Antibiotics
now browsing by category
Achilles Tendon Injuries Are Rising Among Athletes
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2026/01/14/rising-achilles-tendon-injuries.aspx
Analysis by Dr. Joseph Mercola January 14, 2026

Story at-a-glance
- The Achilles tendon, the body’s longest and strongest connective tissue, links your calf muscles to the heel. It supports walking and jumping, withstands extreme loads, yet faces rising injury rates across populations
- National U.S. data from 2001 to 2020 show Achilles ruptures are the most common tendon injury, increasing about 3% annually, with higher risk in men and Black patients
- Research indicates Achilles ruptures develop from long-term overload and silent degeneration, worsened by sudden training changes, poor foot mechanics, limited recovery, and metabolic conditions like obesity and insulin resistance
- Certain medications, especially fluoroquinolone antibiotics and corticosteroids, directly weaken tendon collagen, sharply increasing rupture risk soon after use, particularly with higher or repeated doses
- Prevention focuses on gradual training progression, adequate rest, supportive footwear, metabolic health, and sufficient collagen intake from sources like bone broth to strengthen tendon structure before pain appears
The Achilles tendon is one of the most important connective tissues in your feet. Moreover, it’s the longest and strongest tendon in your entire body, connecting your calf muscles to the heel bone. In fact, it can withstand up to four times your body weight and allows plantar flexion of your feet — an essential movement allowing you to walk, run, and jump.1
However, experts are now noticing an uptick in Achilles tendon injuries from all walks of life. In a report from CNN, it’s not just professional athletes who are getting this injury. High-profile actors and ordinary people exercising at the gym have also torn their Achilles tendon.2 Numerous factors have been implicated in this issue, and a 2025 study shows that everyone, including you, could be at risk.
Data Confirms Achilles Ruptures Are Accelerating
A study published in The Orthopaedic Journal of Sports Medicine mapped out the rising rates in Achilles tendon ruptures in America. For the analysis, the researchers combed through data from 2001 through 2020. Specifically, they used the National Electronic Injury Surveillance System, a large federal database designed to track injury-related emergency visits across a representative sample of U.S. hospitals. This approach allowed the authors to estimate national trends rather than isolated regional snapshots.3
• The current state of Achilles tendon injuries — Across the study period, 235,189 emergency department visits for acute primary tendon ruptures were recorded. Among all tendon injuries, Achilles tendon ruptures stood out as the most common, accounting for 38.2% of cases. Other injuries included the biceps brachii (16.2%) and patellar tendon (12.7%).
• There is a clear, upward trend — The researchers calculated an average annual increase of about 3% in tendon rupture incidence over the 20-year analysis. Interestingly, that rise did not flatten out or reverse toward the end — it continued.
• A breakdown of risk by sex — Men experienced Achilles tendon ruptures at far higher rates than women, with an incidence rate of 2.46 per 100,000 person-years for men compared with just 0.48 for women. That translates to a male-to-female incidence rate ratio of roughly 5 to 1.
• Race-based differences — Black patients showed the highest overall incidence rate of tendon ruptures, at 4.78 per 100,000 person-years, compared with lower rates in White and other racial groups. The study did not specify an explanation for this gap, but it highlighted that tendon rupture risk does not distribute evenly across the population.
• Everyone could be at risk — A steadily rising injury rate over 20 years points to systemic drivers rather than isolated accidents. This means lifestyle changes, occupational demands, recreational exercise trends, and broader health factors likely shape tendon strength long before the rupture occurs. If you wait until pain forces you into an emergency room, the problem has already progressed too far.
The researchers also emphasized that the records were acute primary ruptures, not repeat injuries or complications from prior tears. That distinction matters because it shows the increase in injury rates does not come from poor recovery alone — it reflects a growing vulnerability in the population.
Mapping the Drivers Behind Achilles Rupture Risk
In a study published in the Journal of Orthopaedic Translation, researchers set out to identify why Achilles tendon ruptures continue to rise despite better awareness, training tools, and medical care. The researchers reviewed clinical evidence on rupture risk factors and prevention strategies, with a specific focus on how modern lifestyles affect tendon health.4
The paper focused on adults with Achilles tendon injuries across both athletic and non-athletic populations, reflecting real-world conditions rather than elite performers alone. The researchers also emphasized that ruptures increasingly affect people who exercise recreationally, work physically demanding jobs, or have metabolic disorders.
After analysis was complete, they noted that an Achilles tendon rupture is not a random event — it is the result of repeated tissue overload combined with biological weakening that goes unnoticed until failure occurs.
• Risk builds up long before pain appears — The researchers explained that many people develop silent tendon degeneration over time, meaning the tissue structure slowly weakens without obvious symptoms. This condition leaves the tendon vulnerable to sudden rupture during routine activity.
• Sudden changes in training patterns increase risk — Abrupt changes in physical load are a major driver of rupture risk. For example, sudden increases in running volume, intensity, or explosive movement place stress on the tendon fibers faster than they can repair.
• Foot and ankle mechanics also play a role — The authors described how abnormal foot alignment, limited ankle mobility, and poor force distribution increase localized strain within the Achilles tendon. Over time, this uneven stress degrades the collagen fibers.
• Metabolic health emerged as another overlooked factor — Conditions such as obesity, insulin resistance, and chronic inflammation impair tendon repair. Just like every other process in your body, the tendons also rely on steady nutrient delivery and efficient cellular repair. When those processes slow down, microscopic damage accumulates faster than your body fixes it.
• Drugs also weaken tendons — Certain drugs interfere with tendon cell function and collagen maintenance, making the tissue more fragile under normal loads. While the study didn’t go into detail about the mechanisms, it listed the following drugs as modifiable risk factors:
◦ Fluoroquinolones
◦ Antimicrobial drugs
◦ Statins
◦ Corticosteroids
◦ Aromatase inhibitors
◦ Anabolic steroids
◦ Isotretinoin
◦ Renin-angiotensin system drugs
◦ Thiazide diuretics and calcium channel blockers
• A comparison of compared modifiable and non-modifiable risk factors — Age, sex, and genetic structure fall outside your control, but training design, recovery time, metabolic support, and mechanical alignment do not. The review stressed that focusing only on unchangeable factors leads to missed prevention opportunities. In other words, the risk of injuring your Achilles tendon is something you can influence through choices, not chance or plain bad luck.
• The paper discussed why prevention often fails — Many people rely on pain as a warning sign, yet tendon degeneration progresses quietly. By the time discomfort appears, structural damage already exists.
• How tendon breakdown occurs at the microscopic scale — Collagen fibers lose organization, and enzymes that degrade connective tissue increase in activity. At the same time, oxidative stress rises inside tendon cells, reducing their ability to maintain strong fibers.
• Another mechanism involves blood supply — The Achilles tendon has limited circulation compared to muscle, which slows healing. When combined with metabolic strain or medication effects, this low blood flow leaves the tendon vulnerable. The researchers describe the process below:5
“[T]he middle Achilles tendon part is the least supplied with blood, relying on capillaries in the surrounding connective tissue for reperfusion. Under increased load, these areas are more prone to hypoxia and metabolic disturbances, leading to dystrophic changes.
Poorly supplied tendon parts exhibit higher temperature regimes, which increase the elastic component and significantly reduce tendon fiber strength.”

Save This Article for Later – Get the PDF Now
Could Taking Antibiotics Weaken Your Achilles Tendon?
As mentioned earlier, drugs are a factor in deteriorating tendon health. Now, a study published in the Journal of Sport and Health Science followed this angle, specifically investigating whether commonly prescribed oral fluoroquinolone antibiotics raised the risk of Achilles tendon injury compared with another widely used antibiotic, amoxicillin.6
The research team used a nationwide Danish health registry data in a nested case-control design, which means they compared people who experienced Achilles tendon lesions or ruptures with carefully matched individuals who did not. The goal was straightforward — determine how strong the association is, how quickly the risk appears after exposure, and whether dose matters.
• Risk quickly rises — Within the first 60 days after fluoroquinolone use, the risk was 3.6 times higher in the two months after taking the drug compared to amoxicillin. Even at 90 days, the risk remained high at 2.74, and in one year it stayed elevated at 1.49.
• The impact of dosage — The researchers measured cumulative defined daily doses, which reflects how much of the antibiotic a person consumed over time. Individuals who accumulated more than 10 defined daily doses had a significantly higher risk of Achilles tendon injury than those with lower exposure. This means that longer or repeated courses raise risk more than a short exposure, especially if prescriptions stack up over time.
• What happens when other medications enter the picture — People who experienced Achilles injuries more often have recent exposure to oral glucocorticoids compared with controls. Specifically, about 6% of cases had used glucocorticoids versus 2% of controls. Thus, if you’re an athlete taking both antibiotics and steroids within a short window, your Achilles tendon faces further increased risk.
• How fluoroquinolones affect tendon tissue directly — These drugs interfere with collagen synthesis, meaning they disrupt the process by which tendon cells maintain and repair their structural fibers. Collagen acts like tightly woven rope strands and when these weaken, the tendon loses tensile strength.
• Beware of antibiotics on your connective tissues — By quantifying how strongly and how quickly fluoroquinolones raise Achilles tendon rupture risk, this research adds a critical piece to the larger picture. It shows that modern injury patterns do not stem only from movement or training habits. Sometimes, the trigger comes from a prescription, quietly weakening tissue until the tendon reaches its breaking point.
Some Tips to Protect Your Achilles Tendon
Going back to the CNN report, it’s noted that everyone who is 35 to 50 years old can tear their Achilles tendon. However, there are several things you can do to lower the risk:7
• Get enough rest — After a strenuous game or exercise session, give your body enough time to recover, especially if you’ve been using your legs a lot.8 This tactic allows your tissues to adapt and preventing overuse injuries.9
• Gradually increase intensity — Slowly ramping up exercise intensity, coupled with proper rest, helps lower the risk of injuries.10
• Buy good shoes — Many people overlook the importance of proper footwear when it comes to preventing injuries. According to a study published in the Clinical Journal of Sport Medicine, high-top shoes can significantly reduce tension in the Achilles tendon compared to low-top shoes.11
In another study, shoes biased to forefoot landing was found to improve Achilles tendon loading, “and may be useful for progressing loading prior to introducing more advanced movements.”12
• Reduce vegetable oil consumption — As noted earlier, metabolic disorders have been identified as a risk factor, which is likely influenced by a diet high in linoleic acid (LA).
LA affects your overall metabolic health and ability to produce healthy cellular energy. That said, keep your intake to below 2 grams per day from all sources, such as soybean, cotton, and safflower oil. In addition, avoid ultraprocessed foods, as these also contain LA. Next, add in healthy fat sources, such as coconut oil and grass fed tallow or ghee.
To help monitor your intake, sign up for the upcoming Mercola Health Coach app. It contains the Seed Oil Sleuth, which helps monitor your LA intake to a tenth of a gram.
Support Your Achilles Tendon with Collagen
Collagen is the main structural protein found in your skin, tendons, and bones, as well as playing a crucial role in many bodily functions.13 Thus, proper collagen intake is essential to keeping your Achilles tendon strong and flexible, especially if you’re a high-level athlete or fitness enthusiast.
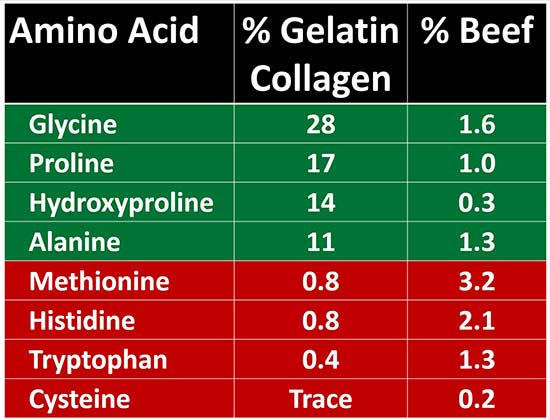
• A primer on collagen sources — For your body to produce collagen, your body will need the right amino acids from animal parts that have them. That’s because red meat alone won’t give your body the amino acids (highlighted in green below). In addition, a high intake of amino acids from red meat (highlighted in red below) can promote inflammation, as well as suppress thyroid function and metabolism.14
• Ideal collagen intake — I recommend that a third of your overall daily protein intake comes from collagen sources, as 30% of your body is comprised of this protein.
• Best source of collagen — For your body to make enough collagen, I recommend making your own bone broth using organic, grass fed animal bones. Gelatinous cuts of meat also work, and you can use slow-cooking or pressure-cooking to make them easier to eat. To learn how to make your own bone broth, read “The Ultimate Guide to Bone Broth: Nature’s Collagen Supplement.”
Frequently Asked Questions About Achilles Tendon Ruptures and Injuries
Q: Why are Achilles tendon injuries becoming more common?
A: Achilles tendon ruptures have increased steadily over the past two decades due to systemic factors like lifestyle changes, recreational exercise trends, metabolic health issues, and cumulative tissue overload, not just sports-related accidents.
Q: Who is most at risk for an Achilles tendon rupture?
A: Men face significantly higher risk than women, Black patients show higher incidence rates, and adults aged 35 to 50 are especially vulnerable, though rising trends suggest most people are at risk.
Q: Can Achilles tendon damage develop without warning signs?
A: Yes. Tendon degeneration often occurs silently over years, weakening collagen structure without pain, making sudden rupture possible during routine activities before any symptoms appear.
Q: Do medications affect Achilles tendon strength?
A: Certain drugs, especially fluoroquinolone antibiotics and corticosteroids, impair collagen synthesis and tendon repair, sharply increasing rupture risk shortly after use, particularly with higher or repeated doses.
Q: What steps can help protect the Achilles tendon?
A: Gradual training progression, adequate recovery, proper footwear, minimize LA intake, avoid antibiotics, and sufficient collagen consumption from natural sources like bone broth can strengthen tendon resilience and reduce injury risk.
- 1, 2, 7, 8 CNN, December 3, 2025
- 3, 4, 5, 9, 10 Journal of Orthopaedic Translation Volume 49, November 2024, Pages 289-307
- 6 J Sport Health Sci. 2024 Apr 2;13(6):749–750
- 11 Clinical Journal of Sport Medicine 20(5):p 344-349, September 2010
- 12 Clinical Biomechanics Volume 131, January 2026, 106684
- 13 Polymers (Basel). 2021 Nov; 13(22): 3868, Introduction
- 14 Optimising Nutrition, December 18, 2022
Cystitis vs. UTI — Understanding the Differences
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/11/18/uti-cystitis-awareness.aspx
Analysis by Dr. Joseph Mercola November 18, 2025

