protect the integrity of your intestinal lining and therefore may help prevent leaky gut, which increases inflammation and may be the basis for many chronic diseases
- Broccoli is a cruciferous vegetable with dozens of nutrients that support optimal health, including fiber, the anticancer compounds sulforaphane and glucoraphanin, anti-inflammatory and free radical quenching phenolic compounds and immune-boosting DIM
- 3,3′-diindolylmethane (DIM) is converted from indole-3-carbinol, a compound found in cruciferous vegetables. Researchers believe it may be a potent weapon against antibiotic-resistant pathogens
- You can maximize the benefits of broccoli by lightly cooking it to augment the sulforaphane content. You can raise levels further by pairing it with a myrosinase-containing food such as mustard seed, arugula or radishes
- Broccoli sprouts pack a greater nutritional punch and contain from 10 to 100 times the concentration of glucoraphanin and may have up to 100 times more enzymes than raw fruits and vegetables
Food is a profoundly effective means of affecting your overall health and cruciferous vegetables have long been cherished for their health benefits. Among those are broccoli, cabbage, collards, Brussels sprouts and cauliflower. One of the most well-known compounds in cruciferous vegetables is sulforaphane, which is an organic sulfur that supports normal cell function and division.
A 2023 study1 published in Laboratory Investigation by Penn State University scientists2 finds that broccoli’s health benefits may also extend to protecting the integrity of the gut lining. This important discovery adds to research that demonstrates how to protect your gut health, since a considerable portion of your immune system resides in the gastrointestinal tract.3
As such, optimizing your gut microbiome and protecting your gut integrity is a worthwhile pursuit that has far-reaching effects on physical and mental health. Mounting evidence also suggests that by keeping harmful microbes in the gut in check, protecting health-promoting gut bacteria and protecting the lining of your intestines, you help to shore up your protection against chronic disease.
Animal Model Demonstrates Broccoli Protects Gut Integrity
In the February 2023 study,4 researchers presented evidence that supported the role of the aryl hydrocarbon receptor in building intestinal resilience. Using an animal model, they found that broccoli contains molecules that attach to the receptor and safeguard the intestinal lining. Researcher Gary Perdew said:5
“We all know that broccoli is good for us, but why? What happens in the body when we eat broccoli? Our research is helping to uncover the mechanisms for how broccoli and other foods benefit health in mice and likely humans, as well. It provides strong evidence that cruciferous vegetables, such as broccoli, cabbage, and Brussels sprouts should be part of a normal healthy diet.”
The researchers fed an experimental group of mice a diet that was equal to a human eating roughly 3.5 cups of broccoli each day. The control group received a typical lab diet without broccoli. Examination of the intestinal tissue showed the mice who were fed a lab diet without broccoli had minimal AHR activity.
This reduced food transit time in the small intestines and altered the barrier function. The researchers also analyzed cells within the intestines that help prevent food particles and bacteria from escaping into the body. As SciTechDaily describes,6 these cells include goblet cells that secrete a protective layer of mucus, Paneth cells that secrete lysosomes with digestive enzymes and enterocytes that absorb water and nutrients.
When these cells are healthy, they help regulate intestinal wall integrity. The team found the mice that were not fed broccoli had a decreased number of each of these cells. They also found the mice who were fed broccoli did not experience the same damage. Aryl hydrocarbon receptor ligands found in broccoli will bind to AHR and this initiates activity that improves the function of the cells that line the intestinal wall. Perdew commented:
“The gut health of the mice that were not fed broccoli was compromised in a variety of ways that are known to be associated with disease. Our research suggests that broccoli and likely other foods can be used as natural sources of AHR ligands, and that diets rich in these ligands contribute to the resilience of the small intestine.”
Intact Gut Integrity Lowers Risk of Leaky Gut Syndrome
Mammals have a complicated and specialized gastrointestinal system that relies on an intact mucosal barrier. Evidence continues to mount demonstrating that your gut integrity may be an underlying trigger for most chronic diseases. The intestinal lining forms a barrier and when that permeability is compromised it allows bacteria and toxins to enter the bloodstream.7 Colloquially, this is known as leaky gut.
When environmental factors and pathogens enter the bloodstream, it can trigger the development of autoimmune diseases and increase the level of inflammation in your body. Research evidence also shows other factors that can promote tight cell junctions and therefore lower the risk of leaky gut.
For example, probiotics can enhance the growth of beneficial bacteria, which in turn improves the production of tight junction proteins. On the other hand, pathogenic bacteria facilitate a leaky gut. Lectins also have been linked to autoimmune reactions and inflammation as well as contributing to leaky gut syndrome.
Dr. Steven Gundry, author of “The Plant Paradox: The Hidden Dangers in ‘Healthy’ Foods That Cause Disease and Weight Gain,” suggests that lectins bind to receptor sites in intestinal mucosal cells and interfere with the absorption of nutrients across your intestinal wall.
According to a paper in the Journal of Autoimmunity, “… intestinal permeability (leaky gut) and bacterial translocation are important contributors to chronic systemic inflammation and, without repair of the intestinal barrier, might represent a continuous inflammatory stimulus capable of triggering autoimmune processes.”8
When left unchecked, leaky gut also leads to chronic systemic inflammation.9 Research has found associations between chronic inflammation and diseases that represent some of the leading causes of mortality and disability, such as diabetes, cancer, heart disease, chronic kidney disease and nonalcoholic fatty liver disease.
The specific chronic inflammatory disease that emerges depends in part on your genetic makeup, in part on the types of exposures you’ve had, and in part on the composition of your gut microbiome. As explained by Dr. Alessio Fasano, a pediatric gastroenterologist, researcher and director of the Center for Celiac Research and Treatment:10
“Besides genetic predisposition and exposure to environmental triggers, the pathogenesis of a variety of CIDs [chronic inflammatory diseases] seems to involve mutually influenced changes in gut permeability/Ag trafficking, immune activation, and changes in composition/function of the gut microbiome.
Depending on the host genetic makeup, activated T cells may remain within the GI tract, causing CID of the gut … or migrate to several different organs to cause systemic CID.”

Download this Article Before it Disappears
Multiple Health Benefits From Cruciferous Vegetables
In addition to the immense benefits of improving gut wall integrity, cruciferous vegetables have other health benefits. Sulforaphane11 is one of several compounds that can spark genetic changes and activate genes that fight cancer, while switching off others that fuel tumors. One paper suggested that cruciferous vegetables were “perhaps a key to eliminating cancer as a life-threatening disease.”12
Cruciferous vegetables provide dozens of nutrients that support optimal health, including fiber, the anticancer compounds sulforaphane13,14 and glucoraphanin,15 anti-inflammatory and free radical quenching phenolic compounds16 and immune-boosting DIM.17
3,3′-diindolylmethane (DIM) is converted from indole-3-carbinol, a compound found in cruciferous vegetables. DIM has been found to inhibit the PI3K protein that interrupts the pathway which regulates the growth and survival of cancer cells.18
Compounds in cruciferous vegetables have also been shown to lower your risk of obesity, reduce glucose production and improve Type 2 diabetes,19 support healthy liver function20 and improve allergies and asthma symptoms by reducing oxidative stress in the airways.21
Optimizing your gut microbiome is another way to help protect your health and reduce your risk of chronic disease. One of the easiest ways is to regularly eat traditionally fermented and cultured foods. Another is to include cruciferous vegetables in your daily diet.
