Reproduced from original OMNS article (OrthoMolecular News Service):
http://orthomolecular.org/
Subscribe to the free Orthomolecular Newsletter: http://orthomolecular.org/subscribe.html
Go to the OMNS Archive: http://orthomolecular.org/resources/omns/index.shtml
Orthomolecular Medicine News Service, December 17, 2023
Commentary by Thomas E. Levy, MD, JD
OMNS (December 17, 2023) Breast cancer causes enormous morbidity and mortality around the world, and its traditional treatment, along with the relentless progression of the disease, greatly impacts the quality of life for both patients and their families. This cancer basically targets just women, as only a relatively minimal number of cases occur in men (roughly 1%). [1] Yet, despite its predilection for women, breast cancer is still the most common of malignancies (aside from non-melanoma skin cancers) statistically in the overall population. It continues to be the leading cause of cancer deaths across the planet. [2]
Redox Biology and Toxins
Reduction and oxidation basically refer to the movement of electrons between molecules. When a normal biomolecule with a normal electron content is depleted of one or more electrons, it becomes oxidized. And when that oxidized biomolecule can regain the lost electron(s), it returns to a normal, reduced chemical state. A reduced biomolecule functions normally, while an oxidized biomolecule either partially or completely loses its normal chemical/biological function. More oxidized biomolecules result in the accumulation of largely metabolically inert agents that only occupy space, interfering with normal chemical reactions and no longer directly supporting normal biological function. Examples of biomolecules include sugars, fats, proteins, enzymes, nucleic acids, and structural molecules.
Redox (reduction-oxidation) biology is based on the concept that all biological health is directly due to the degree of reduction versus oxidation in the biomolecules throughout the body. Higher reduction/oxidation ratios indicate good cellular health. This has led to the frequent use of the term “oxidative stress” as the premier biomarker and measuring stick of all disease.
Widely discussed in the medical and scientific literature, increased oxidative stress, or the excess presence of oxidized biomolecules, is always the primary pathophysiology of any disease under consideration. [3,4] It is characterized by a relatively low antioxidant presence and/or an increased pro-oxidant presence. At the cellular level, all diseases or medical conditions have increased oxidative stress in the cells of the affected organs or tissues. The extracellular areas are often involved as well. As pathology cannot exist in the absence of excess oxidation, there are no exceptions to this premise.
All toxins damage by directly or indirectly causing the oxidation of important biomolecules. Oxidation is the chemical process of giving up, or losing, one or more electrons to an electron-robbing toxin (pro-oxidant) that never surrenders that electron back to an oxidized biomolecule once it is acquired. Unless an agent results in the oxidation of biomolecules in the body along with the permanent retention of the electrons it has taken, it is not toxic, and it cannot be toxic. Clinical toxicity and any symptoms of toxicity cannot exist in the absence of excess oxidized biomolecules.
As excess oxidation is the basis of all disease, it logically follows that all cancers, either in the breast or elsewhere, result from excessively and chronically elevated oxidative stress at the affected tissue site. This elevated oxidative stress is always secondary to electron-depleted toxins, also known as pro-oxidants, poisons, free radicals, reactive oxygen species, or oxidizing agents.
This leads to the following two questions:
- What is the source of the toxins in breast cancer, and
- What is causing them to excessively accumulate?
Breast Cancer Pathophysiology
All chronic degenerative diseases, including cancer, only arise when an area of affected tissue becomes substantially inflamed and remains that way. Phrased differently, the areas in the body that have exceptionally increased and chronic oxidative stress are the areas where malignant transformation eventually takes place. Lesser degrees of increased oxidative stress, depending on their location, underlie the development and maintenance of all non-malignant diseases as well. But the highest chronic elevations of oxidative stress, both intracellularly and extracellularly, are the reasons for the initiation and evolution of cancerous growth. No cancer has ever developed in an area that was not already inflamed. While a cancer can metastatically seed abnormal cells in a previously normal tissue site, the primary cancer focus will never be initiated in normal, uninflamed tissue.
A prolonged and sizeable presence of toxins always precedes the development of cancer in the affected areas of the breast. These toxins are produced by slow-growing pathogens (colonizations), and the pathogens themselves will often be found at the cancer site as well. But toxins (highly pro-oxidant molecules) must always be present in order to provoke and sustain a state of chronic inflammation and excess oxidation.