Story at-a-glance
- One in three Europeans cannot correctly define cystitis as a bladder infection, with younger adults showing particularly poor awareness of these common conditions
- While UTIs can occur anywhere in the urinary tract, cystitis affects only the bladder; pyelonephritis involves kidneys and requires urgent care
- Studies show up to 85% of UTI diagnoses may be incorrect, often confusing harmless bacterial colonization with actual infection requiring treatment
- Mild uncomplicated cases often resolve with hydration and symptom management; overuse of antibiotics drives dangerous resistance and should be avoided when possible
- Reducing factory-farmed meat, practicing proper hygiene, using methylene blue or cranberry products, and getting sunlight exposure can help prevent recurrent infections
The level of urinary tract infections (UTIs) awareness is far less than what one might expect given how common these conditions are. In a recent international survey published by the European Association of Urology, one in three Europeans could not correctly define cystitis as a bladder infection, with many confusing it for entirely unrelated problems such as skin conditions or allergies.1,2
The knowledge gaps are especially striking among younger adults. Fewer than half of people aged 18 to 24 recognized cystitis for what it is, suggesting that basic education on urological health has failed to reach some of the most vulnerable groups.
The same survey showed that only about half of respondents were aware that women are disproportionately affected by UTIs, despite medical evidence that 50% to 60% of women will experience at least one UTI during their lifetime. Almost one in five men, in fact, incorrectly assumed that males were more likely to be affected.
Misconceptions between terminologies will inevitably contribute to misdiagnosis. In fact, it’s already happening, and these inaccuracies can contribute to delayed treatment and worsening outcomes.
What’s the Difference Between Cystitis and a UTI?
Cystitis is a specific type of urinary tract infection that affects the bladder, but the broader term “UTI” refers to infections that can occur anywhere along the urinary tract, including the urethra, bladder, ureters, and kidneys.
When the infection is confined to the lower urinary tract, it usually manifests as urethritis or cystitis. If it spreads upward, it can involve the kidneys in a condition known as pyelonephritis, which is often more serious and can be life-threatening.3,4
• The most common cause of both cystitis and other UTIs — Uropathogenic Escherichia coli (UPEC) is the root cause, which accounts for the majority of infections in otherwise healthy individuals. Other bacteria such as Klebsiella pneumoniae, Proteus mirabilis, Enterococcus faecalis, and Staphylococcus saprophyticus are also important culprits, particularly in certain populations.
• UTIs are further divided into uncomplicated and complicated types — Uncomplicated infections usually occur in otherwise healthy individuals without structural abnormalities of the urinary tract, whereas complicated UTIs are linked to conditions such as catheter use, urinary tract obstruction, or pregnancy.
• Another source of confusion in diagnosis is interstitial cystitis — Unlike bacterial cystitis, this is a chronic inflammatory condition of the bladder wall with no detectable pathogens. Patients may experience pain, urgency, and frequency similar to cystitis, but cultures are negative. This distinction is vital because mislabeling interstitial cystitis as a recurrent infection can lead to unnecessary antibiotic exposure without relief of symptoms.
The table below provides a quick overview of the differences between each condition:
| Condition | Where is the infection? | Typical symptoms | Why it matters |
|---|---|---|---|
| Cystitis (bladder) | Bladder (lower UTI) | Burning, urgency, frequency, suprapubic pain; usually no fever | Common; can worsen without care |
| Urethritis | Urethra | Burning, possible discharge; consider STIs in differential | Treating the wrong cause (e.g., STI) leads to persistent symptoms |
| Pyelonephritis (kidney) | Kidneys (upper UTI) | Fever, flank/back pain, chills, nausea | Requires prompt medical care to prevent complications |
What Symptoms Should You Watch for in Women, Men, and Older Adults?
The presentation of UTIs varies across different groups. In women, the classic signs are well-known — a burning feeling during urination, an urgent and frequent need to urinate, and sometimes lower abdominal pain or discomfort. Men experience many of the same symptoms, but because UTIs are less common in males, the presence of infection often suggests a more complicated scenario, such as prostate involvement.5
• Older adults are especially challenging to diagnose accurately — While clinicians and caregivers often attribute confusion or sudden changes in mental status to UTIs, research cautions against reflexively treating every case of bacteriuria in older people as infection.
Asymptomatic bacteriuria is common in this age group, and antibiotics should not automatically be given unless absolutely necessary. Misdiagnosis in older adults is widespread, and it contributes to overtreatment with antibiotics.
• The knowledge gaps revealed by public surveys compound these issues — Younger women, for example, often underestimate their own vulnerability, and many wrongly assume contraceptive methods such as the pill protect against bladder infections. This leads to missed opportunities for prevention and unnecessary suffering when infections occur.

Save This Article for Later – Get the PDF Now
How Are UTIs Diagnosed (and Why Are So Many Misdiagnosed)?
The diagnostic process is straightforward, but limitations in current methods make misdiagnosed UTI cases common. For example, dipstick urine tests are widely used in clinics for their speed and affordability — this process tests for nitrites and leukocyte esterase, which are typical indicators of bacterial presence and inflammation. However, these tests are prone to false negatives and cannot identify the specific organism involved.6,7
• Urine culture has long been considered the gold standard — Results with a bacterial count of at least 100,000 colony-forming units (CFUs) per milliliter serve as the diagnostic threshold. Yet, women with clear symptoms may have counts as low as 1,000 per milliliter of urine, which means traditional culture criteria miss many clinically relevant cases.
Furthermore, cultures can come back negative even when bacteria are present in the bladder, a phenomenon increasingly recognized with advanced diagnostic techniques.
• Misdiagnosis also arises because UTI-like symptoms can overlap with other conditions — Sexually transmitted infections (STIs), overactive bladder, and interstitial cystitis can all mimic the presentation of cystitis, and if clinicians rely too heavily on culture results alone, they risk misclassifying or overlooking these possibilities.
• New tests can offer more accurate results — Advanced tools such as extended quantitative urine cultures, mass spectrometry, and multiplex polymerase chain reaction (PCR) panels have shown promise in detecting pathogens that evade standard testing. While these are not yet widely available, they illustrate why reliance on conventional culture alone can be misleading.
The table below provides an overview of current UTI testing methods:
| What it checks | Strengths | Pitfalls and false results | Practical takeaways | |
|---|---|---|---|---|
| Urine dipstick: nitrite | Bacterial conversion of nitrate → nitrite (often E. coli) | Fast; decent rule-in when positive with symptoms | False-negative with non-nitrite-producing bugs, short bladder dwell time, high vitamin C; false-positive from contamination | Helpful when paired with classic symptoms; don’t treat a lone positive without symptoms |
| Urine dipstick: leukocyte esterase | Marker of white blood cells | Sensitive for inflammation | Not specific to infection (can reflect irritation, vaginitis, STIs); dilution → false-negative | Supportive clue only; absence doesn’t fully exclude UTI if symptoms fit |
| Microscopy (pyuria, bacteriuria) | Cells and organisms | Adds context beyond dipstick | Pyuria may occur without infection; contamination skews results | Interpret with history/exam; repeat clean-catch if contamination likely |
| Urine culture | Identifies pathogen + susceptibilities | Gold standard when symptomatic; guides antibiotics | “No growth” doesn’t explain all dysuria (consider urethritis, Interstitial Cystitis/Bladder Pain Syndrome); slower turnaround | Best for recurrent, atypical, pregnancy, febrile, or non-resolving cases; avoid culturing asymptomatic patients |
| Nucleic Acid Amplification Test (NAAT)/STI testing (when indicated) | Chlamydia, gonorrhea, etc. | Rules in non-UTI causes | Missed when we assume “every burn = UTI” | Consider in sexually active patients with urethral symptoms / discharge |
Do You Always Need Antibiotics for a UTI?
The short answer is no. Not every UTI requires antibiotic treatment. In otherwise healthy women with mild symptoms, many uncomplicated bladder infections can resolve on their own with hydration and symptom management.8,9
• Clinical guidelines emphasize a more nuanced approach — Antibiotics should only be considered in special cases wherein the infection has spread to the kidneys, such as for pregnant women, and when patients present with systemic symptoms such as fever or flank pain. This is done to reduce the risk of antibiotic-resistant bacteria, which can cause problems down the line.
• First-line usage of antibiotics has shifted in response to rising bacterial resistance — Drugs such as nitrofurantoin, fosfomycin, and pivmecillinam are now used in rotation, while fluoroquinolones and aminopenicillins are discouraged due to high failure rates and the risk of lasting side effects.
Going back to the Urology Week survey, 16% of respondents still believe antibiotics are always required. This belief contributes to the overuse of antibiotics and accelerates the rise of resistant pathogens.10 That’s why it’s important to consider natural strategies first.
What Actually Works to Prevent Cystitis and UTIs?
Prevention is particularly important for those who suffer recurrent infections. Some strategies are universally beneficial, while others are more appropriate for certain groups.11
• Increasing daily fluid intake — This has a well-documented effect in reducing recurrence, and is one of the simplest measures available. Urinating after sexual activity is also strongly recommended, especially for younger women, as it helps flush bacteria from the urinary tract. Proper hygiene, such as wiping front to back, remains a cornerstone of prevention.
• For postmenopausal women — Local estrogen therapy can help restore the balance of protective Lactobacillus in the vaginal microbiota and reduce recurrence.
Supplements such as cranberry extracts and D-mannose are also widely used. Natural cranberry products appear to reduce recurrence in some studies but not others, while D-mannose interferes with bacterial adhesion to the bladder wall, offering a potential non-antibiotic option. Methenamine hippurate, a urinary antiseptic, has moderate evidence supporting its use in prevention, though it is not suitable for all patients.
• Prevention strategies are most effective when tailored to individual circumstances — Postcoital UTI prevention through urination are universally recommended, while estrogen therapy is reserved for postmenopausal women, and D-mannose supplements can offer additional support where appropriate. Be sure to consult with your doctor to craft a program specific to your current circumstances.
When Should You See a Doctor — or Go to Urgent Care?
Although many UTIs are mild and self-limiting, there are clear circumstances where medical attention is essential. Fever, flank pain, and chills point toward kidney involvement, which requires urgent treatment.
• Other markers to watch out for — Blood in the urine, recurrent infections within a short period, or any infection occurring during pregnancy also warrant professional care. If mild symptoms do not improve within two to three days of self-care, consult a doctor right away.
• Healthy adults with mild bladder symptoms may safely monitor themselves — Note that this should only last for a day or two while increasing fluid intake. If symptoms persist or worsen, they should seek medical care. More severe presentations, especially those involving systemic symptoms, demand urgent evaluation in primary care or emergency settings.
When Relying Too Much on Urine Tests Backfire
Millions of people visit the emergency room each year due to recurring UTIs, and their diagnoses often miss the mark. Geriatric specialist Dr. Nick Schneeman has criticized the tendency in medicine to assume that an older adult who suddenly feels weak, disoriented, or lightheaded automatically has a UTI.
In his guest article for TIME, Schneeman noted how quickly urine tests are ordered in these cases and how frequently antibiotics are prescribed when bacteria show up, even if the patient never reported hallmark signs such as painful urination, frequent urges, or sudden urgency.12
• The problem of misdiagnosis is widespread — More than half of all women will be told at some point that they have had a UTI, yet research has revealed alarmingly high rates of overdiagnosis. In some regions, studies suggest as many as 85% of cases may be incorrectly labeled. One 2020 analysis of 43 hospitals found that three out of four patients diagnosed with a UTI did not actually meet the clinical criteria.
• Older adults are especially vulnerable — Many already carry harmless bacteria in their urine or bladder, a state known as colonization, which does not require medication. Unfortunately, this is frequently mistaken for infection. The challenge is compounded by the difficulty of obtaining clean urine samples in frail or bedridden individuals, particularly those who rely on adult diapers. Contamination is common, and it often produces misleading results.
•Clinicians are drawn to the convenience of testing — A urine culture is fast and easy, making it a default step in hospitals and clinics. But convenience should not be confused with accuracy. Relying on lab findings without aligning them to a patient’s actual symptoms risks unnecessary treatment and fails to get to the true source of the problem.
Address UTIs with These Steps
If you’ve been dealing with repeat urinary tract infections, it’s time to take a closer look. UTIs are frequently misidentified, especially in older adults, and antibiotics are often prescribed without a clear understanding of the real underlying issue.
That approach not only fails to solve the problem but can also do harm. Instead of relying solely on quick prescriptions, focus on practical steps that address the root causes and minimize recurrences:
1. Reconsider your diet, particularly when it comes to meat — Research shows that certain UTI-causing strains of E. coli are introduced into the body through food, especially factory-farmed chicken, but also pork and beef from concentrated animal feeding operations (CAFOs). Thus, reducing or eliminating industrially farmed meats, particularly poultry, from your diet can lower your risk of exposure to resistant bacteria.
If you do choose to eat animal products, look for grass fed beef or pasture-raised options from farmers following biodynamic, regenerative practices. Chicken, particularly organic and free-range varieties, are safer. However, I don’t encourage it because chicken meat generally contains high amounts of linoleic acid.
2. Good hygiene habits remain a cornerstone of prevention — Small everyday habits can have big effects. For example, always wipe front to back after using the bathroom to minimize the chance of transferring bacteria toward the urethra. If you’re prone to UTIs, or if you’re a caregiver for someone at higher risk, a bidet can be more effective than toilet paper for reducing bacterial spread.
Showers are generally preferable to baths, and a quick wash before sexual activity can make a meaningful difference in preventing bacteria from entering the urinary tract.
3. Consider natural strategies that strengthen the urinary tract’s defenses — Pharmaceutical-grade methylene blue has been studied for its ability to concentrate in the bladder and directly suppress harmful bacteria, offering a targeted approach without broadly disturbing the body’s microbiome the way antibiotics often do.
If you currently have UTI, a 65-milligram tablet, taken thrice daily with water and meals, may help. Combining this with organic cranberries or unsweetened cranberry juice provides an added layer of defense by making it harder for bacteria to cling to the lining of the urinary tract. Together, they form a potent protective duo.
4. Don’t underestimate the power of sunlight — Appropriate sun exposure stimulates cellular energy production, which strengthens the immune system’s ability to fight infection. However, if your diet still contains large amounts of LA from vegetable oils such as soybean, corn, or canola oil, your skin is more vulnerable to ultraviolet damage.
LA accumulates in your tissues and oxidizes rapidly under sunlight, driving inflammation and oxidative stress. By removing them from your diet for several months, you create conditions for safer sun exposure during peak hours, ultimately supporting mitochondrial function and immune resilience. For a more in-depth explanation of this approach, read “The Fast-Track Path to Clearing Vegetable Oils from Your Skin.”
5. Practice grounding — This is an approach wherein you reconnect yourself, literally, with the Earth’s electrical field to restore cellular balance. But not all environments are equally beneficial.
In much of North America, land-based grounding is often disrupted by electromagnetic interference from power lines and urban infrastructure. The ocean, however, provides a cleaner connection. Saltwater conducts energy efficiently, allowing your body to release excess charge and reestablish its natural electrical state. Thus, walking barefoot along the shoreline or immersing yourself in the sea can be a more effective way to experience the benefits of grounding.
Frequently Asked Questions (FAQs) About Cystitis And UTIs
Q: What’s the difference between cystitis and UTI?
A: Cystitis is a specific type of urinary tract infection (UTI) that affects the bladder, while UTIs can involve any part of the urinary tract, including the urethra, bladder, ureters, or kidneys. A bladder infection is usually uncomfortable but rarely dangerous if treated, whereas an upper UTI such as pyelonephritis (kidney infection) can become serious.
Interstitial cystitis, sometimes confused with bacterial infections, is a chronic bladder condition not caused by bacteria and requires different management.
Q: What are the red flags that a UTI needs urgent care?
A: Most bladder infections cause burning with urination, urgency, or frequency, and these can often be managed with simple care. But there are warning signs that point to a more serious infection. If you develop fever, flank pain, chills, or nausea, the infection may have spread to your kidneys and requires immediate medical attention. Blood in the urine, persistent symptoms lasting more than two to three days, or any infection during pregnancy are also urgent red flags.
Q: What are the most commonly asked UTI questions?
A: Patients frequently ask about what causes UTIs, whether they can be prevented, whether they are contagious, and how they are treated. Many also wonder if men can get UTIs, how children are affected, and whether lifestyle habits like sexual activity or hygiene increase risk. These questions reflect the uncertainty many people feel when faced with recurrent or confusing symptoms.
Q: How many UTIs count as “recurrent” and who’s at risk?
A: Doctors generally define recurrent UTIs as three or more infections in a single year or two or more in six months. Women, older adults, and those with structural issues in the urinary tract are most at risk. Pregnancy also changes risk patterns because of hormonal shifts and changes in urinary flow.
Q: What should I ask my clinician about preventing future UTIs (including during pregnancy)?
A: If you have had more than one infection, it’s reasonable to ask your doctor about strategies to lower your risk. Questions include whether you should drink more fluids, urinate after sex, or consider supplements like cranberry or D-mannose. Postmenopausal women want to ask about vaginal estrogen, while pregnant women should ask which preventive steps are safe during pregnancy and whether antibiotics are necessary for asymptomatic bacteriuria.
Q: Which three questions should I ask myself before assuming it’s a UTI?
A: “Am I experiencing the classic UTI symptoms of pain or burning when urinating, urgency, or frequency?” Another one is, “Could these symptoms be due to another cause, such as vaginal irritation or an STI?” And finally, “Do I have additional signs like fever or flank pain that might suggest something more serious?” Thinking through these questions can help you decide whether to try self-care briefly, call your doctor, or head to urgent care.
Q: What do patients usually ask about recurrent UTIs and vaginal estrogen?
A: Urologists frequently hear questions about why UTIs keep coming back, whether antibiotics are the only solution, and whether supplements or non-antibiotic strategies can help. For postmenopausal women, one of the most common questions is about vaginal estrogen — what it is, whether it works, and if it is safe. Clinicians often explain that estrogen helps restore healthy bacteria in the vaginal environment and reduces recurrence, but it is only recommended in certain cases.
- 1 News-Medical, September 22, 2025
- 2, 10 EuroWeb, September 22, 2025
- 3, 5, 6, 9 Diseases. 2025 Feb 15;13(2):59
- 4, 7, 8, 11 Pathogens 2023, 12(4), 623
- 12 TIME, March 13, 2025
Types of Medications That Harm Your Kidneys
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/28/medications-that-damage-kidneys.aspx
Analysis by Dr. Joseph Mercola July 28, 2025