A 2023 study22 published in the Journal of Nutritional Biochemistry found a diet rich in cruciferous vegetables helped reduce inflammation, and the metabolites were found to improve both forms of inflammatory bowel disease — ulcerative colitis and Crohn’s disease.23
A high intake of cruciferous vegetables was associated with a reduction in serum levels of proinflammatory cytokines. The bioactive metabolites of glucosinolates, also found in cruciferous vegetables, were associated with anti-inflammatory and anticancer activities. As News Medical Life Sciences notes:24
“Broccoli diets enhance the concentration of Bacteroides in human gut microbiota. In addition, enhancement in Clostridium spp., Proteobacteria, and butyrate-producing bacteria was observed.”
Compound in Broccoli May Solve Antibiotic Resistance
Antimicrobial resistance has been on the rise for several decades. Infections that were once easily treated are becoming a serious threat once again. According to the World Health Organization,25 antimicrobial resistance is “one of the top 10 global public health threats facing humanity,” and the primary cause of this man-made epidemic is the widespread misuse of antibiotics in human medicine and food production.
Agriculture accounts for 80% of all antibiotic use in the U.S.,26,27 so it’s a major source of human antibiotic consumption as well. Pathogens have also developed resistance to more than one drug (pan-resistance), which makes treating them challenging. While pan-resistant superbugs are increasing, the development of new antibiotics to tackle them has come to a near halt.28
Researchers believe that DIM may be a potent weapon against antibiotic-resistant pathogens. In a 2022 study29 published in Pharmaceutics, researchers investigated the activity of DIM in a series of lab assays on gram-negative pathogens. They found DIM has antibiofilm activity. Biofilm is a slimy substance that contains a mixture of bacteria and protein, which makes it challenging for antibiotics to reach the bacteria.
The research showed that DIM treatment on biofilm formation of two bacterial pathogens inhibited Acinetobacter baumannii by 65% and Pseudomonas aeruginosa by 70%. Both pathogens are a major source of hospital-based infections worldwide and are known to be resistant to many antibiotics.30
When DIM was combined with the antibiotic tobramycin, biofilm growth of P. aeruginosa was diminished by 94%.31 Non-healing wounds are often infected with pan-resistant bacteria, and it’s the biofilm that presents prevents the tissue from healing. To test whether DIM could work topically, the researchers infected puncture wounds on pigs with p. aeruginosa.32
They then applied a cream containing either DIM alone, the antibiotic gentamicin alone, or DIM plus gentamicin. The wounds treated with DIM for 10 days healed significantly better than untreated wounds, thanks to a significant reduction in biofilm formation. The combination of DIM plus the antibiotic worked even better. Interestingly, gentamicin alone slowed wound healing and formed lesions that prevented wound closure.
Maximize the Health Benefits of Broccoli
To get the most out of your broccoli, lightly steam it for three to four minutes until it’s tough-tender. Do not steam longer than five minutes. This will allow you to get the most bioavailable sulforaphane out of it. If you opt for boiling, blanch the broccoli in boiling water for no more than 20 to 30 seconds, then immerse it in cold water to stop the cooking process.
If you want to augment the sulforaphane content even further, pair broccoli and other cruciferous veggies with a myrosinase-containing food,33 which is needed for the sulforaphane to form. Mustard seed,34 daikon radishes, wasabi, arugula or coleslaw are high in myrosinase; of these, mustard seed is the most potent.
If you’re not a fan of mature cruciferous vegetables, then consider broccoli sprouts instead. They pack a greater punch in terms of nutrition, so you don’t have to eat as much. According to researchers,35 broccoli sprouts contain 10 to 100 times the concentration of the compound glucoraphanin (the glucosinolate of sulforaphane) of mature broccoli.
Sprouts can also contain up to 100 times more enzymes than raw fruits and vegetables, allowing your body to extract more vitamins, minerals, amino acids and essential fats from the foods you eat. You can easily and inexpensively grow broccoli sprouts at home, indoors, and you don’t have to cook them. They are eaten raw, usually as an addition to salad or juice.
- 1, 4 Laboratory Investigation, 2023; doi: 10.1016/j.labinv.2022.100012
- 2, 5, 6 SciTechDaily, April 9, 2023
- 3 Johns Hopkins Medicine, The Gut: Where Bacteria and Immune System Meet
- 7 Frontiers in Immunology, 2017; 8
- 8 Journal of Autoimmunity, 2018;92
- 9 Nature Medicine, 2019; 25 Abstract
- 10 F1000Research, January 31, 2020
- 11 Cancer Letters, 2008; 269(2)
- 12 Current Pharmacology Reports, 2015;1(1)
- 13 Archives of Pharmacal Research, 2020;43(4)
- 14 Frontiers in Oncology, January 23, 2023
- 15 Medicines, 2015;2(3)
- 16 Phys.org, June 22, 2016
- 17 Journal of Biomedical Research, 2014;28(5)
- 18 Anticancer Agents in Medicinal Chemistry, 2013;13(7)
- 19 New Scientist, June 14, 2017
- 20 Texas A&M Today, February 7, 2020
- 21 Respiratory Research, 2015;16(1)
- 22 Journal of Nutritional Biochemistry, 2023; 113(109238)
- 23, 24 News Medical Life Science, November 29, 2022
- 25 World Health Organization, November 17, 2021
- 26 Food Safety News, February 24, 2011
- 27 American Journal of Public Health, 2015;105(12)
- 28 World Health Organization, November 17, 2021 Why is antimicrobial resistance a global concern?
- 29, 31 Pharmaceutics, 2022;14(5)
- 30 Expert Review of Anti-Infective Therapy, 2010; 8(1)
- 32 Pharmaceutics, 2022;14(5) Section 3.5
- 33 American Institute for Cancer Research November 7, 2013
- 34 Food Chemistry, 2013;138(2-3)
- 35 PNAS, 1997;94(19)
Eye Drops Linked to Antibiotic-Resistant Bacterial Infection
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/02/18/eye-drops-antibiotic-resistant-infection.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked February 18, 2023

STORY AT-A-GLANCE
- January 20, 2023, the CDC announced an investigation into a multistate cluster of infections from May 17, 2022, to January 19, 2023, caused by Carbapenem-resistant Pseudomonas aeruginosa associated with artificial tears
- The infection was identified in 50 patients across 11 states, causing one death and at least three people to go blind in one eye
- Antibiotic resistance has been rising since the discovery of penicillin and now contributes to 4.95 million deaths worldwide each year; without change, consumption of antibiotics is estimated to increase by 200% by 2030
- Dry eye can be temporary from environmental factors like dry air or exposure to smoke, or it can be chronic. Data show optimizing vitamin D and omega-3 levels and using curcumin can all help ameliorate the symptoms of dry eye
Aging may be inevitable, but many age-related problems do not need to be. For example, your vision is largely dependent on your lifestyle. Your eyes, like many other organ systems, require appropriate nutrients throughout the years to ensure you maintain good eyesight and lower the potential of dry eye.