The amount of time that such a toxin/pathogen accumulation needs to be present before a cancer develops is highly variable. Some women with exceptionally strong immune systems, high antioxidant intake, and a relatively lesser degree of toxin/pathogen presence may never demonstrate malignant transformation. Of note, benign breast lumps and other forms of breast pathology result from lesser degrees of toxin exposure.
No pathology of any kind can develop when a tissue has intracellular and extracellular levels of oxidation that are physiological in degree (from normal metabolism). Only increased levels of oxidation can result in pathology. And only extremely increased levels of oxidation result in the appearance of cancer.
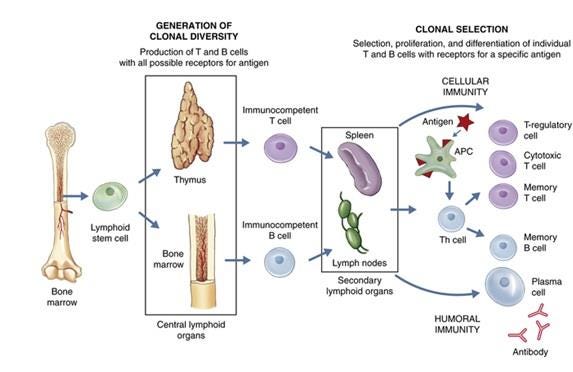
In addition to a blood circulation, the body has a lymphatic circulation as well. This circulation moves lymph, the plasma-like extracellular fluid bathing the cells throughout the body, into the venous blood circulation. Under normal circumstances, this lymph flow is one-way only in the direction needed to reach the blood. [5] The primary role of the lymphatic circulation is to provide an outlet for cellular waste products, excess water, and toxins, as well as to support an immune defense against pathogens. [6] It also periodically condenses into focal bodies known as the lymph nodes.
These lymph nodes, of which there are about 500 to 600 in the body, work to concentrate B- and T-lymphocytes needed to combat the infectious agents that are encountered, such that the lymph itself is rendered sterile by the time it leaves the lymph nodes and reaches the blood. [7,8] When draining a large enough source of infection, such lymph nodes will readily enlarge and become sore where they can be felt (palpated), such as in the neck, armpits, or groin areas. Once the processed lymph finally reaches the blood circulation, multiple ways of metabolizing and excreting the remaining non-infective extracellular debris are then available.
The breasts have an extensive lymphatic circulation, and much of its lymph comes from drainage of the head and neck. A portion of the breast lymph subsequently flows into a large collecting vessel (thoracic duct), which then empties into the venous circulation. The rest of it first flows into the extensive lymphatic network in the armpits before eventually reaching the thoracic duct and the blood.
The lymphatic vessels have a limited ability to contract and promote a one-way flow of lymph. [9] However, this lymphatic movement can be slowed, stopped, or even reversed in direction by the presence of sufficient inflammation and structural damage in the tissue being drained. When there is sufficient impairment of normal lymphatic flow, tissue swelling (lymphedema) can result.