Story at-a-glance
- Common medications like NSAIDs, antibiotics, acid blockers, and laxatives quietly damage your kidneys, even when used as directed
- Kidney symptoms often show up late, so damage is underway before you feel anything, especially if you’re older or taking multiple prescriptions
- NSAIDs reduce blood flow, antibiotics clog, or inflame kidney filters and proton pump inhibitors trigger immune reactions that harm kidney tissue
- Imaging contrast dyes used in CT or MRI scans sharply reduce kidney function in vulnerable people, particularly those with diabetes or dehydration
- Reviewing your medications regularly, leading a healthy lifestyle and using natural alternatives help reduce your kidney burden and prevent long-term harm
Kidney damage doesn’t always start with disease — it often starts with prescriptions. Many of the medications you’ve been told are safe are filtered through your kidneys, creating a constant workload that backfires over time. As drug use climbs, so does the hidden toll on this key organ.
Your kidneys handle far more than waste. They help balance fluids, regulate blood pressure, and support red blood cell production. But the more medications your body has to process, the more strain your kidneys are under, especially if you’re older, managing chronic illness, or taking multiple prescriptions.
Most people don’t think to question their medications until something goes wrong. But when kidney function declines, the signs often show up late, after the real damage has been done. That’s why catching the risk early matters. Let’s break down which drug classes pose the greatest kidney risks — and what to do to stay protected.
NSAIDs and Other Painkillers Are Tough on Your Kidneys
An article, published by AARP, highlighted how widely used medications, including both over-the-counter (OTC) and prescription drugs, damage your kidneys even when taken as directed.1 The most vulnerable include older adults, people with diabetes, and anyone who’s dehydrated or managing other illnesses. However, even people without diagnosed kidney issues are at risk if they take multiple medications or ignore dosage guidelines.
• Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce blood flow to your kidneys — Drugs like ibuprofen and naproxen, often used to relieve pain, inflammation, or fever, work by blocking enzymes that cause inflammation. But they also reduce a hormone that keeps the blood vessels in your kidneys open. Without enough of that hormone, these vessels narrow, making it harder for blood to flow in. This leads to reduced kidney function, especially during illness or if you’re dehydrated.
• Don’t take them for too long — Clinical pharmacist Derek Owen, with the University of Chicago Department of Medicine, told AARP that NSAIDs shouldn’t be taken for more than 10 days in a row for pain, or more than three days for fever. These drugs seem harmless because they’re sold over the counter, but regular or prolonged use does real damage.
• Taking NSAIDs with blood pressure and water pills is dangerous — When NSAIDs are combined with ACE inhibitors (for blood pressure) and diuretics (to reduce swelling or fluid buildup), your kidneys are hit from multiple angles. This combination reduces blood flow and filtration pressure, leading to a dangerous drop in kidney function — often without early symptoms. It’s called the “triple whammy” for a reason.
• Get simple tests to check your kidneys — Your doctor can run basic lab tests to measure how well your kidneys are filtering waste and whether they’re leaking protein. Catching small changes early helps you adjust your medications before permanent damage occurs.
Antibiotics, Antivirals, and Immunosuppressants Are Powerful Drugs with Hidden Risks
Antibiotics, antivirals, and immunosuppressants come with serious risks for your kidneys. Even when taken as prescribed, these medications disrupt filtration, block urine flow or cause direct damage if not carefully managed.2
• Some antibiotics damage kidney cells directly — Drugs like tobramycin are especially hard on your kidneys. They build up inside the tiny filtering cells and cause structural damage. The longer these antibiotics are used, the greater the risk, which is why they’re usually only given in short courses under close supervision.
• Others block urine flow — Sulfonamides, another type of antibiotic, form crystals that don’t dissolve well in urine. If you’re dehydrated or your urine flow is slow, these crystals clog the tiny tubes in your kidneys, leading to inflammation, back pressure, and pain. Even if you don’t notice right away, your creatinine levels could start creeping up — a warning sign that filtration is slowing down.
• Doses need to match how well your kidneys are working — If your kidneys aren’t filtering properly and the dose isn’t adjusted, drugs like amoxicillin and ciprofloxacin build up and become harmful. In some cases, they even cause an allergic reaction in the kidneys, leading to swelling and more damage.3
• HIV and transplant drugs also harm your kidneys — Medications like tenofovir for HIV and cyclosporine to prevent organ rejection reduce blood flow in the kidneys and damage the same cells that handle waste removal. People taking these drugs are often on complex medication regimens, making it even more important to track kidney labs regularly.4

Save This Article for Later – Get the PDF Now
Proton Pump Inhibitors and Other Acid Suppressants Are Quiet Contributors to Chronic Kidney Trouble
Proton pump inhibitors (PPIs), such as omeprazole (Prilosec), esomeprazole (Nexium) and lansoprazole (Prevacid), are widely used to reduce stomach acid. They’re commonly taken for heartburn, indigestion, or ulcers, sometimes for years. But long-term PPI use is linked to chronic kidney disease.5
• They inflame your kidney’s filters — PPIs are associated with a condition called interstitial nephritis, an allergic-type reaction that causes swelling in the spaces between kidney structures. This leads to fatigue, swelling in your legs, and darker urine. Because the symptoms are sometimes mild or vague, they often go unnoticed until serious damage has occurred.
• People often stay on these drugs too long — Many start taking PPIs for temporary symptoms but never stop. If you’re using PPIs, taper off slowly and switch to famotidine (Pepcid), a safer option that not only avoids PPI-related heart risks but also helps block excess serotonin that disrupts energy and drives inflammation.
• Lifestyle changes often replace the need for acid blockers — Low stomach acid — not high — is often the actual problem behind acid reflux. The solution isn’t just symptom relief with drugs. It’s optimizing your mitochondrial function to restore the foundation that helps your stomach break down food, absorb nutrients, and protect you from pathogens.
Laxatives Seem Harmless but Quietly Hurt Your Kidneys
Stimulant laxatives like senna and osmotic types like Miralax work by pulling water into your intestines or speeding up how fast things move through your gut. But if you’re not drinking enough fluids — or if you use these products regularly — you lose too much water. That drop in body fluid also reduces blood flow to your kidneys, making it harder for them to do their job.6
• Long-term use often leads to kidney stones — When you’re dehydrated, your urine becomes more concentrated with minerals like calcium and oxalate. Over time, these minerals form crystals and turn into kidney stones. These stones often block urine flow, cause pain and damage the kidneys further if not treated.
• Frequent laxative use is more common than you think — Many people use laxatives several times a week, or even daily, without realizing it could be hurting their kidneys. This is especially true for older adults who are already prone to dehydration or who are on other medications that affect kidney function.
• There are safer, natural ways to manage constipation — Instead of relying on laxatives, try focusing on your gut health and increasing your intake of fiber-rich foods like fruit and vegetables. Drinking more water and moving your body daily also support regular bowel movements.
• Ask your doctor about safer options — If you feel like you can’t go without laxatives, talk to your integrative health care provider. You could have an underlying issue, like low stomach acid, a sluggish thyroid or imbalanced gut bacteria, that’s better off fixed naturally, without risking damage to your kidneys.
Imaging Contrast Dyes Overload Your Kidneys
Doctors often use contrast dyes during CT or MRI scans. These dyes highlight organs and blood vessels, but they also pass through your kidneys. In some people, especially those with diabetes, heart disease or reduced kidney function, these dyes reduce blood flow and damage the filters inside the kidneys.7
• Iodine-based contrast from CT scans trigger acute kidney problems — Some contrast agents contain iodine, which your kidneys have to filter out. In people with existing kidney concerns, this sudden workload leads to contrast-induced nephropathy, a condition where kidney function drops sharply within 48 hours of the scan.
• MRI dyes carry a different kind of risk — Gadolinium-based contrast dyes, used in MRI scans, have been linked to a rare condition called nephrogenic systemic fibrosis. This causes thickening of the skin and connective tissue, mainly in people with severely impaired kidney function.
• The risks go up if you’re sick or dehydrated — If you have a chronic illness, are already taking multiple medications or haven’t been drinking enough fluids, your kidneys could be too stressed to handle the extra load from imaging dyes. The effects don’t always show up right away but are often long-lasting.
How to Protect Your Kidneys
If you’re managing chronic pain, blood pressure, reflux, or inflammation with multiple medications, your kidneys are bearing the brunt, not because they’re weak, but because they’re forced to filter and excrete drug residues day after day. What starts as temporary relief quietly becomes permanent dependence, especially when no one revisits the original reason the drug was prescribed.
Breaking that cycle doesn’t begin with another pill. It starts by restoring your body’s own ability to function. Here’s how to take the pressure off your kidneys and reclaim control over your health:
1. Revisit the original reason for each drug — Was it for a short-term issue like post-surgery pain or an infection? Many people stay on medications for years simply because no one rechecked whether they still need them. If the root cause has resolved, the drug is likely doing more harm than good.
2. Watch for warning signs your kidneys are under strain — Fatigue, fluid retention, back pain, changes in urination, or brain fog all point to sluggish kidney function, especially if you’re on multiple medications. These symptoms are often dismissed as “just aging,” but they’re often your body’s early alert system. Don’t ignore them.
3. Support the systems that make medication unnecessary — Chronic symptoms like fatigue, bloating, reflux, or joint pain are often signs of deeper imbalances. Focus on restoring your body’s energy production, improving mitochondrial health, eating nutrient-dense carbs and avoiding vegetable oils that disrupt metabolism. As health improves, medications become easier to taper.
4. Switch out harmful drugs for safer strategies — NSAIDs damage kidney tissues over time but topical magnesium, turmeric, or gentle exercise offer relief without the risk. Acid blockers reduce stomach acid, but the real cause of reflux, for most people, is low stomach acid, not too much of it; switching to digestive bitters before meals to signal your body to start acid production could ease symptoms without long-term harm.
5. Make a medication review part of your routine — Set a calendar reminder every six months to review your medications with your doctor. Ask one powerful question: “Is this fixing the problem — or just covering up symptoms?” That single shift in thinking could help protect your kidneys for years to come.
When your treatment plan aligns with your biology — instead of working against it — most medications become optional, not mandatory. That’s the path to true healing and long-term kidney protection.
FAQs About Medications That Harm Your Kidneys
Q: Which types of medications are most likely to harm my kidneys over time?
A: Common culprits include NSAIDs (like ibuprofen and naproxen), antibiotics (such as tobramycin and sulfonamides), acid blockers (especially PPIs like omeprazole), certain antivirals, and immunosuppressants (like tenofovir and cyclosporine), laxatives and imaging contrast dyes. These drugs reduce kidney blood flow, cause inflammation, or block urine filtration, often without obvious symptoms at first.
Q: Why don’t most people realize their kidneys are being damaged by medications?
A: Kidney damage typically develops slowly and symptoms often appear late. Early signs, like fatigue, swelling, changes in urination or brain fog, are frequently mistaken for aging or other conditions. Without routine lab tests, many people remain unaware until permanent damage is done.
Q: How do NSAIDs and acid blockers affect kidney function?
A: NSAIDs reduce a hormone that keeps kidney blood vessels open, leading to restricted flow and lower filtration, especially during illness or dehydration. PPIs cause an inflammatory reaction in kidney tissues known as interstitial nephritis and are also linked to chronic kidney disease with long-term use.
Q: Does using laxatives or undergoing medical scans also affect kidney health?
A: Yes. Overuse of laxatives cause dehydration and kidney stone formation, while contrast dyes used in CT and MRI scans reduce kidney function, particularly in people with preexisting conditions or poor hydration. Both scenarios increase your risk of long-term kidney damage if not managed carefully.
Q: How do I protect my kidneys if I use these medications?
A: Start by reviewing each drug’s original purpose to see if it’s still necessary. Also watch for signs of kidney stress while supporting your body’s natural healing systems through diet and lifestyle. Taper off unnecessary medications and explore safer nondrug alternatives. Set a six-month reminder to review all prescriptions regularly.
Unlocking DMSO — The Forgotten Molecule That Makes Drugs Work Better, Safer, and Faster
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/07/04/unlocking-dmso.aspx
Analysis by A Midwestern Doctor July 04, 2025