In late January 2023, a brand of eye drops marketed for dry eyes was connected to drug-resistant bacterial infections.1 Eye lubricant drops are marketed to support your tears. Your eyes need tears to keep them wet, smooth and to help focus light so you can see clearly. Your body uses tears to protect the eye from infections and foreign body irritations, like dust and dirt.
There are three different layers of fluid in your tears. Each layer is produced differently and performs a different function. The outer layer is an oily surface that keeps the watery layer from drying too quickly. It also makes the surface of the eyes smooth. The middle layer is watery and helps nourish the eye tissue and keep the eyes moist. The innermost layer of fluid is mucus.
This helps the watery layer stick to the surface of the eye and remain in place. Together these three layers are called the tear film. Inside the tear film are factors that help suppress inflammation in the eye, promote wound healing and defend against infection.2
You also have three different types of tears. Basil tears are the type just described that always stay in your eyes to help lubricate them and protect your cornea. Reflex tears are produced when an irritant is in your eye, such as a foreign body. These tears are released in large amounts to help flush out the foreign body and fight bacteria.
Finally, you produce emotional tears in response to sadness, joy and fear. According to the American Academy of Ophthalmology,3 some scientists propose emotional tears contain hormones that are not found in other types of tears. They hypothesize the stress hormones released in emotional tears may help regulate the body.
EzriCare Artificial Tears Linked to Infection
January 20, 2023, the CDC4 announced they were investigating a multistate cluster of infections caused by Carbapenem-resistant Pseudomonas aeruginosa that appeared to be associated with EzriCare Artificial Tears. The CDC stated they had identified 56 isolates from 50 patients across 11 states from May 17, 2022, to January 19, 2023.
The common exposure among the patients was the use of EzriCare Artificial Tears, which is a preservative-free product sold in a multidose bottle. The bacteria were isolated from several areas of the body, including cultures of the cornea, sputum, urine, blood and rectal swabs. January 24, 2023, EzriCare5 announced they had not received consumer complaints or reports of adverse events.
At that point, they also claimed to have “not received communication from any regulatory agency providing any outcomes or details to EzriCare about the ongoing investigation.”6 February 1, 2023, the company announced they received notice of the investigation, had stopped distribution and began contacting customers to advise them to discontinue use.
According to EzriCare, the artificial tears product is manufactured by Global Pharma Healthcare Pvt Limited in India and imported by ARU Pharma Inc. EzriCare places its label on the bottles and markets them to their customers. The company’s understanding is that the same product is also marketed under other brand names.
According to the CDC, as of January 20, 2023, there has been one death when pseudomonas entered the bloodstream. According to Fox News,7 there were 11 reported cases of eye infections and at least three people who became blind in one eye from the infection.
According to the CDC,8 pseudomonas aeruginosa is one type of pseudomonas that causes hospital-acquired infections. It is commonly found in the soil and water. Pseudomonas aeruginosa has become multidrug resistant and in 2017 caused an estimated 32,600 hospital-acquired infections and an estimated 2,700 deaths.
Antibacterial Resistance on the Rise
Interestingly, the first clinical use of antibiotics was Pyocyanase,9 which was extracted from pseudomonas aeruginosa and used in hospitals in the 1890s. Not long after the introduction of penicillin, doctors began noticing antibiotic resistance in bacteria that had once quickly succumbed to treatment. And the problem continues to grow.
In 2013, the CDC10 published the first Antibiotic Resistant Threats Report to highlight the danger of antimicrobial resistance and underscore the threat to human health. The 2022 report found much of the progress had been lost, in large part to the overuse of antibiotics during the COVID-19 viral pandemic.
Antibiotic-resistant pathogens are conservatively estimated to cause at least 2.8 million infections annually in the U.S.11 and lead to 35,000 deaths each year. Globally, data from a study12 published in February 2022, show there are 4.95 million deaths associated with antibiotic-resistant infection and 1.27 million directly attributable to them.
Even as the challenge of antibiotic resistance was better understood, global consumption of the drugs rose by 65% between 2000 and 2015,13 driven by low- and middle-income countries where the drugs are often available without a prescription, which increases the risk for potential abuse. Antibiotics are routinely used to promote growth in livestock,14 and use accounts for about 80% of all antibiotics.15
The danger associated with giving livestock antibiotics is that it changes their gut microbiome, which is in part how they promote unnatural growth in the animal. However, some of those gut bacteria become antibiotic resistant. These can either be passed into the environment through the animal’s manure or may contaminate the meat during slaughter or processing.
The problems with antibiotic resistance need to be addressed through public policy. Yet, our individual choices influence personal risk. You can help lower your risk of contracting and or spreading a drug-resistant infection using some of the following strategies.
• Practice infection prevention, with a focus on naturally strengthening your immune system. Foundational strategies include avoiding sugars, processed foods and grains, stress reduction and optimizing your sleep and vitamin D level. Adding in traditionally fermented and cultured foods helps optimize your microbiome. Properly wash your hands with warm water and plain soap, to prevent the spread of bacteria.
• Limit your exposure to antibiotics — Keep in mind that antibiotics do not work for viral infections. Avoid antibiotics in food by purchasing organic or biodynamic grass fed meats and animal products and organically grown fruits and vegetables. Avoid antibacterial soaps, hand sanitizers and wipes, as these promote antibiotic resistance by allowing the strongest bacteria to survive and thrive in your home.
• Take commonsense precautions in the kitchen — Kitchens are notorious breeding grounds for disease-causing bacteria. To avoid cross-contamination between foods in your kitchen, adhere to the following recommendations:
◦ Use a designated cutting board, preferably wood, not plastic, for raw meat and poultry, and never use this board for other food preparation. Color coding your cutting boards is a simple way to distinguish between them.
◦ Sanitize your cutting board with hot water and detergent. For an inexpensive, safe and effective kitchen counter and cutting board sanitizer, use 3% hydrogen peroxide and vinegar. Keep each liquid in a separate spray bottle, and then spray the surface with one, followed by the other, and wipe off.
◦ Coconut oil can also be used to clean, treat and sanitize your wooden cutting boards. It’s loaded with lauric acid with potent antimicrobial actions. The fats will also help condition the wood.

Download this Article Before it Disappears
What Is ‘Dry Eye’?