In the breast, this impairment of lymphatic drainage can result from either the chronic inflammation in the cancerous tissue, or much more commonly, following the surgical removal of cancer-laden axillary lymph nodes draining the breast. [10,11] The fewer draining lymphatic pathways available, the more likely lymph flow will slow enough to accumulate. Together, both situations result in about 20% of women with breast cancer eventually developing arm swelling due to the back-up of lymph. [12,13]
As with tissues elsewhere in the body, the lymphatic system also drains the superficial gum tissue, the deep gum tissue (periodontium), the teeth, and the tonsils. This drainage largely follows gravity and is filtered in the lymphatic vasculature in the floor of the mouth and then the neck. From there much of the drainage proceeds further down into the rich network of lymphatic vessels in the chest and the breasts, with most of the breast lymph then draining directly into the armpits. [14-16] Deep periodontal infection (periodontitis) has been “linked” to many different cancers, including the breast. Of significant note,
Maintenance of periodontal health has been found to be effective in the primary prevention of breast cancer. This indicates that periodontal infection has a cause-and-effect relationship to breast cancer, not just a link, association, or correlation. [17]
Left unresolved, periodontitis seeds pathogens and their associated toxins throughout the body. To assert that disease occurring after such typical oral pathogens start growing in different tissues is some ill-defined “association” and not a straightforward cause-and-effect relationship defies simple logic. Aside from breast disease and breast cancer, chronically infected gums have been significantly linked to nearly all diseases and conditions. Some studies also document improvement of the “linked” disease with effective periodontitis treatment, as well as a worsening of the disease as periodontitis progresses. This further indicates that periodontitis has a cause-and-effect with most chronic diseases. These diseases and conditions include the following:
- Cardiovascular disease and all-cause mortality, including atherosclerosis, myocardial infarction, heart failure, abnormal lipid and cholesterol metabolism (metabolic syndrome), diabetes, and arterial calcification [18-32]
- Neurological disease, including migraine, seizure, depression, bipolar disorder, dementia, Alzheimer’s disease, Parkinson’s disease, brain abscess and multiple sclerosis [33-53]
- Chronic pulmonary disease, pneumonia, asthma, allergic rhinitis [54-60]
- Vascular disease [61,62]
- Obesity [63,64]
- Inflammatory bowel disease [65-67]
- Inflammatory bone diseases, including arthritis and osteoporosis [68-73]
- Kidney disease [74-76]
- Cancers (pancreatic, lung, liver, colorectal, esophageal, oral cavity and throat, head and neck, stomach, prostate, blood, skin, and cancer in general) [77-92]
- Female infertility and adverse pregnancy and neonatal/birth outcomes [93-95]
- Thyroid disease [96]
- Anemia [97,98]
- Eye disorders [99,100]
- Psoriasis [101-104]
- Ear disorders (hearing loss, vertigo) [105-107]
- Polycystic ovary syndrome [108]
- Autoimmune disease [109-111]
- Erectile dysfunction [112]
- Increased body-wide inflammation (elevated C-reactive protein levels) [113-115]
- Depressed vitamin levels (C and D) and antioxidants [116-122]
The data above on chronic disease and periodontal infection is vital to understanding the impact of root canals and other infected teeth on the general health. Because the pathogens found in infected teeth only come from deep gum infections (except when large cavities allow the pulp to become infected from above), the infections found around the root tips of affected teeth have the same infectious profile as is found in periodontitis. However, the infected teeth, which include all root canal-treated teeth, are even more disease-causing than the infected gums, since they also have the additional following characteristics:
- The infected teeth have a much greater amount of infectious material, often manifest as root tip (apical) abscesses on X-ray.
- The infectious content in and around the root tips of the infected teeth drains directly into the venous circulation.
- The infectious content in and around the root tips of the infected teeth are also released into the extracellular fluid and drained directly into the lymphatic system of the teeth and jawbone.
- The act of chewing on the infected teeth greatly magnifies the expression of pathogens and toxins into the blood and lymph, as extraordinary pressures are generated between opposing teeth. Since pathogen release into the lymph occurs in addition to their release into the venous blood, the delivery of these oral pathogens and toxins to the entire body is more effective and efficient with chewing on infected teeth than if the pathogens and toxins were just directly injected into a vein with a syringe.
The release of highly pathogenic bacteria into the blood during a root canal procedure has been clearly documented. Of note, their release occurs in the absence of any chewing pressure that would further promote pathogen release. [123,124]
Traditional dentists and endodontists (root canal specialists) somehow deny and/or blind themselves to the massive documentation that all root canals are infected. Instead, they collectively maintain that a successful root canal procedure leaves the tooth infection-free just because a root tip abscess was reduced in size and the pain associated with the acute abscess was relieved.