Story at-a-glance
- DMSO is an “umbrella remedy” capable of treating a wide range of challenging ailments due to its combination of therapeutic properties (e.g., reducing inflammation, improving circulation, and reviving dying cells)
- One of DMSO’s unique properties is its ability to enter through the skin and carry anything it dissolves with it as it rapidly travels throughout the body, greatly enhancing the potency and viability of many pharmaceutical drugs
- Because of this, numerous preparations over the years have combined DMSO with a commonly used medication, and in many cases, demonstrated safety and efficacy of the combination to drug regulators
- Some of these DMSO combination therapies are able to treat challenging illnesses, such as significant musculoskeletal injuries, antibiotic resistant infections, persistent fungal and viral infections, chemotherapy resistant cancers, and chronic pain
- More creative DMSO combinations (which can be produced at home) have been frequently used to successfully treat many challenging conditions (e.g., tinnitus, a wide range of eye issues, cancers, and uncomfortable scars)
DMSO is a remarkable naturally occurring substance that (provided it’s used correctly1) safely and rapidly improves a variety of conditions medicine struggles with — particularly chronic pain. For example, thousands of studies show DMSO treats a wide range of:
• Injuries such as sprains, concussions, burns, surgical incisions, and spinal cord injuries (discussed here).
• Strokes, paralysis, many neurological disorders (e.g., Down syndrome and dementia), and numerous circulatory disorders (e.g., Raynaud’s, varicose veins, or hemorrhoids), which were discussed here.
• Chronic pain (e.g., from a bad disc, bursitis, arthritis, or complex regional pain syndrome), which was discussed here.
• Many autoimmune, protein, and contractile disorders, such as scleroderma, amyloidosis, and interstitial cystitis (discussed here).
• Head conditions, such as tinnitus, vision loss, dental problems, and sinusitis (discussed here).
• Internal organ diseases such as pancreatitis, infertility, liver cirrhosis, and endometriosis (discussed here).
• A wide range of skin conditions, such as burns, varicose veins, acne, hair loss, ulcers, skin cancer, and many autoimmune dermatologic diseases (discussed here).
• Many challenging infections, such as shingles, herpes, chronic ear or dental infections, and osteomyelitis (discussed here).
• Cancers and many complications from the illness and its treatments (discussed here).
In turn, since I started this series, it struck a chord, and I have received over 2,000 reports of remarkable responses to DMSO, and many readers have had for a variety of “incurable conditions.”
This begs an obvious question — if a substance capable of doing all of that exists, why does almost no one know about it? Simply put, like many other promising therapies, it fell victim to a pernicious campaign by the FDA, which kept it away from America despite decades of scientific research, congressional protest, and thousands of people pleading for the FDA to reconsider its actions. Consider for example, this 60 minutes program about DMSO that aired on March 23, 1980:
Understanding DMSO’s Combination Potential
DMSO’s effectiveness in treating a wide range of illnesses stems from its unique and diverse properties, many of which appear to target the root causes of disease — such as enhancing parasympathetic activity, improving circulation, regenerating senescent cells, providing potent anti-inflammatory effects, and blocking pain conduction. Sadly, despite hundreds of studies demonstrating these promising characteristics, the FDA has refused to recognize all but one property of DMSO.
In pharmacology, DMSO is often referred to as a “vehicle” that helps other drugs get into the body. Because of this, while DMSO only has one approved (intravesical) use in the United States, a variety of drugs are on the market that use DMSO as a “vehicle” to transport them in the body.
In short, when DMSO is given alone, it is “unsafe” and “unproven” but when combined with a patentable drug, it suddenly becomes “safe and effective.” Likewise, in package inserts, DMSO is typically described as a safe and inert ingredient (despite it often being the primary “active ingredient”).
DMSO’s ability to serve as a drug delivery system is due to its being a potent solvent with a variety of unique properties.
• Membrane permeability — DMSO will pass through biological membranes without damaging them, which is extremely unusual.2 This property is believed to be due to its exchange and interchange with water in biological membranes.3 In addition to not harming the skin, when tested with other substances that could enter the brain, DMSO was not observed to alter the cells lining the blood-brain barrier or the brain tissue.4
• Rapid distribution — Once it contacts the skin, DMSO rapidly spreads throughout the body. Within an hour of being applied to the skin, it can be found within the bones and teeth.5 Interestingly, DMSO does not penetrate tooth enamel or nails, which may explain why certain conditions affecting these structures require different approaches.6
• Solvent properties — DMSO is a highly potent solvent that can dissolve a wide range of polar and non-polar substances (and hence is sometimes used to solubilize other drug products). If a substance is dissolved within DMSO, DMSO can typically bring it into the body. While a few other substances can also serve as vehicles, DMSO is the most potent in pharmacology (e.g., DMSO is more effective than propylene glycol at delivering topical steroids into the body7).
• Enhanced circulation and cellular transport — Beyond simply transporting substances into the body, DMSO also greatly increases circulation. By taking the place of water (as it is small, can form hydrogen bonds, and is relatively polar) while being both fat and water soluble, it changes the permeability of the cell membrane, allowing new things to enter the cell and waste products to leave the cells.
As a result, DMSO is able to both spread what it transports throughout the body and significantly enhance the body’s innate ability to circulate what has already been absorbed (including to previously inaccessible areas).
This combination of properties enables the topical administration of drugs that would normally require injection, and in many cases, can significantly increase their potency because it penetrates deep regions of the body that pharmaceuticals typically have difficulty entering, or because it bypasses the cellular barriers that normally exclude foreign substances.
In turn, lower doses of drugs can frequently be used (reducing their toxicity) because they become more potent, and because DMSO combinations can be locally applied to bring a drug to a target region, rather than taking a standard oral dose that raises the entire body’s target concentration.
• Specialized DMSO pharmaceuticals — These properties allow well established drugs to be combined with DMSO. For example, NSAIDs (which are also used to treat pain and musculoskeletal injuries) have a variety of side effects when consumed orally (e.g., fatal NSAIDs gastric bleeds killed over 16,000 Americans in 19998). However, when combined with DMSO, NSAIDs can be applied topically to the site of injury, thereby avoiding the risks of oral NSAID consumption.
One FDA-approved drug (Pennsaid) does just that, and in clinical trials, it was found to have minimal systemic toxicity. DMSO significantly enhances the efficacy of diclofenac (Pennsaid’s NSAID) while exhibiting much lower toxicity compared to oral diclofenac.9,10,11,12
Many other FDA approved pharmaceutical products utilizing DMSO further demonstrate its therapeutic versatility:
◦Mekinist, a targeted cancer therapy, uses DMSO to stabilize the drug and enhance its water solubility, possibly increasing tumor penetration.13
◦Prochymal, a stem cell product for preventing tissue rejection, uses 10% DMSO to preserve stem cells, as do many other stem cell products.14
◦Onyx, a liquid injected into blood vessels to seal leaks, uses DMSO to dissolve the polymer so it remains liquid until reaching problem areas. DMSO is chosen because it’s a uniquely safe substance capable of this function.15
◦Viadur is a non-degradable implant for prostate cancer containing Lupron dissolved in DMSO, designed to slowly release Lupron over a year.16 DMSO is essential because Lupron is otherwise difficult to dissolve, and DMSO preserves its stability while being nontoxic.
Note: Lupron is an incredibly toxic hormone eliminating drug used for prostate cancer which was adopted by urologists due to it being incredibly lucrative (which then led to it being repurposed for many other areas of medicine such as gynecology and blocking puberty in transgender children).
Critical Considerations
DMSO’s function as a vehicle and potentiator has enabled a variety of innovations for common medical therapies (e.g., pain-killers, antibiotics, and chemotherapy), which has inspired many others to experiment with these combinations. However, for anyone planning to do this, it is critical to understand the safety precautions that must accompany using DMSO in this manner.
• Contamination risk — One of the major risks of DMSO is its potential to exacerbate the effects of a toxic substance already present in the skin, so it is crucial to clean the skin thoroughly before applying DMSO. The original investigator of DMSO learned this lesson the hard way when researching toxic pesticides.17
[Herschler] wanted to investigate whether certain highly toxic pesticides were soluble in DMSO. The researcher felt how soluble they were when he sprayed some of the solution onto his skin. DMSO transported the poison into the body within minutes. The poison worked: Herschler temporarily suffered from impaired consciousness and shortness of breath.
Remarkably, despite the immense potential harm, serious incidents are extremely rare, suggesting either that users are consistently careful about cleaning skin prior to DMSO applications or that the actual risk is limited to highly toxic substances.
• Potentiation effects — Many agents become significantly more potent when mixed with DMSO, and in a few reports made rare side effects typically seen at higher doses manifest (something which has occasionally been reported with the more toxic antibiotics like fluoroquinolones or certain chemotherapy drugs).
With natural substances, this is generally not problematic (as their potency and toxicity are typically much less than pharmaceuticals). Still, it remains a real consideration (although I have not come across any reports of this injuring someone).
• Size limitations — While DMSO can draw things inside the body, it can only do so for smaller molecules, with the size limit thought to be around 500 daltons (although there are numerous examples of larger drugs also being transported).
For this reason, DMSO tends to work well as a vehicle for individual drugs or chemicals but not larger proteins (e.g., peptides). Likewise, pathogenic organisms are far too big for DMSO to transport, so areas of application do not need to be disinfected prior to application.
Note: Below the skin, the transportation limit is much higher (e.g., evidence suggests DMSO can bring molecules larger than 70,000 Da through the blood-brain barrier, opening even wider possibilities for intravenous applications).18
• Purity requirements — When making DMSO combinations, it’s essential to obtain pure ingredients, as many pharmaceutical and supplement preparations contain multiple ingredients beyond the primary active compound
Note: One of DMSO’s most promising combinations is with a common dye (hematoxylin) as this combination selectively targets tumors with no toxicity to normal tissue and has remarkable efficacy against a wide range of cancers. Unfortunately, hematoxylin is often mixed with heavy metals (to better stain tissues), illustrating the need to ensure pure substances with DMSO.
• Leaching — As a solvent, DMSO can leach toxic chemicals (e.g., those added to the surfaces of plastics) and hence later bring them into the body. For this reason, it is advisable to avoid storing DMSO in plastic that is not DMSO resistant and to avoid mixing or preparing DMSO with plastic tools.
In most cases, DMSO only leaches plastic at concentrations about 20%, so if DMSO is diluted before putting it in contact with plastic many of these issues can be avoided. Likewise, many DMSO compatible materials exist for preparing DMSO combinations — all of which is discussed further here.
Note: Most implanted medical devices are not at risk of DMSO leaching them as it dilutes far below 20% by the time it reaches them and can contact their plastic components. The one exception are within dental implants, and for that reason, DMSO mouthwashes must always be sufficiently diluted.

Save This Article for Later – Get the PDF Now
DMSO Drug Interactions
Given DMSO’s ability to potentiate pharmaceuticals, a critical question arises: is it safe to take alongside other drugs? The answer is nuanced:
• What we know — Most pharmaceutical interactions, unfortunately, have not been studied. Fortunately (particularly since over 61% of Americans are on at least one medication19), significant reactions are rarely reported.
Generally speaking, the risk for potentiation is stronger the closer they are taken together (particularly when mixed together in an IV infusion) so it is generally advised to space DMSO and a pharmaceutical by at least two hours, and in the case of more toxic ones (e.g., fluoroquinolones and certain chemotherapies) by at least two days.
Note: DMSO can also mitigate many pharmaceutical toxicities, such as gentamicin’s kidney toxicity20 or many injuries caused by chemotherapy.
Most of the research into DMSO’s interactions was conducted during the initial trials in the 1960s, where it was discovered DMSO significantly potentiated alcohol and also potentiated barbiturates, corticosteroids, insulin, digitalis, nitroglycerin, quinidine sulfate, and chemotherapy21 (leading to lower doses sometimes being needed).
Since then, DMSO has also been observed to potentiate certain opioids (e.g., morphine patches), NSAIDs, anticonvulsants (e.g., gabapentin), and certain sedatives (e.g., trazodone). Users typically do not report potentiation of anticoagulants; however, as a serious risk might exist, it is advisable to monitor your coagulation parameters when using both concurrently.
Note: Insulin potentiation is hypothesized to result from DMSO’s protein refolding capacity restoring the functionality of insulin receptors.22
Conversely, DMSO has also been observed to reverse the effects of Botox, likely by neutralizing the toxin induced paralysis.
Therapeutic Synergies
Over the years, many remarkable pharmaceutical DMSO combinations have been developed for a wide range of medical applications. These include:
• Antibiotics — Antibiotic resistance is a major problem in medicine. However, when combined with DMSO, many organisms that are chronic and debilitating or life threatening (e.g., tuberculosis) lose their resistance to antibiotics.
DMSO also makes it possible to reach infections such as those within the bones that are normally difficult to reach and otherwise require maintaining very high blood concentrations of the drugs to ensure this result. Finally, in many cases (both for cost and to protect the gut microbiome) being able to topically apply an oral or IV antibiotic can be immensely advantageous (e.g., for mastitis or Lyme disease).
• Antifungals — Fungal infections are often located in areas that topical and oral antibiotics have difficulty penetrating. However, research shows combining an antifungal with topical DMSO can reach those infections and there are many reports of multiyear fungal infections quickly resolving from this combination.
• Herpes and shingles — Some of the most potent antiviral medications have difficulty penetrating through a lesion to where the virus resides. However, once combined with DMSO they do, and many clinical trials have proven the efficacy of these antiviral combinations.
• Corticosteroids — For issues within the body, steroids (which have significant systemic toxicity) must be injected or taken orally. When combined with DMSO, this is often no longer needed, and as DMSO potentiates steroids, much lower and far less toxic doses can be taken to address an autoimmune or musculoskeletal issue.
• Chemotherapy — By potentiating chemotherapy, DMSO has been proven to cure chemotherapy resistant cancers, and in many cases does so with much lower doses being needed.
Recently, owing to the emerging popularity of using ivermectin for treating cancer (which sometimes produces spectacular results but typically fits best as a complementary therapy), physicians have begun combining ivermectin with DMSO into a paste and topically applying it over tumors. While data is limited, this appears to consistently work, and sometimes produces dramatic responses like this one James Miller MD recently shared with me:
“I had a patient with a thoracic sarcoma that was debilitatingly painful with growth through a couple of ribs and metastases to his skull base that became basically pain free after 2 days of topical DMSO-ivermectin. At his 2.5 week follow up, he was completely pain free and had returned to playing racketball.”
Note: Nothing comparable to do this can be done with conventional cancer options (and given the severity of that situation, what would be used is also fairly toxic).
Conclusion
As so many things can be combined with DMSO, the incredible things we’ve seen so far are only the tip of the iceberg, and only the most preliminary (but highly encouraging) data exists on many of them, as there is so much to research. For example, DMSO combinations have been shown to effectively treat a wide range of eye issues (e.g., eye strain, macular degeneration, glaucoma, and cataracts), traumatic injuries (e.g., whiplash) tinnitus, uncomfortable scars, neuropathic pain and Lyme disease.
Likewise, DMSO combination therapies are not restricted to pharmaceuticals, and as such, over the years, the DMSO community has discovered hundreds of incredible natural DMSO combinations that revolutionize natural medicine.
Stanley Jacob, the father of DMSO who devoted his career to advancing the science of it, was driven by the recognition DMSO was not a new drug, but rather, like penicillin, a new therapeutic principle which redefined how medicine could be practiced. Fortunately, due to an extraordinary confluence of circumstances, we have now arrived in an era where it is at last (after more than a century) no longer possible to suppress natural healing methods.
People around the world are at last awakening to the Forgotten Sides of Medicine and the realization that the ways to find the cures we need is not “more research” but rather rediscovering what was already found (but not possible to profit off of). This is an incredibly exciting time and I am immensely grateful to be part of it with you.
Author’s Note: This is an abridged version of a longer article about DMSO combination therapies which goes into greater detail on the points mentioned here, many of the other combinations not covered (e.g., for tinnitus or vision loss), and provides guidance for preparing the combination therapies. That article, along with resources and protocols for obtaining and using DMSO can be read here.
A Note from Dr. Mercola About the Author
A Midwestern Doctor (AMD) is a board-certified physician from the Midwest and a longtime reader of Mercola.com. I appreciate AMD’s exceptional insight on a wide range of topics and am grateful to share it. I also respect AMD’s desire to remain anonymous since AMD is still on the front lines treating patients. To find more of AMD’s work, be sure to check out The Forgotten Side of Medicine on Substack.
- 1, 17 A Midwestern Doctor, June 21, 2025
- 2, 6 Annals of the New York Academy of Sciences, 243: 7-19
- 3 International Journal of Molecular Veterinary Research, 2013, Vol. 3, No. 6 (Archived)
- 4 Science. 1982 Jul 9;217(4555):164-6
- 5 Annals of the New York Academy of Sciences, 141: 85-95
- 7 Annals of the New York Academy of Sciences, 141: 428-436
- 8 Cleveland Clinic Journal of Medicine Volume 66, Number 9, October 1999
- 9 JAMA Internal Medicine | Vol. 164, No. 18
- 10 Current Medical Research and Opinion, 32(2), 241–250
- 11 Pain. 2009 Jun;143(3):238-245
- 12 The Journal of Rheumatology 2006; 33:3
- 13 Wikipedia, Trametinib
- 14 Wikipedia, Prochymal
- 15 Medtronic, OnyxTM Liquid Embolic System
- 16 Urology. 2003 Dec 22;62(6 Suppl 1):36-42
- 18 Science, 9 Jul 1982, Vol. 217, Issue 4555, pp. 164-166
- 19 kff.org, October 04, 2024
- 20 Universidad Dr. José Matías Delgado, 2012 (Archived)
- 21 Annals of the New York Academy of Sciences, 141: 532-550
- 22 A Midwestern Doctor, September 15, 2024
Appendix cancer explodes 400% in Gen X and millennials, doctors can’t explain why
Reproduced from original article:
https://www.naturalhealth365.com/appendix-cancer-explodes-400-in-gen-x-and-millennials-doctors-cant-explain-why.html
by: July 3, 2025 (NaturalHealth365)
(NaturalHealth365)
A devastating new study has uncovered a cancer crisis that’s quietly ravaging younger generations while leaving medical experts scrambling for answers. Appendix cancer rates have exploded by 400% among millennials and Gen X, representing one of the most dramatic cancer increases ever documented
The research, published in the Annals of Internal Medicine, analyzed data from nearly 5,000 appendix cancer patients over 45 years and revealed a pattern that should alarm every young adult in America. People born between 1976-1984 showed cancer rates more than three times higher than those born in the 1940s. Those born between 1981-1989 had four times the cancer risk.
Cancer rates skyrocket while doctors stay silent
Dr. Andreana Holowatyj from Vanderbilt University Medical Center put it bluntly: “The rates and trends which we observed were alarming and worrisome.”
Appendix cancer remains relatively rare, affecting only 1-2 people per million annually. But the explosive increase among younger generations signals something deeply wrong. Unlike other cancers with screening protocols, there’s no way to detect appendix cancer until it’s often too late.
Most people discover they have appendix cancer by accident, usually during emergency appendix removal surgery. By then, it’s frequently spread throughout the abdomen.
Symptoms that fool everyone
Appendix cancer symptoms masquerade as everyday digestive problems:
- Abdominal pain that feels like appendicitis
- Bloating that won’t go away
- Nausea and vomiting
- General stomach discomfort
These vague symptoms are often dismissed as stress or poor diet. Most cases aren’t found until the appendix ruptures, spreading cancer cells everywhere. Half of all patients are diagnosed after the cancer has already spread.
The appendix was once considered useless. Scientists now know it plays a role in immune function, making this cancer surge even more troubling.
Nobody knows what’s causing this
What’s driving this cancer explosion? Researchers suspect environmental exposures during childhood are now showing up as cancer decades later.
Dr. Andrea Cercek from Memorial Sloan Kettering admits: “It’s probably some type of combination, something multifactorial, but we have not yet identified it.”
The prime suspects include:
Ultra-processed foods that became standard in Gen X and millennial diets during childhood. These foods potentially altered gut bacteria in ways that increase cancer risk years later.
Chemical exposure from pesticides, plastics, and industrial pollutants that have built up over decades. Younger generations faced higher chemical loads than any previous generation.
Chronic stress from economic instability, social media pressure, and lifestyle factors that suppress immune systems meant to catch cancer early.
Antibiotic overuse during childhood can permanently damage gut bacteria communities responsible for immune function.
This cancer surge isn’t happening alone
Dr. Holowatyj noted similar patterns across multiple cancer types: “We’re seeing some of these generational effects for cancers of the colon, the rectum, the stomach.”
Something is affecting entire generations, not just appendix cancer. Multiple digestive cancers are spiking in younger adults, suggesting a common cause that’s damaging the entire gastrointestinal system.
Whatever is driving appendix cancer rates higher is also compromising the body’s ability to prevent other cancers. This points to fundamental changes in our environment, food supply, or lifestyle that previous generations never experienced.
Fighting back when Western medicine has no answers
Younger adults can’t wait for researchers to figure this out. The cancer prevention strategies that worked for previous generations may not cut it anymore.
Your body has natural cancer surveillance systems, but they need support in today’s toxic environment.
Reduce inflammation through a balanced diet of real, organic food, effective stress management, and avoidance of toxic exposures. Chronic inflammation facilitates the growth and spread of cancer.
Support detox pathways so your body can eliminate the chemicals that may be fueling this cancer epidemic. Your liver, kidneys, and gut require extra support in handling the modern toxic loads.
Strengthen immune function through proper nutrition, sleep, and lifestyle choices. Your immune system is designed to find and kill cancer cells before they become problems.
Avoid processed foods that may be contributing to the generational cancer surge. Fresh, whole, organic foods don’t carry the same risks as heavily processed products.
The clock is ticking
The 400% increase in appendix cancer among younger generations is proof that something fundamental has changed in our world that’s making cancer more common than ever.
Since there’s no screening for appendix cancer, prevention becomes your only protection against this silent killer.
If you are ready to learn how to protect yourself from the environmental factors driving cancer rates through the roof, consider Jonathan Landsman’s Stop Cancer Docu-Class, featuring 22 leading cancer experts sharing breakthrough strategies for cancer prevention and immune system support. Discover which foods, nutrients, and lifestyle changes can help your body detect and eliminate cancer cells before they become life-threatening. Learn about the environmental toxins to avoid, early warning signs to watch for, and proven protocols for reducing cancer risk.
Sources for this article include:
E. Coli Toxin Sparks Cancer Concerns Worldwide
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2025/01/10/colibactin-colorectal-cancer.aspx
Analysis by Dr. Joseph Mercola January 10, 2025