Another step to lowering your risk of infection is to reduce your dependence on over-the-counter products, such as artificial tears. Artificial tears or eye lubricants are used to help ease the symptoms of dry eye syndrome. This happens when the eye is unable to produce enough tears to maintain a healthy eye environment. The incidence of dry eye increases with age and may be related to hormonal changes.16
Other environmental factors that trigger temporary symptoms of dry eye include wearing contact lenses, a dry indoor environment, smoking or secondhand smoke exposure, or cold and allergy medications. In some cases, chronic dry eye may be caused by a nutritional deficiency, or damage to the tear gland. The most common cause of tear gland damage is Sjögren’s Syndrome, which is a systemic autoimmune, rheumatic disease that affects the whole body.
Symptoms of dry eye include blurred vision, sensitivity to light, burning, itching or redness in the eye, or a scratchy feeling. Depending on the type or cause of the condition, an ophthalmologist may prescribe over-the-counter eye drops, prescription medications, tear duct plugs or surgery.
The American Optometric Association17 recommends several steps to prevent temporary dry eye. This includes blinking regularly when you’re staring at a computer screen for a long time, wearing sunglasses to reduce exposure to the sun and dry winds and increasing the humidity at work and home. Dehydration and a lack of sleep can also contribute to temporary symptoms of dry eye.
Tips to Treat Dry Eye Naturally
While it may seem easier to grab a bottle of artificial tears, the long-term solution is to make slight changes in your lifestyle habits and nutritional intake to help offset the condition. Your tears are made in part with water, so it makes sense to stay hydrated. Dehydration also leads to you feeling tired, grumpy and sick, and accelerates biological aging.
It’s not necessary to count how many glasses of water you drink each day. Two indicators you need fluid are your thirst and the color of your urine. Thirst helps ensure your needs are met on a day-to-day basis. The color of your urine can also be used as a guide. While your urine color can be influenced by medication or supplements, overall, if it’s a deep dark yellow, you are likely not drinking enough water.
Adequate hydration is indicated by pale, straw-colored or light-yellow urine. Most healthy individuals urinate on average seven to eight times each day. If you aren’t urinating at least every two to three hours while you’re awake, it may indicate that you’re not drinking enough.
Optimizing your vitamin D levels also protects against dry eye syndromes. A 2015 study18 called it “more than an incidental association” and concluded that dry eye and impaired tear function in patients with a vitamin D deficiency indicate it plays a protective role.
As I’ve discussed in the past optimizing vitamin D levels affects many bodily systems including reducing your risk of infectious disease,19 cardiovascular disease20 and autoimmune diseases21 to name just three.
Regular sensible sun exposure is the best way to optimize your vitamin D status, but many need an oral vitamin D3 supplement during the winter months. The only way to gauge whether you need a supplement and how much to take, is to test your vitamin D level, ideally twice a year. This is particularly important if you’re pregnant, planning to become pregnant, or if you have cancer.
The optimal level is between 60 nanograms per milliliter (ng/mL) and 80 ng/mL with 40 ng/mL being a low cutoff point for sufficiency to prevent a wide range of diseases. GrassrootsHealth22 makes testing easy by offering an inexpensive vitamin D3 testing kit and an online vitamin D3 calculator you can use to estimate the dosage once you know your current serum level.
Another nutritional supplement that is effective in preventing and supporting eye health is omega-3 fatty acids. This is a recommendation from the American Optometric Association23 and a survey24 of 206 optometrists in Australia and New Zealand. In that survey, 78% recommended omega-3-rich foods or supplements for dry eye disease and 79% said they recommended their patients consume omega-3 fats to improve their eye health.
Although fish oil is a well-known source, it has several drawbacks, including the lack of phospholipids. Omega-3 fats DHA and EPA are water insoluble and thus must be packaged into lipoprotein vehicles such as phospholipids. This is primarily why krill oil bioavailability is so much higher than fish oil since the DHA and EPA in fish oil are bound to triglycerides. Marine sources high in omega-3 and low in environmental pollutants include:
- Wild Alaskan salmon
- Small fatty, cold-water fish such as herring, sardines and anchovies
- Fish roe
- Krill oil
Finally, data also show that curcumin has a beneficial effect on several ocular diseases, including dry eye syndrome. In a 2014 paper,25 the researchers noted the beneficial effects on dry eye as did researchers in 201926 and 2020.27
It is a potent antioxidant28 and boosts the function of your own antioxidant enzymes.29 Overall, curcumin appears to be powerful, cost-effective and has a low toxicity profile. As such, it could be a valuable supplement. It is also worth noting the beneficial impact on pathways that help reverse insulin resistance, metabolic syndrome and obesity.30,31
I believe curcumin is a valuable nutritional addition worthy of consideration for all-around good health since inflammation drives so many different disease processes.
- 1 CNN Health, January 31, 2023
- 2 Experimental Eye Research, 2020; 197(108115)
- 3 American Academy of Ophthalmology, All About Emotional Tears, last subhead
- 4 Centers for Disease Control and Prevention, January 20, 2023
- 5, 6 EzriCare, January 24, 2023
- 7 Fox News, February 1, 2023
- 8 CDC, Pseudomonas aeruginosa in Healthcare Settings
- 9 Medical News Life Sciences, The History of Antibiotics
- 10 Centers for Disease Control and Prevention, 2019
- 11 CDC, In Our Scope: 2022 and Beyond
- 12 The Lancet, 2022; doi: 10.1016/S0140-6736(21)02724-0
- 13 PNAS, 2018;115(15)
- 14 USDA, November 24, 2015
- 15 Food Safety News, November 24, 2011
- 16 Mount Sinai, Dry Eye Syndrome
- 17, 23 American Optometric Association, Dry Eye
- 18 Journal of Rheumatic Diseases, 2015; 19(1)
- 19 SciDevNet, July 24, 2015
- 20 International Journal of Nanomedicine, 2018;13(455)
- 21 The BMJ, 2022;376
- 22 GrassrootsHealth, D*action Tests
- 24 Nutrients, 2020 Apr 22;12(4):1179
- 25 Planta Medica, 2014; 80(4)
- 26 Central European Journal of Immunology, 2019;44(2)
- 27 Nutrients, 2020;12(4)
- 28 Advances in Experimental and Medicinal Biology, 2007;595
- 29 BioMedicine 2019;9(4)
- 30 Frontiers in Pharmacology, 2019; doi: 10.3389/fphar.2019.00649
- 31 Toxicology and Applied Pharmacology, 2016;304
Got MilQ? Fake Milk to Replace Dairy and Breast Milk
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2022/12/22/biomilq-fake-milk.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked December 22, 2022
STORY AT-A-GLANCE
- The globalist technocrats are intent on monopolizing the entire food supply. They already have a monopoly on grains and have made headway in genetically engineered (GE) seafood. The next targets include lab-grown meats and dairy substitutes
- Biomilq, made from cultured breast tissue, will be marketed as a breast milk substitute
- The company Helaina is working on creating glycoproteins “identical to those found in breast milk.” Those proteins can then be added to a variety of infant formulas, seniors’ nutrition and, eventually, all sorts of foods
- The justification for creating synthetic milk substitutes is, of course, preventing and reversing “climate change.” That’s the justification used to sell virtually all fake foods. In reality, however, they will perpetuate and worsen adverse effects on the environment
- Lab-created foods are ultraprocessed and therefore qualify as junk food. Fake meat and dairy cannot replace the complex mix of nutrients found in grass fed beef and dairy, and it’s likely that consuming ultraprocessed meat and milk alternatives may lead to many of the same health issues that are caused by a processed food diet
- The starting ingredients in fermented synthetic biology products are cheap sugars derived from GE corn and soy. All GE crops are grown in environmentally destructive monocultures, and use loads of herbicides such as glyphosate, pesticides like neonicotinoids and synthetic fertilizers. As a result, they’re loaded with chemical residues that end up in the final product
The globalist technocrats are intent on monopolizing the entire food supply. They already have a monopoly on genetically engineered (GE) grains and have made headway in GE seafood. The next targets are lab-grown meats and dairy substitutes. There’s even a lab-made breast milk alternative on the way called Biomilq, which is made from cultured breast tissue.1
Another company, Helaina, aims to create glycoproteins “identical to those found in breast milk,”2 which can then be added to a variety of infant formulas. They may also be used in seniors’ nutrition and eventually, all sorts of foods.