Nevertheless, all the research on the impact of periodontitis and abscessed teeth on all chronic disease applies to all root canals as well, regardless of how well they were performed technically. Although less extensively studied than the relation of just periodontitis with chronic diseases, a great deal of research has also established a link between chronically abscessed teeth (CAP-chronic apical periodontitis) and many different diseases. CAP simply means an extension of and a more advanced form of deep gum inflammation and infection (periodontitis), with root tip abscesses seen on imaging. Significant research studies have documented this abscessed tooth-chronic disease link, which includes all root canals that have resulted in the reduction of root tip abscesses on imaging studies. These studies directly mirror the many studies on early periodontitis and chronic diseases cited above and include the following:
- Cardiovascular disease [125-130]
- Neurological disease [131-137]
- Eye infection [138]
- Inflammatory bowel disease (including Crohn’s disease and chronic ulcerative colitis) [139-142]
- Diabetes [143]
- Liver disease [144,145]
- Kidney disease [146,147]
- Inflammatory bone diseases [148-152]
- Autoimmune disease [153,154]
- Adverse pregnancy outcomes [155,156]
- Increased body-wide inflammation (elevated C-reactive protein levels) [157-161]
- Reservoir for a wide variety of pathogens (bacteria, fungi, and viruses, including Epstein-Barr and herpes) [162-166]
- Increased morbidity and mortality in COVID-19 patients [167]
- Decreased physical fitness/capacity [168]
- Body-wide disease in general [169]
While other factors may be involved, it appears likely that men have virtually no breast cancer because the amount of breast tissue is so much smaller than in women, and there is much less toxic and infected lymph from oral cavity infections getting continually filtered in that tissue. And even though there is a large difference in the average amount of breast tissue between men and women, the lymphatic drainage patterns are largely the same. [170] Also, larger and denser breasts, along with overly constrictive bras and clothing, can all impede the rate at which lymph can be conducted through the breasts. Anything that slows lymphatic flow, especially if it has a significant toxin/pathogen content, will be a factor in determining whether significant inflammation is allowed to take hold in an area of the breast draining the lymph from the oral cavity. Consistent with this concept, studies have shown that very large-breasted women who undergo breast reduction surgery lower their chances of breast cancer. [171] Furthermore, it has been shown that women with larger breasts fare worse with breast cancer than women with smaller breasts. [172]
Root Canal-Treated Teeth
The root canal procedure is one of the most common dental procedures. A meta-analysis revealed that more than half of the subjects in the populations studied had at least one root canal. [173] A very large review and meta-analysis also found that at least half of the population has at least one abscessed tooth. [174] When combined with the prevalence of abscessed teeth that have not received a root canal treatment, the prevalence of infected teeth runs between 55% and 70% of the subjects in the studies. [175-180] Depending on the information source, between 25 and 45 million root canal procedures are performed in the United States every year. Even the low side of the estimate means that a significant majority of adults are always chewing on one or more infected teeth.
Another study found that over 60% of people in Europe had abscessed teeth, with the prevalence steadily increasing with age. [181] Furthermore, fully 25% of teeth that have had procedures other than root canal treatments end up chronically abscessed as well. [182]
Root canal-treated teeth are generally performed when a patient presents with a painful, acutely-abscessed tooth. The “successful” root canal procedure results in a tooth that no longer hurts, resulting in a happy patient and satisfied dentist, at least for the moment. However, the infection remains as long as the tooth remains unextracted, or when the socket infection remains is not completely cleaned out after extraction.
There is an enormous variety and a large total number of different pathogens and other microbes found in and around the root tips of root canal-treated teeth. Fungi, viruses, protozoa and over 460 different types of bacteria have been identified in these infections. [183] No two root canals have the same assortment of indwelling pathogens, and this is why no two root canals inflict the same degree of infectious/toxic damage to the body. Nevertheless, even the “least toxic” root canals can wreak havoc throughout the body.
The physiological core of the tooth, known as the pulp, contains the nerves, blood vessels, and connective tissue matrix that keep the tooth alive and viable. Once this pulp has become infected, there is no way to eradicate the infection and restore the pulp to its normal, health-supporting state. Instead, the removal of the pulp by the root canal procedure permanently prevents immune system access to the pathogens in the tooth, especially in the miles of dentinal tubules extending away from the pulp throughout the tooth structure.
Without immune support, no infection can be resolved. Furthermore, even without the root canal procedure, the infected pulp quickly destroys the pulp structure itself, just leaving a collection of pus and dead (necrotic) cells that can never be returned to normal. Even though pain can still be felt in the root tips embedded in the jawbone, the upper part of the tooth and the pulp is simply a non-vital shell.