STORY AT-A-GLANCE
- Colibactin-producing E. coli bacteria are linked to increased risks of colorectal and urinary tract cancers due to their ability to induce DNA damage, leading to tumorigenesis
- Geographical variations in cancer incidence are associated with colibactin exposure, with higher prevalence in high-Human Development Index countries, correlating with increased cancer rates in these regions
- Autophagy, the body’s natural recycling process, plays a role in inhibiting colibactin-induced carcinogenesis by repairing DNA damage and removing harmful substances
- Genetic diversity of colibactin-producing E. coli is observed across different populations, with the B2 phylogroup being more prevalent among cancer-associated strains, indicating higher pathogenicity
- Understanding the role of colibactin-producing E. coli in cancer development opens new avenues for prevention and intervention strategies, such as lifestyle modifications to improve gut health
Colorectal cancer, characterized by the uncontrolled growth of cells in the colon or rectum, presents symptoms such as persistent abdominal discomfort, changes in bowel habits and unexplained weight loss. Urinary tract cancer, including bladder and prostate cancer, manifests through painful urination, blood in urine and frequent urges to urinate. These cancers pose significant health challenges, often leading to severe complications if left untreated.
Research published in The Lancet Microbe1 uncovered a link between certain strains of Escherichia coli bacteria that produce a toxin called colibactin and the increased risk of developing colorectal and urinary tract cancers.
Colibactin induces double-strand breaks in the DNA of human cells, driving tumorigenesis and contributing to the formation of cancerous growths. This discovery sheds light on how bacterial infections play a more substantial role in cancer development than previously understood.
Colibactin-Producing E. Coli Linked to Increased Cancer Risk
The Lancet Microbe study investigated the connection between colibactin-producing E. coli and the incidence of colorectal, bladder and prostate cancers. The research sought to determine how geographical variations in the prevalence of these bacteria correlate with cancer rates, particularly focusing on regions with high Human Development Index (HDI).
The study examined different populations across various countries, assessing the presence of colibactin-producing E. coli and the corresponding rates of colorectal and urinary tract cancers. It revealed that areas with a higher prevalence of these bacteria also experienced increased incidences of these cancers. This strong association suggests that the bacteria play a significant role in cancer development.
One of the key findings is that colibactin causes double-strand breaks in the DNA of epithelial cells. This damage is a key factor in tumorigenesis, the process by which normal cells transform into cancer cells. The study highlighted that colibactin-driven DNA damage is a plausible mechanism linking these bacteria to cancer.
Additionally, the research found that certain phylogroup B2 E. coli strains secrete colibactin during interbacterial competition. This secretion not only helps the bacteria survive but also increases the host’s risk of DNA damage. Such interactions within the gut microbiome create an environment conducive to cancer development.
The prevalence of colibactin-producing E. coli varies significantly across different regions, aligning closely with the variation in colorectal cancer rates. In high-HDI countries, the major lineages of these bacteria are frequently associated with urinary tract infections and are more commonly found within the population.
Moreover, the study noted that the incidence of early-onset colorectal cancer has risen significantly in high-HDI countries since the mid-1980s. This trend correlates with the increased prevalence of colibactin-producing E. coli, suggesting that environmental and lifestyle factors in these regions contribute to the spread and impact of these bacteria.
The research highlighted that other members of the Enterobacteriaceae family, particularly the Klebsiella genus, also possess genes for colibactin production. These bacteria frequently colonize the human gut and are common culprits in urinary tract infections. The presence of these genes in multiple bacterial species suggests a broader impact on public health, as it increases the number of sources of colibactin exposure.
The study concluded that eradication of the major pks+ E. coli lineages could offer considerable public health benefits. Reducing the burden of E. coli infections, decreasing the need for antibiotics and lowering the risk of developing cancers linked to colibactin exposure are significant outcomes of such efforts.2
Autophagy Is the Body’s Defense Against E. Coli-Induced Cancer
Another study found that the body’s natural recycling system, known as autophagy, plays a role in protecting against cancer caused by harmful E. coli bacteria. Autophagy is like the cell’s own cleaning crew, removing damaged parts and keeping everything running smoothly. In this research, scientists explored how autophagy helps prevent the development of cancer in the presence of colibactin-producing E. coli (CoPEC).3
The study focused on mice that were either normal or had a specific genetic modification that impaired their autophagy process in intestinal cells. By introducing CoPEC to these mice and inducing chronic inflammation, the researchers aimed to see how autophagy affects cancer formation.
The findings were striking: mice with impaired autophagy developed more invasive cancers compared to those with functioning autophagy systems. This shows that autophagy is essential in fighting off the cancer-promoting effects of CoPEC.
One of the key discoveries was that CoPEC infection leads to significant DNA damage in the cells lining the colon. DNA damage is like having cracks in the blueprint of a building; it leads to structural failures, or in this case, to cells turning cancerous.
The researchers observed that in mice with deficient autophagy, the extent of DNA damage was much greater. This suggests that autophagy helps to repair or remove damaged DNA, preventing the cells from becoming cancerous.4
Moreover, the study highlighted that autophagy not only repairs DNA but also controls the amount of harmful substances within the cells. When autophagy is functioning properly, it clears out toxins and damaged components that could otherwise contribute to cancer development. In the absence of efficient autophagy, these harmful elements accumulate, creating an environment where cancer thrives.5
The researchers also discovered that chronic inflammation, which is a long-term, persistent irritation of the body’s tissues, exacerbates the cancer-promoting effects of CoPEC. Inflammation is the body’s response to harmful stimuli, but when it becomes chronic, it causes more harm than good. The study showed that in mice with chronic inflammation, the presence of CoPEC led to a higher incidence of invasive tumors.
However, when autophagy was active, it mitigated some of the damage caused by both inflammation and bacterial infection, reducing the overall risk of cancer.6 The findings suggest that enhancing autophagy could be a strategy for reducing cancer risk in environments where harmful bacteria are prevalent.7
When comparing the effects of different variables, the study found that the presence of colibactin was a critical factor in cancer development. Mice infected with CoPEC that produced colibactin showed a much higher rate of cancer than those infected with bacteria that could not produce this toxin. This indicates that colibactin is a potent agent in causing DNA damage and promoting cancer.
Additionally, the interaction between colibactin and the body’s autophagy system illustrates how important cellular processes are in defending against external threats.8 Overall, this study underscores the role of autophagy in preventing cancer.
By understanding how autophagy interacts with harmful bacteria like CoPEC, researchers can develop better strategies to enhance this natural defense mechanism. This could lead to new treatments that boost autophagy in high-risk populations, ultimately reducing the incidence of colorectal cancer linked to bacterial infections and chronic inflammation.