Many familiar globalists are invested in these faux dairy ventures. Biomilq investors, for example, include Bill Gates, Jeff Bezos, Mark Zuckerberg, Richard Branson, Masayoshi Son, Jack Ma, Michael Bloomberg and Marc Benioff.3
The first Biomilq product is expected to be ready for the market within the next three to five years.4 Other animal-free milk products are expected to hit the shelves sometime between 2023 and 2024.5,6 That includes ice cream made with lab-grown diary, which will go into Ben & Jerry’s product line.7
In the Environmental Health Symposium video above, Alan Lewis reviews what goes into the making of synthetic biology. Synthetic biology goes by many names, including “gene edited fermentation” and “precision fermentation products.”
While that sounds fairly innocuous, synthetic biology manufacturers rarely ever discuss what goes into the feed they use to grow the target organism, or what happens to the waste at the end of the fermentation process. That’s understandable, as both raise a number of serious questions.
What Are the Base Ingredients?
As explained by Lewis, the starting ingredients in fermented synthetic biology products are cheap sugars derived from GE corn and soy. All GE crops are grown in environmentally destructive monocultures with taxpayer subsidies, and use loads of herbicides such as glyphosate, pesticides like neonicotinoids and synthetic fertilizers. As a result, they’re loaded with chemical residues that end up in the final product.
In addition to a base of sugars, hundreds of other ingredients may be added to the ferment in order to produce the desired end product, such as a certain protein, color, flavor or scent.
Aside from the desired target metabolite, these gene-edited organisms may also be spitting out any number of non-target metabolites that have completely unknown environmental consequences and health effects.
As explained by Lewis, the most-often used microorganism in the fermentation process is E.coli. The E.coli is gene-edited to produce the desired compound through its digestive process. It also needs to be antibiotic-resistant, since it needs to survive the antibiotics used to kill off other undesirable organisms in the vat.
Aside from the desired target metabolite, these gene-edited organisms may also be spitting out any number of non-target metabolites that have completely unknown environmental consequences and health effects.
How Are Synthetic Biology Ferments Created?
As explained by Lewis, the various “feed” ingredients are placed in a fermentation bioreactor set at 87 to 90 degrees Fahrenheit for anywhere from 24 to hundreds of hours to grow the target microorganism. The target organisms in the ferment consume the nutrients they need, and what’s left over after those organisms are extracted is hazardous biowaste.
Importantly, while traditional fermentation processes, such as the making of beer, produces waste products that are edible by animals, compostable and pose no biohazard, the same cannot be said for these GMO synthetic biology ferments. The biowaste must first be deactivated, and then it must be securely disposed of. It cannot go into a landfill.
It’s important to realize that they are creating GMO organisms that have never existed on earth before, and these organisms and their waste are neither edible nor compostable, and there are unknown risks involved with unintentional or intentional release of these organisms into the environment.
They may also result in novel foodborne illnesses. And, since antibiotics are used to prevent the growth of undesirable organisms in the ferment, antibiotic-resistant organisms are automatically integrated into the final product. The types of foodborne illness that might be caused by gene-edited E.coli and its metabolites are anyone’s guess at this point. Nobody knows what such illness might look like.
The Fake Justification for Fake Foods
The justification for creating synthetic biology for food, including milk substitutes, is to prevent and reverse “climate change.” As reported by CNBC in June 2020:8
“Biomilq co-founder and CEO Michelle Egger … and her co-founder, CSO Leila Strickland, hope that the breast milk produced by Biomilq from culturing mammary epithelial cells will help reduce the carbon footprint from the global infant formula market …
‘Right now, by the estimations we have been able to make, at least 10% of the dairy market globally ends up in infant formula,’ Eggers said. ‘That means per-infant-fed formula in the U.S., 5,700 metric tons of CO2 are produced, and 4,300 gallons of freshwater are consumed each year to feed a child. Parents want to do what’s best for their kids but shouldn’t have to decide between feeding their children and protecting the planet.'”
While the push for synthetic biology is built on the idea that it will somehow save the environment from the ravages of factory farming, concentrated animal feeding operations (CAFOs) and monocultures, it’s incredibly misleading, because it doesn’t address the fact that there are environmentally beneficial ways to farm, and we really should switch to those instead of transitioning into factory laboratories where everything that comes out of it is a biohazard.
Fake Food Manufacturing Creates Toxic Waste Products
In February 2021, the Good Food Institute (GFI), a nonprofit group behind the alternative protein industry, released a techno-economic analysis of cultivated meat, which was prepared by consulting firm CE Delft.9 In it, they developed a model to reduce the current costs of cultured meat production down to a point that would make it economically feasible in full-scale plants by 2030, a model they said is “feasible.”
In attempting to create cultured meat on the scale that would be necessary to feed the world, logistical problems are numerous and, possibly, insurmountable. There are waste products — catabolites — to deal with, as even cultured cells excrete waste that is toxic.
Oxygen and nutrients must also be adequately distributed to all the cells, something that’s difficult in a large reactor. Stirring the cells faster or adding more oxygen may help, but this can cause fatal stress to the cells.10
The environmental “benefits” are also on shaky ground when you factor in soy production as well as the use of conventional energy sources. When this is factored in, GFI’s life-cycle analysis found that cultured meat may actually be worse for the environment than conventionally produced chicken and pork.11,12
Repeat of a Failed System
Yet, the push for the creation of synthetic biology continues. In the foreword to Navdanya International’s report “False Solutions That Endanger Our Health and Damage the Planet,” Vandana Shiva details how lab-grown foods are catastrophic for human health and the environment, as they are repeating the mistakes already made with industrial agriculture:13
“In response to the crises in our food system, we are witnessing the rise of technological solutions that aim to replace animal products and other food staples with lab-grown alternatives. Artificial food advocates are reiterating the old and failed rhetoric that industrial agriculture is essential to feed the world.
Real, nutrient-rich food is gradually disappearing, while the dominant industrial agricultural model is causing an increase in chronic diseases and exacerbating climate change.