In order to stop the immediate infection-causing pain and remove much of the bulk (but never all) of the infection, the root canal procedure drills and routs out as much of the pulp as can be reached, after which it is filled in with an agent to maintain the overall tooth structure. The ends of the pulp space extend to the tooth root tips embedded in the jawbone, and the pulp infection and its necrotic debris effectively “collects” there. This results in well-defined abscesses surrounding the root tips.
Chronically infected teeth will usually be found to have clearly visible evidence of this pathology at the root tips. On X-ray or on computed tomography studies variably-sized abscesses will nearly always be seen, appearing as dark areas, or radiolucencies, surrounding the root tips. Rarely, the infected tooth might not contain enough infected debris to be visible in an imaging study, but the lack of an identifiable abscess does not mean the infection is still not there.
When a root canal procedure has been performed with optimal expertise, much of the associated root tip abscess will be removed (debulked), and follow-up imaging will no longer easily detect it. However, this does not mean the infection is gone, only that it has been effectively drained. Pathogens and their toxins are still readily expressed into the blood and lymph, especially during chewing.
Dr. Boyd Haley conclusively proved that all root canals produce and collect toxins. He devised a test using a process called nucleotide photo affinity labeling to measure the impact of the pathogen-generated toxins in extracted root canal-treated teeth on five key human enzymes. After studying over 5,000 consecutive extracted root canal-treated teeth sent to him from around the country, the results were stunning. ALL tested teeth had significant toxin content. Differences in the degree of toxicity among the teeth were seen, but none were toxin-free. Such variability in toxicity is to be expected, as no two root canals have the same pathogen population. [184] Furthermore, normal teeth extracted for orthodontic purposes never demonstrated any toxicity, even to a minor degree, ruling out “mouth contamination” as a potential reason for the results.
Of note, Dr. Haley found similar toxin profiles in the specimens sent to him from cavitation surgery. Cavitations occur when chronic infection remains in the healed-over sockets of extracted teeth. [185] Cavitations have a comparable connection to chronic diseases, including breast cancer, although it is much less extensively studied than the relation between abscessed teeth and chronic disease. [186-189]
In addition to the clear visual appearance of chronic infection at the time of extraction, frequently accompanied by putrid odors, ALL root canal teeth extraction sites have pathogens that can be cultured, and microscopic examinations of biopsy specimens always reveal inflamed and necrotic bone and tissue cells resulting from the chronic infection.
Infected Teeth-The Hidden Pandemic
Chronically abscessed teeth, as seen in imaging studies, are very common. Furthermore, they are nearly always completely free of pain or any other associated symptoms, and the patient has no reason to suspect that there are any problems in the mouth. In contrast the acutely abscessed tooth, for which many root canals are performed, are typically extremely painful. This is why chronic diseases in adults are the rule and not the exception. Too many physicians and their patients simply “expect” that hypertension, diabetes, cancer, or heart disease are the norm for many older adults. Also of note, the deciduous (non-permanent or baby) teeth in children demonstrate a high incidence of abscess formation. [190] When a child becomes chronically ill, a complete oral examination is just as important as in the adult with a chronic disease. So, for all ages, the important take-away point is that:
When the mouth is infection-free, all chronic diseases are very rare. And when there is a chronic disease, oral- or gut-derived pathogen colonization of the affected tissue with local toxin production is almost always the cause.
While some individuals, in a completely unpredictable manner, can have one or more root canals without ever resulting in negative clinical consequences, this is very rare. However, significant laboratory abnormalities are often present even when a chronic disease is not yet manifest. Also, clinical medicine always looks for a prompt and clear-cut relationship between an intervention and a negative clinical impact. With root canals and other chronically infected teeth, the leakage of pathogens and toxins can be slow, and breast cancer or a heart attack due to those infected teeth can take years to occur.
Complications can occur rapidly after a root canal procedure, but this is not a very common consequence. If that were the case, root canal treatments would have been abandoned long ago. But when someone gets breast cancer years after a root canal, the status of the mouth is simply never considered as the possible reason by the clinician or the patient.