Save This Article for Later – Get the PDF Now
Genetic Diversity of Colibactin-Producing E. Coli
A study published in PLOS One explored the genetic diversity of harmful E. coli bacteria that produce colibactin within different populations in Pakistan.9 The researchers aimed to understand how these bacteria differ genetically and how these differences influence their ability to cause cancer.
By analyzing samples from both colorectal cancer patients and healthy individuals, the study provided valuable insights into the relationship between specific E. coli strains and cancer development.
The study focused on individuals from Pakistan, specifically those visiting the Pakistan Institute of Medical Sciences (PIMS) in Islamabad. By comparing the E. coli strains, the researchers identified significant differences in the types and characteristics of the bacteria.
One of the key findings was that a substantial portion of the E. coli isolates from cancer patients belonged to the B2 phylogroup. Phylogroups are classifications that group bacteria based on their genetic characteristics. The B2 group, in particular, was found to be more pathogenic, meaning it has a greater ability to cause disease, compared to other phylogroups. This higher pathogenicity makes the B2 group a significant concern in the context of cancer development.
The study revealed that 43.47% of the cancer-associated E. coli isolates were from the B2 phylogroup, whereas none of the isolates from healthy controls belonged to this group. This stark difference highlights the role of B2 phylogroup E. coli in promoting cancer. The absence of B2 phylogroup strains in healthy individuals suggests that these bacteria specifically contribute to the progression of colorectal cancer.
In addition to the prevalence of the B2 phylogroup, the researchers found that a remarkable 90% of the cancer-associated E. coli strains tested positive for colibactin and the polyketide synthase (pks) island. The pks island is a cluster of genes responsible for producing colibactin. None of the healthy control isolates tested positive for these colibactin genes, underscoring the strong association between colibactin-producing E. coli and colorectal cancer.
Colibactin Is a Genotoxic Compound
The presence of colibactin in these bacteria is particularly concerning because colibactin is a genotoxic compound. Genotoxic means it damages the genetic information within a cell, leading to mutations and causing the cell to become cancerous. In simpler terms, colibactin acts like a faulty key that disrupts the normal functioning of cells, making them more likely to turn into cancer cells.
Furthermore, the study documented the significant cytotoxic activity of the B2 phylogroup E. coli isolates that produce colibactin. Cytotoxic activity refers to the ability of these bacteria to kill cells or damage them severely. The damage caused by these bacteria disrupts the balance of the gut microbiota, which is essential for maintaining intestinal health.
Interestingly, this research was the first to report the prevalence of different E. coli phylogroups in cancer patients within a Pakistani population from a low socioeconomic background. This finding is important because it highlights how genetic diversity in harmful bacteria varies across different regions and populations.
Understanding this diversity helps in identifying specific bacterial strains that pose the highest risk for cancer, allowing for more targeted prevention and treatment strategies.
Microbial dysbiosis, an imbalance in gut microbiota, is closely linked with various intestinal abnormalities, including inflammatory bowel disease (IBD) and colorectal cancer. The study emphasized that the presence of colibactin-producing E. coli strains disrupts the normal gut environment, leading to dysbiosis.
This imbalance creates conditions that favor the growth of harmful bacteria while inhibiting beneficial ones, thereby increasing the risk of cancer development.
Further, in vitro studies, which are experiments conducted outside of living organisms, have shown that E. coli strains with the pks island promote megalocytosis, a condition where cells and their nuclei become enlarged without undergoing proper cell division.
Additionally, these bacteria induce DNA double-strand breaks and encourage G2 cell cycle arrest, where cells are halted before they divide. These effects collectively contribute to the development and progression of cancer by allowing damaged cells to survive and proliferate uncontrollably.
Overall, the genetic diversity of colibactin-producing E. coli and their strong association with the B2 phylogroup highlight the significant role these bacteria play in colorectal cancer development. This study provides a foundation for further research into the microbial factors involved in cancer and underscores the importance of addressing bacterial diversity in the fight against colorectal cancer.10
Practical Steps to Reduce Colorectal Cancer Risk
With E. coli bacteria linked to cancer development, it’s important to take steps to safeguard your health. Research indicates that specific strains of E. coli, especially those producing colibactin toxins, elevate cancer risk by causing DNA damage. Maintaining a stable microbial balance enhances cellular health for chronic disease prevention. Below are the top approaches to improve your gut health and decrease cancer risk.
1. Eliminate processed foods and seed oils — The contemporary diet is laden with processed foods that contain seed oils rich in linoleic acid (LA), which harms your gut microbiome and encourages the proliferation of harmful bacteria.
LA acts as a mitochondrial toxin, disrupting cellular energy production and hindering your ability to sustain a healthy gut environment. In addition to removing processed foods, avoid nuts and seeds to further lower LA intake. It’s also advisable to minimize eating out, as most restaurants use seed oils in their cooking, sauces and dressings.
Furthermore, reduce your consumption of chicken and pork, which are typically high in LA. Replace processed foods with whole, natural foods and healthy fats such as grass fed butter, tallow and ghee. Aim to keep your total LA intake below 5 grams from all sources, ideally under 2 grams. To monitor your LA consumption, record all your daily meals using an online nutrition tracker.
2. Optimize your carbohydrate consumption — Another key factor is the careful management of your carbohydrate intake. Carbohydrates are essential for supporting mitochondrial function since glucose is the primary fuel for cellular energy production. Adjust your carbohydrate intake to promote a healthy microbiome by consuming 200 to 350 grams of specific carbohydrates each day for most adults.
Individuals with higher activity levels may require more. Introduce carbohydrates gradually to allow your gut time to adapt, thereby minimizing digestive issues and endotoxin levels. Start with white rice and whole fruits to nourish beneficial bacteria before incorporating vegetables, whole grains and starches. Initially avoiding high-fiber diets is important if your gut microbiome is compromised, as excessive fiber elevates endotoxin levels in this case.
If your gut health is significantly impaired, focus on easily digestible carbohydrates like dextrose water for the first week or two. Slowly sip it throughout the day to support gradual healing of your gut.
3. Minimize exposure to environmental toxins — Exposure to synthetic endocrine-disrupting chemicals (EDCs), estrogens and widespread electromagnetic fields (EMFs) further weakens your cells’ ability to produce energy efficiently. This energy shortfall makes it challenging to maintain the oxygen-free gut environment necessary for beneficial bacteria like Akkermansia to thrive.
Additionally, inadequate cellular energy creates a gut environment that favors endotoxin-producing bacteria, which damage mitochondria and perpetuate a cycle of declining health. By reducing excess LA, estrogens (including xenoestrogens found in everyday products like plastics), EDCs and EMFs, you restore cellular energy and move toward optimal health.
4. Limit antibiotic use and consider Akkermansia — Antibiotics severely damage beneficial gut bacteria and significantly increase the risk of colon cancer. Use antibiotics only when absolutely necessary and focus on rebuilding your gut flora with targeted dietary choices, including fermented foods, afterward.
Additionally, avoid conventionally raised meats that often contain antibiotic residues by selecting high-quality, responsibly sourced proteins to support a healthy microbiome.
Akkermansia is vital for a healthy microbiome, but many individuals have little to none. It is important to eliminate all seed oils from your diet for at least six months before starting an Akkermansia supplementation program.
This preparation period allows your body to restore mitochondrial function and create a more supportive environment in your colon for beneficial bacteria. By following these steps, you maximize the benefits of Akkermansia supplementation and support overall gut health.
When selecting Akkermansia supplements, choose those that utilize advanced, timed-release capsules or microencapsulation technology. These methods keep the bacteria dormant and protected until they reach your colon, typically within two to four hours after ingestion, ensuring that a higher number of live bacteria survive the journey through your digestive system.
- 1, 2 The Lancet Microbe December 05, 2024
- 3, 4, 5, 6, 7, 8 Cancers 2021, Volume 13(9), 2060
- 9, 10 PLoS ONE November 11, 2022, Volume 17; 11
How Your Gut Microbiome Affects Your Oxalate Tolerance
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/06/23/oxalate-intolerance-gut-microbiome.aspx
Analysis by Dr. Joseph Mercola June 23, 2024
STORY AT-A-GLANCE
- Oxalates are naturally occurring substances found in many plants, including vegetables and fruit
- While they’re a normal part of human metabolism and your diet, can contribute to the formation of kidney stones and other problems in sensitive individuals
- The problem isn’t the oxalates themselves but a damaged gut, which interferes with your body’s ability to clear oxalates effectively
- In my interview with Ruth Ann Foster, ScD, BSN, RN, we explore the underlying causes of that gut dysfunction and how it relates to overall health
- A diet of ultraprocessed foods and antibiotics are two primary culprits underlying gut dysfunction and oxalate intolerance
Oxalates are naturally occurring substances found in many plants, including vegetables, fruits, nuts and seeds. Chemically, oxalate is the ionized form of oxalic acid, explains Ruth Ann Foster, ScD, BSN, RN.1 While they’re a normal part of human metabolism and your diet, they can bind to minerals like calcium, forming crystals known as calcium oxalate.
When consumed in large amounts or in susceptible individuals, oxalates can contribute to the formation of kidney stones. However, the problem isn’t the oxalates themselves but a damaged gut, which interferes with your body’s ability to clear oxalates effectively.
In my interview with Foster, who has a doctorate in holistic nutrition and studies the relationships between minerals, microbes and water, we explore the underlying causes of that gut dysfunction and how it relates to overall health.
People Have Eaten High-Oxalate Diets for Millenia
“I really got started on oxalates when I was doing my dissertation on magnesium and drinking water. And because magnesium is, you know, vital it inside the cell,” Foster explains. “It’s an antagonist with calcium, which is made mainly outside of the cell. And, you know, the majority of kidney stones are calcium oxalate, and that has coincided with a deficiency in magnesium. So, I was well aware of problems with oxalates.”2
However, she started to wonder why oxalates are such a problem. Initially, she thought plants may be the issue, assuming Eskimos and other native cultures didn’t eat a lot of high-oxalate foods and were therefore healthy, with low rates of kidney stones. But it turned out that high-oxalate foods are common in many traditional diets:3
“I found that there are a lot of ancestral tribes and communities that ate a lot of oxalates and a lot of people that are still living on them today. So, then I started looking more into kidney stone disease and realize yes, while it’s been around since antiquity, it really has taken off exponentially since the Industrial Revolution — since we started eating processed foods.
And, you know, processing our water to take the magnesium out of the drinking water … one of the first groups of people that I looked at … were the people in the lower Pecos … region of I think it’s Western Texas, and they ate a lot of oxalates. But they were able to clear them.
And then looking around at that, looking at animals in the kind of desert area, there’s a wood rat, a white-throated wood rat, that also consumes most of its diet in an oxalate cactus and things like that. But it also excretes them.
So, scientists are now using the woodrat to study our microbiome. And they’ve taken some of the transplanted fecal material from the woodrat into lab rats. And they’ve been able to maintain oxalate clearing tolerance for nine months later. So, there’s something going on in the gut microbiome.”
Foster also researched the Inuits, first assuming that their very low rates of kidney stone disease are due to a diet low in fruits and vegetables, and low in oxalates. Yet, once again, she revealed these native cultures have eaten high-oxalate foods all along, without the problems they cause to so many people today:4
“It turns out … the Inuits eat a lot of high-oxalate foods, and they eat them all year long. They don’t just eat them [during] their short little growing season. They ferment them, they dry them, and so on …
Plus, the other thing that they would do is they eat the rumen of some of the reindeer that they find, which is, again, it’s going to have some bacteria in it. And that helps them to be able to process through these things. So then looking at Africa, same kind of thing, high-oxalate foods. And in each one of these situations, all of these people have been able to clear the oxalates.”
Antibiotics, Ultraprocessed Foods Are Destroying Gut Health
Exposures to antibiotics and ultraprocessed foods represent a key difference in traditional cultures and those living in the modern world. These factors are destroying gut health among those living in the Western world, such that many people are unable to handle high-oxalate foods.
“Overall, accumulating evidence reveals that kidney stones are fundamentally linked to a damaged gut, which impairs the body’s ability to clear oxalates. We must, therefore, consider the real culprits like refined sweeteners, ultraprocessed foods and seed oils — hallmarks of the modern industrial diet,” Foster writes.5
One consequence is that an important bacterium, Oxalobacter formigenes, is now missing in many adults’ guts. “A lot of the primitive cultures still have Oxalobacter in their guts,” Foster says.6 This beneficial bacterium plays a crucial role in the metabolism and regulation of bodily oxalate levels. It digests oxalate crystals and basically signals the gut wall to excrete oxalate for its own nourishment.
In this way, Oxalobacter helps reduce the concentration of oxalate in your gut, which can consequently lower the risk of oxalate crystallization and the formation of kidney stones and other health problems. However, this is just one type of beneficial bacteria involved in oxalate degradation. According to Foster:7
“With rapid advances in technology, scientists have learned that multiple bacterial species can degrade oxalate, working through a large network. For example, monitoring the gut bacteria of over one thousand healthy participants, one study found that the majority (92%) of gut microbiomes contained several species of oxalate-degrading bacteria.
Because of the complexity of the oxalate-degrading network, researchers now understand the importance of assessing gut health in its entirety rather than focusing on a single bacterial type such as O. formigenes … Hence, a healthy gut is key to maintaining oxalate tolerance.”

Save This Article for Later – Get the PDF Now
Healthy Foods Often Get Blamed for Problems Caused by a Damaged Gut
Often, Foster says, when people try to switch from a highly processed diet to a healthy one, they introduce more high-oxalate foods, like spinach and beets. Then, digestive issues, such as bloating, gas and abdominal pain, may occur due to the irritation of the intestinal lining by oxalates.
“You want to correct it and so you start eating healthy, and then you get even sicker … then, instead of blaming the bad foods, you blame the healthy food,” Foster says. In short, as a result of an ultraprocessed diet, mitochondrial dysfunction and an inability to create sufficient cellular energy occurs.
So, many people have lost the ability to maintain a high enough concentration of beneficial bacteria in their gut that actually digest the healthy fibers in fruit, vegetables and grain. Then, when you do eat those types of foods, you get worse, as you’re not feeding the good bacteria anymore, because they’re not there, they can’t survive.
Instead, you have a buildup of pathogenic bacteria that produce toxic endotoxin, one of several factors that destroys mitochondrial function.
Two Major Types of Bacteria — Oxygen Tolerant and Oxygen Intolerant
A healthy gut with a properly maintained anaerobic environment supports the growth of beneficial oxygen intolerant, such as the keystone species Akkermansia. When the oxygen gradient is disturbed due to insufficient energy production (as seen in metabolically inflexible individuals), it allows pathogenic oxygen tolerant bacteria to proliferate.
These bacteria often produce more virulent endotoxins, also known as lipopolysaccharides (LPS), which can cause inflammation if they translocate across the compromised gut barrier into the systemic circulation. Oxalates indirectly contribute to this scenario by exacerbating mitochondrial dysfunction and reducing cellular energy production.
Colonocytes are the epithelial cells lining the surface of your colon, where they make up the majority — about 80% — of the epithelial cell population. Not only do they serve as the barrier, the actual lining of your gut, but they perform beta oxidation and are involved in the metabolism of short chain fatty acids.
In the process of metabolizing short chain fatty acids, colonocytes consume a significant amount of oxygen, reducing the oxygen levels in your colon. The short chain fatty acids that colonocytes need are produced from the fibers that you eat — typically from healthy foods like vegetables, apples and other fruits.
These fibers nourish both good and bad bacteria, however. if you have a preponderance of pathogenic bacteria, it makes it hard to eat healthy, because eating healthy foods makes you feel worse due to the radical increase in endotoxin, which can kill you.
In my view, the No. 1 cause of death, that exceeds heart disease and cancer, is endotoxemia. Healthy, unprocessed foods are historically all our ancient ancestors had — they didn’t have to deal with processed foods. So, they had a healthy gut and were able to consume high-oxalate foods without a problem.
Once your gut is healthy, consuming dietary oxalate helps you maintain tolerance by feeding sustaining oxalate-degrading bacteria, Foster notes. The key is to consume a healthy amount — neither too much nor too little:8
“Maintaining tolerance by daily consuming some dietary oxalate is important. Ironically, when dietary oxalate intake is lower than fifty milligrams per day, oxalate absorption increases significantly. At the same time, overconsuming high amounts of dietary oxalates, especially in the form of foods like spinach smoothies, can be hazardous.”
As mentioned, you have to have cellular energy to consume high-oxalate foods without issue. But if you don’t have it, then you enter a cascading downhill spiral that gets increasingly worse.
Modern Diets Are the Problem
Foster points out that it’s not dietary oxalates that are the issue, but rather modern diets focused on ultraprocessed foods:9
“Considering escalating diabetes rates and poor American dietary habits, it appears that gut dysbiosis and the overconsumption of industrially ultraprocessed foods are more responsible for oxalate toxicity than the overconsumption of so-called ‘superfoods’ like spinach or sweet potatoes.
Simply put, it is not oxalate-containing foods like spinach that are increasing the production and absorption of oxalate. To address the oxalate problem, we must consider the impact of processed and ultraprocessed industrial foods on gut and kidney health.”
This includes seeds oils, high in omega-6 polyunsaturated fatty acids (PUFAs) like linoleic acid. Foster explains:10
“Overconsumption of industrial seed oils, high in omega-6 polyunsaturated fatty acids (PUFAs), contributes to AGE [advanced glycation end product] production … The fatty acid ratio of omega-6 to omega-3 is a driving factor in kidney disease and many other chronic illnesses.
In the past 30 years, dietary omega-6 consumption has increased in the face of omega-3 deficiency. The ideal ratio of omega-6 to omega-3 is about two to one, but today’s ratio is over 20 to one. Researchers have noted that a ‘USDA egg’ has an omega-6 to omega-3 ratio of about 20:1.
Industrial seed oils and other sources of omega-6 weaken and soften the cell membranes, which enhance oxalate binding to the nephrons and begin crystal formation. Accumulating evidence shows a link between increased consumption of omega-6 fatty acids and kidney stone disease.
In contrast, higher intakes of omega-3 fatty acid (mostly from seafood) protect against the risk of kidney stone formation, CKD [chronic kidney disease] and other degenerative diseases, as evidenced by the diet of traditional Inuit populations, rich in omega-3 fatty acids.”
The addition of excessive amounts of omega-6 fat to the diet via ultraprocessed foods is what catalyzed the now epidemic levels of mitochondrial dysfunction. It caused depletion of colonocytes because of the gradual intrusion and increase in oxygen concentration in the colon that causes this cascade of death in your microbiome.
Glucose (Dextrose) May Offer a Short-Term Solution
In my view, the healthiest fuel for your mitochondria is glucose, not fat, as fat increases reductive stress and slows down the electron transport chain. Some cells, like the colonocytes, thrive on beta oxidation, so do our heart cells. Most cells require glucose, but if you’re following a keto or carnivore diet, you’re likely carb deficient.
There’s a lot of consequences from that, but many people get better on carnivore or keto because they stop eating ultraprocessed foods and feeding these patterns.
In the short-term, however, to get out of this destructive cycle, consider taking glucose, which is more commonly called dextrose. It’s pretty inexpensive — about $5 a pound. Glucose never reaches your colon; it’s all absorbed in your small intestine. Because of that, it avoids the complication of providing fuel to the facultative anaerobes, the pathogenic bacteria that can make endotoxin.
Consuming glucose is preferable to not consuming any carbs, which is highly problematic, in part because your cortisol level goes up. Ultimately, if your body is producing high amounts of cortisol to compensate for the lack of healthy carbs in your diet, this is not a state you want to be in for a prolonged period if you want to live a long and healthy life.
So, if you’re unable to tolerate healthy carbs, try pure glucose for a few weeks. This is especially useful for those who are seriously damaged, who don’t have the capacity to eat virtually any carbohydrates. You can go on a high-dextrose diet until your gut starts to heal. You save more cellular energy, which allows you to introduce more carbs back in to your diet, helping to restore your mitochondrial function.
Fraud in the Probiotics Market
Unfortunately, once you’re lacking cellular energy and your gut health is disrupted, most probiotic supplements on the market are useless, as they’re all fatally flawed. No one has yet figured out how to how to take that raw material and put it in a capsule and get it into your gut. It dies in the meantime. There’s a lot of fraud going on in this area, which I’m going to expose shortly.
Further, no one has yet grown Oxalobacter, but I’ve got a research team on it right now to define the protocol. These bugs are very difficult to grow and require many millions of dollars of investment to identify the specific protocol that causes them to thrive and then to harvest them. Once they’re harvested, you still have the technical challenge of putting them into a capsule in a way that doesn’t kill them.
I’m hoping we’ll have Oxalobacter within a year or two. It’s one of our priorities to get that out because it’s just like a seed to encourage good bacterial growth in your gut. But remember, if you put a seed in the Sahara Desert, and there’s no water, the seed can’t grow. It’s the same with Oxalobacter.
Even if you have the best Oxalobacter supplement in the world, if you put it in most everyone’s gut, nothing’s going to happen because the environment isn’t healthy enough to support it. You have to take care of the foundational causes of the issue first, including resolving mitochondrial dysfunction and an inability to create sufficient cellular energy.
Protecting Your Microbiome Is Key
The health of your microbiome begins even before birth, from conception. This crucial window of development sets the stage for your gut health — a topic Foster says she’d like to expand on in book form:11
“The book that I would like to write is … the first 1000 days. And it is from conception to about age 3, when that whole microbiome is developed … we get our gut colonized at birth … we [once] thought that the baby was born sterile. We now know that babies come out with, I think, 100 different species in the colon, ready to go. And it comes from the mother’s … microbiome.”
However, early antibiotic treatments, lack of breastfeeding and other factors often disrupt gut microbiome early on. At any age, however, promoting a healthy gut microbiome by avoiding ultraprocessed foods and consuming probiotic-rich foods like yogurt, kefir and fermented vegetables can support the growth of beneficial bacteria, including those that can degrade oxalates like Oxalobacter.
Drinking sufficient water is also crucial as it helps to flush out oxalates through your urine and prevents kidney stones from forming. Foster explains that not only is the quality of your drinking water important but the mineral content also matters:12
“Higher mineral content is associated with increased urinary citrate, while lower mineral content is not. Mineral water frequently contains bicarbonate, which is absent in tap water. Gerolsteiner, a naturally sparkling mineral water, is a great source of magnesium and high in bicarbonate. As mentioned, magnesium is a natural stone inhibitor, while bicarbonate increases the excretion of citrate, another important inhibitor.
Mineral water provides the most bioavailable forms of magnesium and calcium. Because they are hydrated (ionic), these minerals are rapidly absorbed. Likewise, raw milk is a valuable source of bioavailable magnesium and calcium. Other liquids to increase hydration can include bone broths, soups, tea (depending on oxalate content) and limited amounts of sour kombucha.”
Is Horseradish Nature’s Best Antibiotic?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/25/natural-antibiotic-horseradish.aspx
Analysis by Dr. Joseph Mercola May 25, 2024