The notion that high-tech, ‘farm free’ lab food is a viable solution to the food crisis is simply a continuation of the same mechanistic mindset which has brought us to where we are today — the idea that we are separate from and outside of nature.
Industrial food systems have reduced food to a commodity, to ‘stuff’ that can then be constituted in the lab. In the process, both the planet’s health and our health have been nearly destroyed.”
Lab-Made Foods Are Junk Foods
It’s important to realize that all lab-created “foods” are ultraprocessed, and will likely impart the same kind of ill health effects as other ultraprocessed foods. In 2018, Friends of the Earth (FOE), a grassroots environmental group, released a report that posed critical questions about the trend toward synthetic biology. In it, they stressed the highly-processed nature of these products:14
“Various ‘processing aids’ are employed to make some of these products, including organisms (like genetically engineered bacteria, yeast and algae) that produce proteins, and chemicals to extract proteins.
For example, chemicals like hexane are used to extract components of a food, like proteins (from peas, soy, corn etc.) or compounds (from genetically engineered bacteria) to make xanthan gum … disclosure of these ingredients is not required.
Other processing aids (e.g. bacteria, yeast, algae), including those that are genetically engineered to produce proteins, are also not currently required to be disclosed on package labeling. The lack of transparency makes it difficult to assess the inputs and impact of their use.”
Basically, what the globalist cabal is attempting to do is to eliminate conventional farming methods like raising cattle for beef and dairy products, and replace them with synthetic, patented reproductions. In short, they’re taking whole foods and turning them into ultraprocessed junk foods, all while trying to convince you the junk food is healthier for you.
Synthetic Biology Is Part of a Control Scheme
Aside from the potential health hazards, lab-grown foods rely on monocultured crops that destroy the soil, resulting in carbon release. So, right there, the climate change justification falls apart. Since synthetic biology relies on GMO monoculture, it creates the very things they claim to counteract: environmental degradation that results in climate change.
As noted by Lewis, synthetic biology, which is the latest addition to the patented, genetically modified organism (GMO) food system, also results in a “massive shift in ownership and concentration of wealth … and control over our food supply.”
In short, synthetic biology creates reliance on industry that can then be used to manipulate and control the population in any number of ways. In the long term, people will eventually lose the know-how of producing their own food using traditional methods, and this may well be part of the plan.
The globalist cabal intends to create a one world government, and what better control tool than having everyone completely dependent on the state for all of its food?
Protect Your Health by Avoiding Frankenfoods
The drive for plant-based alternatives to real animal food, be it meat or dairy, isn’t due to health, or even to support vegan or vegetarian diets. Those truly interested in eating a plant-based diet can do so by eating real plants, after all, and in so doing can enjoy the many health benefits that eating plant foods provides. No, it’s about creating a system of control through food. It’s also a way to control people’s health.
It’s already known that the consumption of ultraprocessed food contributes to disease,15 but manufactured fake meat and dairy may also pose additional unknown risks.16 The benefactor of ill health, of course, is Big Pharma.
The processed food industry has spent many decades driving chronic illness that is then treated with drugs rather than a better diet. Synthetic foods will likely be an even bigger driver or chronic ill health and early death.
The fact is, fake meat and dairy cannot replace the complex mix of nutrients found in grass fed beef and dairy, and it’s likely that consuming ultraprocessed meat and milk alternatives may lead to many of the same health issues that are caused by a processed food diet. So, if you want to really protect your health and the environment, skip pseudofoods that require patents and stick to those found in nature instead.
- 1, 4 Alarabiya.net May 3, 2022
- 2 Food Navigator December 12, 2022
- 3, 8 CNBC June 16, 2020
- 5 Startup Daily July 27, 2021
- 6 Sydney Spring Herald September 13, 2022
- 7 ZME Science December 9, 2022
- 9 Techno-Economic Analysis for the production of cultivated meat February 2021
- 10, 12 The Counter September 22, 2021
- 11 LCA of cultivated meat – February 2021, Page 3
- 13 Children’s Health Defense April 5, 2022
- 14 Friends of the Earth, From Lab to Fork, June 2018 (PDF)
- 15 BMJ 2018; 360:k322
- 16 Consumer Reports, August 29, 2019, Impossible Burger, What is it?
Antibiotics Linked to Fatal Heart Condition
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2022/10/22/antibiotics-trigger-heart-disease.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked October 22, 2022

STORY AT-A-GLANCE
- Fluoroquinolones, long associated with Achilles tendonitis and rupture, have been demonstrated to increase your risk of aortic dissection (a tear in the wall of the major artery, allowing blood to flow between the layers) or aortic rupture, which can lead to death
- Even though “black-box” warnings are now attached to them, fluoroquinolones are still often prescribed for upper respiratory infections or urinary tract infections
- Antibiotic use can trigger a permanent change in your gut microbiome, which accounts for nearly 80% of your immune system function, so it is important to use antibiotics only when absolutely necessary
- You may reduce your risk of bacterial and viral infections by supporting your immune system through simple lifestyle measures, such as quality sleep, fermented foods, regular exercise and optimizing your vitamin D level
Research shows your body’s microbiome has nearly 39 trillion bacteria.1 During early years, your family, dietary intake and environmental exposure contribute to the variety in your microbiome, influencing your lifelong health. Everyday activities such as brushing your teeth, eating, kissing someone or handling a family pet also affect your microbiome.
This composition may be as distinct to you as a fingerprint and plays an enormous role in disease prevention, and influences the function of your skin, lungs, breast and liver.2 Harmful bacteria can trigger illness and disease, which is frequently treated with antibiotics. Of the 10 most commonly prescribed, two are from the antibiotic class of fluoroquinolones.3
The Food and Drug Administration (FDA) first added a boxed warning to fluoroquinolones in 2008, due to the increased risk for tendinitis and tendon rupture.4 Boxed warnings, also referred to as black box warnings, appear on prescription drug labels designed to call attention to serious or life-threatening risks.5
An additional warning was added in 2011 for those suffering from myasthenia gravis, and updates were included in 2013 describing irreversible peripheral neuropathy.6 In 2018, the FDA warned fluoroquinolone antibiotics may increase the occurrence of ruptures or tears in the aorta.7 And, in January 2022, the FDA decided:8
“We have determined that fluoroquinolones should be reserved for use in patients with no other treatment options for acute bacterial sinusitis, or ABS, acute bacterial exacerbation of chronic bronchitis (ABECB), and uncomplicated UTI because the risks generally outweighs the benefits.
For some serious bacterial infections the benefits of fluoroquinolones outweigh the risks, and it is appropriate for them to remain available as a therapeutic option.”
Yet, despite these warnings, researchers found in April 2022 that fluoroquinolones are still among the most-prescribed antibiotics around the world.9 They concluded that some health care workers may have an “unsatisfactory knowledge” of the safety profiles and risks of these drugs, and that more education on adverse reactions to fluoroquinolones may be needed.