STORY AT-A-GLANCE
- Used as a medieval medicine as well as a popular condiment on beef, horseradish has a long list of compounds that can help fight and even lower the risk of disease
- Respiratory ailments, from colds to pneumonia, can be alleviated using horseradish, and research shows it can also help treat urinary tract infections, skin disorders and intestinal parasites
- Horseradish contains powerful isothiocyanates (ITCs) such as glucosinolates broken down from the volatile oil sinigrin, found to help protect against lung, breast, colon and bladder cancers
- You can make your own horseradish preparations to help combat sinus infections, colds and skin disorders, help boost your immune system and potentially lower the risk of headaches, gout, colic and gallbladder problems
A wonderfully zesty condiment to add to prime rib or other cuts of grass fed beef, horseradish has an unmistakable heat that radiates not so much in your mouth as in your nose.
While its exact origin isn’t certain, horseradish probably originated in the Mediterranean region, which alludes to its long, rich history.1 Greek mythology, for instance, considered horseradish to be worth its weight in gold.2
Cooks and healers continued making use of this root veggie in 15th century England, and centuries later the earliest American presidents grew it in their gardens. About 60% to 85% of the world’s horseradish production comes from the U.S., specifically Illinois.3
One rule of culinary thumb recommends that horseradish be red when it’s used for shrimp (typically mixed with a tomato base) and white when it’s made into a sauce to spread on beef. But as is true with many plant-based foods, both in ancient times and now, part of this pungent root’s value has been its medicinal capability.
Clinical evidence has indicated that horseradish has worked just as well or better than chemically concocted medicines. Horseradish has been successful in helping manage diseases, as well. Healthy and Natural World notes:
“Empirical research has now proved what our ancestors intuitively already knew. When treating certain conditions, horseradish is just as effective as chemically-synthesized antibiotics and it can sometimes even be superior to over-the-counter drugs.
Horseradish is particularly potent in the treatment of sinusitis and it clears upper respiratory passages, which helps with cold, influenza and lung congestion … When used as a natural drug, it comes without any side effects. At the same time, it provides us with some distinct culinary enjoyment.”4
However, it’s important to remember that heating horseradish can significantly alter the strength of the many healing compounds it contains, so eating it raw is recommended.
Horseradish Contains Compounds With Health-Enhancing Horsepower
It’s probably no surprise that one of the best uses for horseradish is that it can open up the stuffiest sinuses. This harkens back to one of its most popular uses as a throat-coat for hoarseness. Other conditions it remedies range from colds to urinary tract infections to kidney stones.
According to the Baseline of Health Foundation,5 horseradish may be helpful for relieving symptoms of several serious diseases and disorders, including high blood pressure, cancer and sinus infections. It may also help boost immune system function and fight other infections. Mother Earth News even asserted:
“Ounce for ounce, horseradish contains more medicinally active compounds than most other spices.
And they are very active — they can clear congestion, thin mucous, reduce inflammation, squelch cell-damaging oxidants, fight bacteria and viruses, relax muscles, stimulate the immune system — and even battle cancer. That makes the humble horseradish one special spice.”6
Variations of Healing Compounds in Horseradish
One book on the topic lists several healing compounds, and notes that “Horseradish has been reported to have antimicrobial, spasmolytic, cytotoxic, antiseptic, diuretic, stimulant and antioxidant properties.”7
Subfeed adds that horseradish also “acts as an antiviral, antibacterial, antifungal and antiparasitic medicine.”8 Clinical evidence notes that it’s these compounds that infuse it with health-enhancing potential.9
Oddly, horseradish root doesn’t have much of an odor until it’s nicked, cut or chewed, at which point its intensity becomes immediately evident. The smell indicates the presence of some potent, but completely natural, chemicals that impart such dramatic healing capability.
As a member of the Brassicaceae family along with mustard, wasabi and cabbage, horseradish comes with a storehouse of isothiocyanates (ITCs) such as glucosinolates (found only in Brassica plants) broken down from the volatile oil sinigrin and found to protect against cancer.10
The Ohio State University College of Food, Agricultural and Environmental Sciences11 says laboratory studies released by the American Institute for Cancer Research found that the presence of glucosinolates in food can:
- Decrease inflammation associated with many chronic illnesses, including cancer and cardiovascular disease
- Suppress enzymes known to activate carcinogens
- Stimulate enzymes that deactivate carcinogens and decrease the ability of cancer cells to spread
In a study conducted at the University of Illinois, horseradish was found to deliver 10 times more glucosinolate enzymes than broccoli.12 Lead researcher and associate professor in crop sciences Mosbah Kushad disclosed that just a little “dab” on your steak can communicate benefits and may provide the same health benefits as broccoli.
Sinigrin has a distinguished set of skills, as well. Another study links it with inhibiting lipid peroxidation by 71%, and it plays several roles in reducing the risk of several cancers.13

Save This Article for Later – Get the PDF Now
Horseradish Can Impact Several Types of Cancer
Further, the ITCs in horseradish (as well as wasabi root) were found in clinical trials to help reduce colon and lung cancer cell activity, and the higher the dosage, the weaker the cancer cells became — 30% to 68% weaker for colon cancer and 30% to 71% weaker for lung cancer cells.14
Horseradish contains more than two dozen other cancer-combating compounds. Researchers in England, Austria and New Zealand investigated one they called horseradish peroxidase (HRP), which was targeted as a treatment to help control the growth of breast and bladder cancer cells.15
After ingesting the volatile oil of horseradish, tests on human urine have shown that it can kill the bacteria that cause urinary tract infections. In fact, German herbal remedies suggest it kills gram-positive and gram-negative bacteria and candida and successfully treated many viral, bacterial, parasitic and fungal diseases.
The reduction in symptoms from chronically recurrent urinary tract infections (UTIs) after consumption of an herbal medicinal product containing horseradish has been reported as “statistically significant,” another study said.16
Healing and Immune-Boosting Horseradish Recipes
Used in combination with other healing herbs and plants with medicinal capabilities such as ginger, garlic, turmeric and apple cider vinegar, horseradish preparations have numerous applications. As always, use organic ingredients whenever possible.
One recipe calls for a 6-inch horseradish root peeled and grated into the juice of one lemon and a tablespoon of raw, organic honey and sealed in an airtight jar for 24 hours. One tablespoon, undiluted and taken three to four times a day is a heady concoction to soothe your throat and loosen your sinus congestion.
The Master Tonic recipe, which Subfeed17 says is a basic, all-around tonic dating back to medieval Europe, is used as an antibiotic to purify your blood, kill bacteria and increase blood and lymph circulation throughout your body, can be added to olive oil for use as a salad dressing or applied to wounds and infections.
Master Tonic
Ingredients
- 24 ounces organic apple cider vinegar
- 1/4 cup coarsely chopped garlic
- 1/4 cup chopped onion
- 2 fresh hot peppers, such as habaneros
- 1/4 cup grated fresh ginger
- 2 tablespoons horseradish
- 2 tablespoons turmeric powder (or the equivalent in turmeric root)
Procedure
Process the ingredients in a food processor but note that the apple cider vinegar is added later.
- Process the ingredients, then transfer the mixture to a Mason jar, filling it about two-thirds full.
- Pour in enough apple cider vinegar to fill the jar to the top.
- Close tightly and shake the jar until it’s well-combined. Do this several times a day while storing it in a cool, dry place for up to two weeks.
- After 14 days, strain the liquid through gauze or cheese cloth, squeezing the solid bits and setting them aside for use in recipes. The liquid part is then ready for medicinal use.
This mixture can be gargled and swallowed as a sore throat remedy. Take 1 tablespoon per day to strengthen your immune system and fight colds and flu. Master Tonic is safe for use by children and pregnant women in small doses, but take it with food until you’re used to it.
One thing to keep in mind when you’re handling horseradish, whether in food preparation or to make a tonic to treat health problems, is to wear plastic gloves for the same reason you do when handling some of the hottest peppers, such as jalapenos or habanero peppers. Also, keep it as far from your nose as possible!
- 1 Britannica, “Horseradish”
- 2 Horseradish.org, “Horseradish History”
- 3 St. Louis Magazine, May 17, 2018
- 4 Healthy and Natural World 2017
- 5 Baseline of Health Foundation, July 1, 2017
- 6 Mother Earth News March 31, 2014
- 7 Antioxidant Properties of Spices, Herbs and Other Sources, Horseradish, 01 January 2012, pp 347–351, Abstract
- 8, 17 Subfeed, “This Is The Most Powerful Natural Antibiotic Ever – Kills Any Infections In The Body” (Archived)
- 9 Journal of Agroalimentary Processes and Technologies 2013, 19(1), 111-115, Abstract
- 10 Eur J Nutr. 2008 May;47 Suppl 2:73-88
- 11 OSU January 15, 2016
- 12 Science Daily May 17, 2016
- 13 Nutr Cancer. 2004; 48(2):207-13
- 14 J Agric Food Chem. 2005 March 9;53(5):1440-4
- 15 Cancer Med. 2016 June;5(6):1194-203
- 16 Curr Med Res Opin. 2007 October;23(10):2415-22
Maple syrup may help reduce chronic inflammation and fight superbugs
Reproduced from original article:
https://www.naturalhealth365.com/maple-syrup-inflammation-2310.html
by: May 6, 2024
 (NaturalHealth365) The first global symposium focused on the health benefits of pure maple syrup was held in early April 2017. This symposium was part of the 253rd annual American Chemical Society (ACS) meeting in San Francisco, which is a big deal considering that the ACS is the largest scientific society in the world.
(NaturalHealth365) The first global symposium focused on the health benefits of pure maple syrup was held in early April 2017. This symposium was part of the 253rd annual American Chemical Society (ACS) meeting in San Francisco, which is a big deal considering that the ACS is the largest scientific society in the world.
The special symposium was called “Chemistry and Biological Effects of Maple Food Products.” Scientists gathered to share research on maple syrup’s positive effects on inflammation, infection, and the gut microbiome. Since then, new research has shown that certain aspects of maple syrup may even offer cancer-fighting benefits. A study published in Oncology Reports discovered that maple syrup contains some substances other than the usual antioxidants, which may help fight colorectal cancer.
Maple syrup is used traditionally by Native populations for its healing properties
Chronic inflammation is at the root of many diseases and conditions, including arthritis, Alzheimer’s disease, and cancer. It is also a factor in liver disease, metabolic syndrome, and brain health and can upset the balance of the gut microbiome.
Native populations in Canada have used maple syrup for centuries to help fight infections. Scientists have been studying the unique properties of pure maple syrup closely for over a decade.
Researchers have found that some of its health benefits are linked to a complex carbohydrate called inulin. This natural fiber acts as a prebiotic, encouraging the growth of positive gut bacteria, which supports immune system functioning.
Key compounds boost the effects of antibiotics
The beneficial compounds in maple syrup are numerous. Two additional compounds were discovered recently that have antioxidant properties, bringing the known count of beneficial phytonutrients up to 65. A polyphenolic molecule called Quebecol and an analog called isoquebecol show significant positive effects against inflammation.
Research from McGill University has also found that maple syrup can dramatically boost the antimicrobial effect of antibiotics. When carbenicillin and ciprofloxacin were administered along with the syrup, up to 90 percent fewer antibiotics could be used with the same healing results. These results hold tremendous promise for fighting viruses and “superbugs.”
Pure maple syrup also contains key vitamins and minerals that make it a “functional food.” A maple sap drink formulation was found to bring a symbiotic (both probiotic and prebiotic) benefit to gut flora balance. This could offer an added benefit for persons taking antibiotics.
Maple syrup is loaded with health-enhancing polyphenols
As you know, gut health and balance are crucial to immune system health. A healthy immune system can then, in turn, help protect the body against chronic inflammation – which is at the root of many debilitating health conditions.
While some inflammation is part of normal immune system response, chronic inflammation can cause (or make worse) many health problems. Fortunately, foods rich in polyphenols, like pure maple syrup, help fight off and prevent chronic inflammation.
Examples of other polyphenol-rich foods include lots of fruits and vegetables or green tea.
Maple products are produced in abundance in places like Vermont (in the United States) and Canada, with around 7,500 businesses and 44 million taps in Quebec alone. As awareness of the anti-inflammatory and antimicrobial properties spreads, interest and demand worldwide will no doubt increase for this sweet (small) addition to the diet.
Sources for this article:
Natural Therapies for Cystic Fibrosis
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/05/02/natural-therapies-for-cystic-fibrosis.aspx
Analysis by Dr. Joseph Mercola May 02, 2024