FDA Warning Links Fluoroquinolones With Aortic Damage
The aorta is the main artery in your body supplying oxygenated blood to your circulatory system. The artery comes from the left side of your heart and runs down the front of your backbone. The review by the FDA found fluoroquinolone antibiotics increase the risk of tears in the aorta, also called aortic dissections, or ruptures of an aortic aneurysm, leading to excessive bleeding and death.
The findings occurred when antibiotics were given by mouth or through an injection. This led the FDA to caution against the use of fluoroquinolone antibiotics in those at risk, unless there are no other treatment options available.
Specifically, the antibiotic should not be used in those who are at risk for, or have a current, aortic aneurysm, such as those suffering peripheral atherosclerotic vascular disease, hypertension and specific genetic conditions such as Ehlers-Danlos syndrome or Marfan syndrome.10
Findings were pulled from four published observational studies, which taken together demonstrated a consistent association between aortic dissection or rupture and fluoroquinolone use. The underlying mechanism could not be determined from those studies.
Some of the commonly used fluoroquinolones include ciprofloxacin (Cipro), levofloxacin (Levaquin), gemifloxacin (Factive) and moxifloxacin (Avelox). These are prescribed to treat upper respiratory and urinary tract infections. In a statement, the FDA warns:11
“Fluoroquinolones should not be used in patients at increased risk unless there are no other treatment options available.
Health care professionals should avoid prescribing fluoroquinolone antibiotics to patients who have an aortic aneurysm or are at risk for an aortic aneurysm, such as patients with peripheral atherosclerotic vascular diseases, hypertension, certain genetic conditions such as Marfan syndrome and Ehlers-Danlos syndrome, and elderly patients.”
Upper Respiratory Infections Are Often Viral
Viruses commonly trigger upper respiratory infections (URIs) with symptoms of runny nose, cough, low grade fever, sore throat and difficulty sleeping. URIs represent the most common acute illness in the outpatient setting, often related to the common cold, which is typically a mild, self-limited inflammation of the mucous membranes in the airways.12
Bacterial illness may follow a viral illness as a secondary infection, and commonly includes symptoms persisting longer than 14 days with a fever higher than one might typically expect from a virus. Oftentimes, the fever gets worse a few days into the illness rather than improving.13
Unfortunately, one of the more common reasons fluoroquinolones are prescribed is for upper respiratory infections, ordinarily triggered by a virus. According to the U.S. Centers for Disease Control and Prevention (CDC),14 the highest number of community antibiotic prescriptions are written in the southeastern states.
Fluoroquinolones ranked No. 4 in the highest number of prescriptions written per 1,000 people in the CDC’s outpatient antibiotic prescription index in 2016. Because providers were still opting for fluoroquinolones more than they should for respiratory infections such as pneumonia, the CDC reported in 2021 that an expert panel had recommended the use of these drugs for this purpose be lowered by 90%.15
Bacterial and viral infections are dissimilar in important respects related to the organism’s structure and the way they respond to medications. Although both are too small to be seen with the naked eye, the largest virus is actually smaller than the smallest bacteria.16 Unlike the more complex bacteria, viruses cannot survive without a host and only reproduce by attaching themselves to other cells. Also, unlike bacteria, most viruses are specific in the cells they attack.
The differences in the structure and complexity of the organism have an impact on the type of medication that may be effective against it. Viral infections are not affected by antibiotics such as fluoroquinolones. In fact, using antibiotics for viral infections only contributes to the rising number of antibiotic-resistant infections.
Fluoroquinolones Linked to Multiple Health Concerns
Fluoroquinolone antibiotics have been associated with Achilles tendon ruptures and damage for over a decade. Other severe adverse events, such as retinal detachments as well as aortic aneurysms, may also be associated with other systems requiring collagen formation.17 This may also explain, at least in part, how the drug increases your risk of aortic rupture or dissection, as collagen18 lines your arteries and veins to allow for stretch as the heart pumps blood.19
Subsequently, in July 2022 the FDA mandated another warning, “alerting physicians to the increased risk of tendonitis and tendon rupture associated with their use.”20 According to Dr. Renata Albrecht, who heads the FDA’s Division of Special Pathogen and Transplant Products, ‘Achilles’ ruptures associated with fluoroquinolones are three to four times more frequent than ruptures among people not taking these drugs.21
So, if you are taking these antibiotics, you should seek immediate medical care if you experience soreness or inflammation in muscles or tendons. You should also not exercise while your joints are affected.
The drugs are also powerful iron chelating agents that may trigger epigenetic changes through the loss of agents requiring iron as a cofactor. As noted in one study, this may also explain the classic renal toxicity associated with the antibiotics:22
“At sub-millimolar concentrations, these antibiotics inhibited jumonji domain histone demethylases, TET DNA demethylases and collagen prolyl 4-hydroxylases, leading to accumulation of methylated histones and DNA and inhibition of proline hydroxylation in collagen, respectively. These effects may explain fluoroquinolone-induced nephrotoxicity and tendinopathy.”
A recent study23 has linked the use of fluoroquinolones to the rising number of children and adults affected by kidney stones. The odds of stones increased 1.5 times with the use of fluoroquinolones and exposure within 3 to 12 months was associated with greater risk. It appeared children and adolescents were particularly susceptible.
Reactions can be bodywide, impacting your central nervous system and musculoskeletal, visual and renal systems, sometimes simultaneously. Among the serious reactions reported are:24
| Memory impairment | Delirium | Agitation |
| Disorientation | Retinal detachment25 | Hearing loss and/or tinnitus26 |
| Disturbance in attention | Kidney stones | Kidney failure27 |
| Hypoglycemia leading to coma | Aortic rupture or dissection | Tendon rupture or dissection |
More Psychiatric Side Effects Than You Might Imagine
Researchers recommend further study to understand the pathogenesis caused by antibiotics in order to treat antibiotic-associated diseases through the mitigation of the intestinal environment — restoring it to its original state.28
Further research has demonstrated an imbalance in gut microbiome caused by antibiotics can negatively affect health in a number of ways and for long periods of time.29 If your physician prescribes one of these dangerous antibiotics, ask to use another one. It would be unusual a fluoroquinolone would be the only antibiotic that could be used to treat your infection.
Remember, these dangerous antibiotics should be used as a last resort only. If it is necessary, be sure to carefully read the package insert and all the warnings, and seek medical attention the moment you notice a side effect.
The late Dr. David Flockhart, who served as professor of medicine and chief of clinical pharmacology at Indiana University School of Medicine, and who before his death was considered one of the leading experts in fluoroquinolone side effects, said in 2012 that “as many as one-third of patients taking a fluoroquinolone will experience some sort of psychiatric side effect.”30
But the thing is, Flockhart had tried to call attention to these drugs over 10 years earlier, in 2001, when he decried Ciprio specifically, as he tried to stress just how dangerous fluoroquinolones are:31
“Cipro is basically a big gun whose benefits outweigh its risks in certain circumstances. But the bigger the gun you use, the more damage you can expect as collateral.”