STORY AT-A-GLANCE
- Cystic fibrosis (CF) is a severe genetic disorder marked by excessive, thick mucus in the lungs and other organs, leading to chronic inflammation and reduced lung function, necessitating daily breathing treatments
- Nutritional support, including vitamins A, C, E, zinc, omega-3 (DHA), garlic, ginseng and curcumin, is commonly recommended for CF patients
- Vitamin D deficiency is notably prevalent among CF patients, affecting their lung function and overall disease progression; maintaining a vitamin D level of at least 60 ng/mL is recommended for mitigating these effects
- N-acetylcysteine (NAC) has emerged as a significant antioxidant in CF management, helping to reduce inflammation, break down mucus, enhance antibiotic effectiveness, and support immune response
- Reducing dietary intake of linoleic acid (LA) is advised for CF patients due to its potential to exacerbate disease symptoms through mitochondrial dysfunction
Cystic fibrosis (CF) is a progressive and terminal genetic disease that causes an overproduction and buildup of thick, sticky mucus in the lungs and other organs that lead to chronic inflammation and, eventually, a deterioration of lung function.
The disease requires daily breathing treatment for up to five hours a day, and many CF patients end up spending a lot of time in the hospital due to respiratory distress and chronic infections. Pancreatic and gastrointestinal complications, including malabsorption of proteins and fats, and chronic liver disease are also common. The median survival age is about 35 years.1
A 2012 paper2 in the Journal of Pharmacy Practice reviewed several of the most commonly recommended nutritional supports for those with CF, including vitamins A, C and E, zinc, omega-3 docosahexaenoic (DHA), garlic, ginseng and curcumin.
According to this paper, 75% of CF patients routinely use complementary and alternative medicine (CAM) in addition to their regular treatment, so it’s important for health professionals to be familiar with these options.
More recently, a scientific review3 published in 2022 highlighted the role of N-acetylcysteine (NAC) in the clinical management of CF. Removing all linoleic acid (LA) from your diet and optimizing your vitamin D level are two additional foundational recommendations that I will go over here.
Vitamins A, C and E and Zinc
Many CF patients have poor absorption of fat-soluble vitamins such as A and E, due to malabsorption of fats. For this reason, supplementation with these vitamins is often recommended. As a rule, patients are advised to consume between 120% and 150% of the recommended daily allowance (RDA) of nutrients to prevent premature death from malnutrition.4
The Journal of Pharmacy Practice paper5 cites research from 2001, which found that CF patients who received 1 milligram of beta-carotene per kilo of bodyweight per day (up to 50 mg per day) for three months, followed by a daily dose of 10 mg for another three months, experienced “a statistically significant decrease in the number of days of treatment with systemic antibiotics.”
Zinc supplementation at a dose of 30 mg per day has also been shown to reduce the average days of antibiotic use, and a pediatric study using an antioxidant-rich multivitamin supplement containing vitamins A, C, E and zinc and other micronutrients found “modest improvement” in lung function.
How to Select a Good Vitamin Supplement
Vitamin A (retinol) should not be confused with beta-carotene, which is pre-vitamin A that gets converted into vitamin A in your liver. To use beta-carotene, you need to have a well-functioning digestive tract and sufficient bile produced by your gallbladder. Specific enzymes are also needed to break down the carotene for the conversion into retinol to occur.
Most people have poor gut health, and this is particularly true for CF patients, which makes beta-carotene a poor alternative as a primary source of vitamin A. Retinol — preformed vitamin A — is found in animal products such as grass fed meat and poultry, liver, fish and raw organic dairy products like butter. This is the form of vitamin A your body can use, so make sure the vitamin A you buy specifies “retinol” or “retinoic acid,” and not just “vitamin A” or “beta-carotene.”
When it comes to vitamin C, you want to make sure it’s liposomal, as it will allow you to take higher dosages without causing loose stools. It’s also absorbed better.
While healthy people can typically get enough vitamin C from food such as red pepper, broccoli, kiwi, strawberries, citrus fruits, camu camu, rose hips or acerola cherries, if you’re ill, you need far more than what can be obtained from food (possibly except for acerola cherry, which contains 80 mg of vitamin C per cherry).
Selecting a natural supplement is particularly important when it comes to vitamin E. Studies have demonstrated that synthetic vitamin E has the opposite effect of natural vitamin E, such as increasing the risk of certain cancers rather than lowering it,6,7,8 for example. So, it’s important to make sure you’re getting a natural version.
What you’re looking for is “d alpha tocopherol.” Avoid all synthetic forms such as succinate, acetate and the racemic DL isomer. You want the pure D isomer, which is what your body can use. There are also other vitamin E isomers, and you want the complete spectrum of tocotrienols, specifically the beta, gamma, and delta types of vitamin E, in the effective D isomer.

Save This Article for Later – Get the PDF Now
Vitamin D
Vitamin D also plays a crucial role in the health and management of CF, offering several benefits backed by scientific research. A systematic review and meta-analysis9 published in January 2024 revealed that CF patients typically have significantly lower levels of vitamin D compared to healthy controls, both in childhood/adolescence and adulthood.
The prevalence of vitamin D levels considered insufficient (20–30 ng/mL) in CF patients was found to be 36% among pediatrics and adolescents and 63% among adults. Twenty-seven percent of pediatric/adolescent CF patients and 35% of adults had vitamin D levels of below 20 ng/mL, which is a severe deficiency state.
Ideally, you’d want a vitamin D level of at least 60 ng/mL year-round. To reach that level, I recommend daily walks with minimal clothing for 30 minutes before and after solar noon, for a total of one hour. During summertime, that would be right around 1 pm.
While oral vitamin D3 supplementation is an option if you cannot get enough sun exposure, you’ll miss out on many of the other health benefits that sun exposure provides. You also need to make sure you’re taking vitamin K2 and magnesium when using oral supplementation.
How Vitamin D Deficiency Impacts CF
Another study10 focused on the relationship between vitamin D levels and lung function in CF patients, specifically through the lung clearance index (LCI), a measure of lung function. The study found a strong negative correlation between vitamin D levels and LCI, indicating that lower vitamin D levels are associated with worse lung function.
It also noted that vitamin D deficiency could be particularly detrimental in patients with comorbidities such as cystic fibrosis-related diabetes (CFRD) and cystic fibrosis liver disease (CFLD).
Additionally, a pilot study11 published in 2019 investigated the immunomodulatory effects of vitamin D on pro-inflammatory cytokines in the airways of CF patients infected by Pseudomonas aeruginosa.
They found that supplementation with vitamin D led to a decrease in the levels of interleukins IL-17A and IL-23 in the exhaled breath condensate (EBC), indicating a reduction in inflammation.
These cytokines are known to play roles in the body’s inflammatory response, suggesting that vitamin D supplementation can help modulate the immune response in CF patients, potentially mitigating lung damage caused by chronic infections.
These findings collectively underscore the importance of monitoring and managing vitamin D levels in CF patients, not only for bone health but also for its potential benefits in improving lung function, reducing inflammation, and enhancing the body’s response to infections.
N-acetylcysteine (NAC)
NAC is a precursor to your body’s production of glutathione (GSH), also has an important role in the management of CF.12 As noted in the journal Pharmaceuticals:13
“[NAC] has been known for a long time as a powerful antioxidant and as an antidote for paracetamol overdose. However, other activities related to this molecule have been discovered over the years, making it a promising drug for diseases such as cystic fibrosis (CF).
Its antioxidant activity plays a key role in CF airway inflammation and redox imbalance. Furthermore, this molecule appears to play an important role in the prevention and eradication of biofilms resulting from CF airway infections, in particular that of Pseudomonas aeruginosa …
To do this, NAC can act alone, but it can also be used as an adjuvant molecule to known drugs (antibiotics/anti-inflammatories) to increase their activity.”
Here’s a quick overview of how NAC can be beneficial for CF patients, drawing on its various mechanisms:14
| Fighting oxidative stress — There’s a battle between damaging oxidative substances (ROS) and the body’s antioxidants. NAC steps in as a reinforcement, helping to boost the body’s antioxidant levels, especially glutathione (GSH). This helps to mitigate the damage caused by oxidative stress, which can worsen CF conditions. |
| Reducing inflammation — CF lungs are often inflamed, partly due to overactive immune responses that attract too many neutrophils (a type of white blood cell) to the site. These neutrophils release substances that can damage lung tissue. NAC helps calm this overreaction, reducing inflammation by modulating the production of molecules like cytokines that drive the inflammatory process. |
| Breaking down mucus — The thick mucus in CF can trap bacteria, creating biofilms that are hard to treat. NAC can break the sulfur bonds in the mucus, making it less sticky and easier to clear from the lungs. This action helps disrupt the biofilm structure, allowing antibiotics to reach and kill bacteria more effectively. |
| Enhancing antibiotic effectiveness — The presence of biofilms and thick mucus in CF lungs can make bacteria resistant to antibiotics. NAC can make these bacteria more susceptible to antibiotics by breaking down the biofilms. It can also work synergistically with certain antibiotics, improving their ability to kill bacteria. |
| Acting against bacteria directly — Even though NAC is not an antibiotic, it has properties that can directly inhibit the growth of bacteria and their ability to form biofilms. This adds an extra layer of defense against lung infections. |
| Supporting healthy immune responses — By reducing the oxidative stress and helping to manage the inflammatory response, NAC can indirectly support the body’s immune system, making it more effective at fighting off infections without causing additional damage to lung tissues. |
| Improving cell function — On a cellular level, NAC might help correct some of the dysfunction caused by the CF mutation. It has been suggested that NAC can help with the maturation and function of CFTR proteins, which are faulty in CF, thereby helping to alleviate some of the symptoms. |
Omega-3
Omega-3 is also thought to be important for CF patients because deficiency has been linked to worsened pulmonary and GI symptoms, as well as CF progression. DHA, in particular, is important, as it has a beneficial impact on lung function. Previous research has concluded that doses up to 50 mg of DHA per kilo of bodyweight is safe for CF patients.15
When it comes to omega-3, I recommend trying to get most of it from omega-3-rich seafood, such as wild-caught Alaskan salmon, herring, sardines, mackerel and anchovies. If using a supplement, avoid synthetic fish oils and opt for krill oil instead.
Herbal Remedies
Herbal remedies recommended for CF include:16
- Garlic, which has antibacterial effects.
- Ginseng, which has antioxidant, antimicrobial and immune modulating effects. Aqueous extract of ginseng has been shown to be effective in inhibiting P aeruginosa, a bacteria often involved in chronic pulmonary infections, including antibiotic-resistant strains.
- Curcumin, which has antioxidant properties. Limited data also suggests it may increase CFTR-regulated channel activity in CF patients. CFTR is a protein that, when dysfunctional, results in the development of CF symptoms.
Eliminate Linoleic Acid From Your Diet
As important as supplementing certain nutrients might be, CF patients must also be vigilant about avoiding certain things. As explained in my in-depth review, “Linoleic Acid — The Most Destructive Ingredient in Your Diet,” linoleic acid (LA) — an omega-6 polyunsaturated fat (PUFA) — acts as a mitochondrial poison and the primary contributor to all chronic disease.
If you have CF, I strongly advise you to eliminate as much LA from your diet as humanly possible. While LA is found in most foods, by eliminating processed foods, condiments, seed oils for cooking, fast food and restaurant food, and conventionally raised pork, chicken and eggs, you can get your LA intake below 5% of daily calories, which is about what our ancestors used to get.
While there are no studies detailing direct harm caused by LA in CF, dysfunctional lipid metabolism, including LA metabolism, is a characteristic of CF. So, there appears to be a complex interaction with LA that could influence disease outcomes.
Excess LA is a primary driver of mitochondrial dysfunction, and well-functioning mitochondria are a prerequisite for health and disease prevention.
That said, considering excess LA is a primary driver of mitochondrial dysfunction, there’s every reason to believe that it will have a detrimental impact on CF. After all, health and disease prevention require you to have well-functioning mitochondria. It’s as foundational as you can get.
If you’re not sure how much you’re eating, enter your food intake into Cronometer — a free online nutrition tracker — and it will provide you with your total LA intake. Cronometer will tell you how much omega-6 you’re getting from your food down to the 10th of a gram, and you can assume 90% of that is LA. Anything over 10 grams of LA is likely to cause problems.
Healthy fat replacements include tallow, butter or ghee, all of which are excellent for cooking. The table below provides a fairly comprehensive list of the most commonly consumed oils and their approximate LA content.
In general, the lowest LA-containing fats — butter and beef tallow — would be the fats of choice. These excellent cooking fats would not only be the lowest in LA, but will also provide the fat-soluble vitamins, A, D, and K2. Coconut oil is also very low in LA but doesn’t provide the important fat-soluble vitamins that tallow and butter contain.
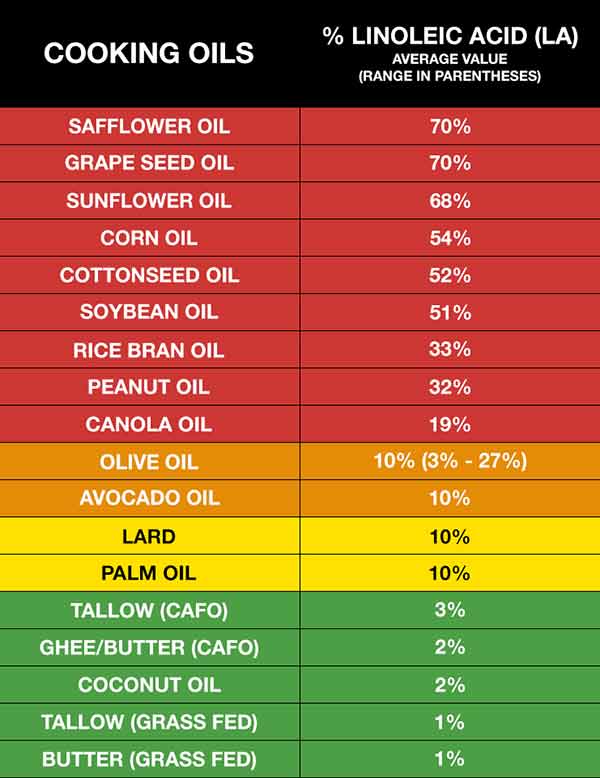
Vitamin E Prevents Oxidation of LA
If you’ve been eating a high-PUFA diet for a long time, consider taking vitamin E regularly until you get your LA down to healthy levels. As noted earlier, CF patients need extra vitamin E anyway, and this is yet another reason to make sure you’re getting enough.
High LA levels increase a potentially dangerous process in your body called lipolysis — the liberation of fatty acids from your fat cells into your bloodstream where they are mobilized. This then increases the oxidation of LA, which is precisely what you want to avoid. Ideally, you want to keep LA in your fat cells until they metabolize it with peroxisomes. Vitamin E can help neutralize this damaging effect of LA.
Due to the high LA burden, few people can get enough vitamin E from their diet to suppress the oxidative destruction caused by LA unless they’re supplementing with vitamin E.
The good news is that since the supplementation is short term, you’re not going to need it the rest of your life. If you can keep your LA intake to below 5 grams a day for three years, it’s likely you may not even need it at all, or at most, only a few times a month.
The Story of Claire Wineland
Claire Wineland, an inspirational speaker and YouTube sensation, was diagnosed with CF at birth. At age 13, she founded the Claire’s Place Foundation17 to help families with children who have CF. She died September 2, 2018, from a massive stroke following an otherwise successful lung transplant.
In 2016, Wineland appeared in an episode of “My Last Days,” a limited CW docuseries hosted by Justin Baldoni, featuring people living with terminal illness. September 2, 2019, YouTube Originals released the documentary “CLAIRE,” directed by Nicholas Reed (above).
While filled with chronic illness, Wineland’s life was a testament to how to live life well, with purpose and gratitude. It’s a potent reminder of how we need to live life to the fullest, even though we might die tomorrow. “I’ve always loved the idea of bringing life into places where people think life doesn’t really exist,” Wineland said.
Wineland’s mother said she was convinced her daughter came into the world with a mission to share the message of “what it’s like to be blessed with life.” I couldn’t agree more.
- 1, 2, 4, 5, 15, 16 Journal of Pharmacy Practice 2012; 26(1): 14-17
- 3, 12, 13, 14 Pharmaceuticals February 2022; 15(2): 217
- 6 Cancer Prevention Research May 2012, DOI: 10.1158/1940-6207.CAPR-12-0045
- 7 Science Daily April 23, 2012
- 8 Sci Transl Med 29 January 2014: Vol. 6, Issue 221, p. 221ra15
- 9 Journal of Health, Population and Nutrition January 17, 2024; 43, Article number 11
- 10 Children 2022; 9(3): 329
- 11 Italian Journal of Pediatrics 2019; 45, Article number 41
- 17 Claire’s Place Foundation, Inc