Antibiotics Trigger Permanent Changes to Your Gut Microbiome
The health of your gut microbiome is a game changer. It has become increasingly apparent in recent years that the composition of your gut microbiome plays an enormous role in your health and disease prevention. Cancer and many other health conditions have been traced back to the influence of gut microbes, including obesity, depression, Parkinson’s and allergies, just to name a few.
Since your gut is the main residence of your immune system,32 disrupting your gut microbiome automatically disrupt your immune function, which can have far-reaching consequences. One way antibiotics can promote disease is by creating an oxygen-rich environment in your intestines, favoring the growth of pathogenic bacteria.
Beneficial microbes grow in an anaerobic (no oxygen) environment, while pathogenic bacteria need oxygen to survive.33 Data suggest even one course of antibiotics can negatively alter your microbiome for up to one year, which is why it’s crucial to use antibiotics only when it is absolutely necessary.34
However, Dr. Martin Blaser with the Langone Medical Center at New York University argues the impact of antibiotics on gut bacteria may be permanent. In an editorial in Nature he writes:35
“Early evidence from my lab and others hint that, sometimes, our friendly flora never fully recover. These long-term changes to the beneficial bacteria within people’s bodies may even increase our susceptibility to infections and disease.
Overuse of antibiotics could be fueling the dramatic increase in conditions such as obesity, Type 1 diabetes, inflammatory bowel disease, allergies and asthma, which have more than doubled in many populations.”
Support Your Health and Your Gut
The stronger your immune system, the less chance any microbe will have of gaining a foothold in your body. Below are some basic strategies for supporting your immune system and preventing illness.
| Optimize your diet — Avoid foods that tax your immune system, such as trans fats, fried foods, processed foods, sugars and grains. Seek to reduce your net carbohydrate (sugar, grains, fructose) and protein intake, replacing them with high-quality healthy fats. |
| Balance your gut flora — One of the best ways to support your gut is by incorporating naturally fermented foods into your diet, working up to 4 to 6 ounces per day. You may take a high-quality probiotic supplement, but fermented foods tend to offer the greatest benefit. |
| Exercise regularly — Exercise improves the circulation of immune cells in your blood, creating a more efficient system at locating and eliminating pathogens in your body. Make sure your fitness plan incorporates weight training, high-intensity exercises, stretching and core work. |
| Get plenty of restorative sleep — Research shows sleep deprivation has the same effect on your immune system as physical stress or disease, which is why you may feel ill after a sleepless night. |
| Reduce stress — High levels of stress hormones can diminish your immunity, so be sure you’re implementing some sort of stress management. Meditation, prayer, yoga and Emotional Freedom Techniques (EFT) are all excellent strategies for managing stress, but you’ll have to find what works best for you. |
| Optimize vitamin D levels — Studies show inadequate vitamin D can increase your risk for MRSA and other infections. Your best source of vitamin D is through sensible sun exposure. Monitor your vitamin D level to confirm they’re in a therapeutic range of 60 to 80 ng/mL. If you can’t get UV exposure, consider taking an oral vitamin D3 supplement, in conjunction with magnesium and vitamin K2 (MK-7). |
In addition to the lifestyle measures listed above, there are natural agents that are naturally antibacterial, including the following:
| Vitamin C — Vitamin C’s role in preventing and treating infectious disease is well established. Intravenous vitamin C is an option, but if you don’t have access to a practitioner who can administer it, liposomal vitamin C is the most potent oral form. For more information on vitamin C, listen to my interview with Dr. Ronald Hunninghake (hyperlinked above), an internationally recognized vitamin C expert. |
| Garlic — Garlic is a powerful antibacterial, antiviral and antifungal. It can stimulate your immune system, help wounds heal and kill antibiotic-resistant bacteria. For highest potency, the garlic should be eaten fresh and raw (chopped or smashed). |
| Olive leaf extract — In vitro studies show olive leaf extract is effective against Klebsiella, a gram-negative bacteria, inhibiting its replication, in addition to being toxic to other pathogenic microbes. |
| Manuka honey — Manuka honey, made from the flowers and pollen of the Manuka bush, has been shown to be more effective than antibiotics in the treatment of serious, hard-to-heal skin infections. Clinical trials have found Manuka honey can effectively eradicate more than 250 clinical strains of bacteria, including resistant varieties such as MRSA. |
| Tea tree oil — Tea tree oil is a natural antiseptic proven to kill many bacterial strains.36 |
| Colloidal silver — Colloidal silver has been regarded as an effective natural antibiotic for centuries, and recent research shows it can even help eradicate antibiotic-resistant pathogens. If you are interested in this treatment, make sure you read the latest guidelines for safe usage of colloidal silver as there are risks with using it improperly. |
- 1 American Microbiome Institute, January 20, 2016
- 2 Institute of Science for Society February 26, 2014
- 3 Drugs.com, Antibiotics Guide
- 4, 6 Food and Drug Administration, July 26, 2016
- 5 Food and Drug Administration, A Guide to Drug Safety Terms at the FDA
- 7, 10 Food and Drug Administration, December 20, 2018
- 8 FDA. FDA Updates Warnings for Oral and Injectable Fluroquinolone Antibiotics Due to Disabling Side Effects. January 19, 2022
- 9 Frontiers in Medicine. April 29, 2022
- 11 NBC News, December 20, 2018
- 12 Medscape, Upper Respiratory Tract Infection
- 13 Duke Health, October 1, 2013
- 14 Centers for Disease Control and Prevention, Outpatient Antibiotic Prescriptions — United States, 2016
- 15 CDC. 2021 Update on Antibiotic Use in the United States. 2021
- 16 Mayo Clinic. Bacterial vs. Viral Infections: How Do They Differ?
- 17 BMJ Open, 2015; 5(11)
- 18 Collagen, G.A. Holzapfel, P 285
- 19 Collagen Complete, Did You Know That the Walls of Your Blood Vessels are Lined With Collagen and Elastin?
- 20, 21 ABC News. FDA Mandates Black Box Warning for Some Antibiotics. July 9, 2022
- 22 Journal of Biological Chemistry, 2015;290(36):22287
- 23 Renal and Urology News, May 15, 2018, Kidney Stones Linked to Oral Antibiotics
- 24 MPR, July 10, 2018
- 25 JAMA, 2012;307(13)
- 26 Ther Adv Drug Saf. 2018 Apr; 9(4): 219–221
- 27 Drug Safety, 2000;22(6):479
- 28 Yonsei Medical Journal, 2018;59(1):4
- 29 Frontiers in Microbiology, 2015;6:1543
- 30 Forbes, Antibiotic Alert: The Drug the Doctor Ordered Could Cause Deadly Side Effects, September 30, 2012
- 31 UCLA Department of Epidemiology, “Drug of Choice Has a Downside,” October 29, 2001
- 32 Hopkinsmedicine.org, November 2015
- 33, 34 Cell Host & Microbe 2016;19(4):443
- 35 Wired, August 26, 2011
- 36 Journal of Hospital Infection, 2004;56(4):283