A particularly aggressive pathogen of periodontal origin, Fusobacterium nucleatum, has been found in human breast cancer tissue. In an animal model, this pathogen has been shown to promote tumor growth and metastatic spread. [191,192] Higher titers of oral pathogens inside breast cancer cells have also been shown to promote metastatic spread, with experimental reduction of these titers decreasing the chances of metastasis. [193] Animal studies have also shown a commonality of pathogen presence in the mouth, gut, and in breast tumors. [194]
Some researchers have actually termed breast cancer as an infectious disease. [195] Many other studies have consistently found pathogenic microbes, including viruses and fungi, in diseased breast tissue, including cancer, and much lower titers of non-pathogenic microbes in normal breast tissue. [196-204] As the mouth is always teeming with microbes (more than 700 different bacterial species) and its lymphatic circulation mostly drains into the breasts, the breast tissue is not completely microbe-free. [205,206] However, it should be pathogen-free, and the non-pathogenic microbes should always be very low in number and difficult to culture. [207]
Researchers found a 10-fold (1,000%) increase in bacterial load in breast tumors relative to normal breast tissue. [208,209]
In addition to the enormous amount of literature cited above that unequivocally ties mouth infections to chronic diseases, several other studies warrant special attention, as they reveal that pathogens of oral and gut origin have been shown to chronically colonize different diseased tissues, with continuous inflammation resulting from the on-site production of pathogen-related toxins. Breast cancer is but one of many infection-related chronic diseases. Chronic pathogen colonization (CPC) in diseased tissues is addressed more extensively elsewhere. [210] Especially noteworthy studies supporting the widespread presence of CPC and its disease-causing impact include the following:
- Pathogens in Alzheimer’s disease brain tissue and cerebrospinal fluid [211-218]
- Pathogens in Parkinson’s disease [219]
- Pathogens in multiple sclerosis brain tissue and cerebrospinal fluid [220,221]
- Pathogens in amyotrophic lateral sclerosis brain tissue and cerebrospinal fluid [222]
- Pathogens in the atherosclerotic lesions of coronary heart disease [223-226]
- Pathogens in intracranial aneurysms [227]
- Pathogens in abdominal aortic aneurysms [228]
- Pathogens in the acute blood clots causing myocardial infarctions [229,230]
- Pathogens in the acute blood clots causing lower limb thrombosis [231]
- Pathogens in the pericardial fluid surrounding the hearts of patients with coronary artery disease [232]
- Pathogens in the joints of patients with rheumatoid arthritis [233-235]
- Pathogens in the placentas of mothers with preterm and low birth weight infants [236,237]
- Pathogen antibodies in systemic lupus erythematosus patients [238,239]
- Pathogen antibodies in stroke patients [240,241]
- Pathogens in cancersBreast [242-244]
Oral, head, and neck [245-247]
Esophageal [248,249]
Liver pathology leading to cancer [250]
Prostate [251]
Pancreatic [252,253]
Colorectal [254,255]
- * Pathogens and chronic body-wide inflammation and chronic diseases in general [256-258]
All chronic diseases need to have a daily source of new oxidative stress greater than the daily intake of antioxidants in diet and supplementation. Otherwise, “chronic” diseases would resolve as the new antioxidant intake repairs the old oxidative damage. This source of the new daily oxidative stress nearly always arises from chronic pathogen colonization in the diseased organ or tissue. New toxin exposure in the affected tissue comes from on-site pathogen-generated toxins and the oxidized (toxic) products of pathogen metabolism. Pathogens also release enormous amounts of pro-oxidant free iron when they finally die and break apart.
Chronically Infected Tonsils
In the 1950s Dr. Josef Issels made some remarkable discoveries that remain largely unknown to the medical and dental community. [259] His clinic in Germany treated mostly advanced cancer patients who were seeking to avoid chemotherapy in their pursuit of health. In surveying his own clinic data he found that 98% of the cancer patients had between what he termed “two and ten dead teeth.” His treatment not only involved the proper removal of such infected and necrotic teeth, but also routine tonsillectomy. This was not initiated until he retrospectively observed that a significant number of his patients, who initially did well after the extractions, later experienced myocardial infarctions. After making tonsillectomies a part of his treatment protocol in these advanced cancer patients, the prevalence of heart attacks dropped from 40% to 5%.
Dr. Issels asserted that “chronically inflamed tonsils are primary head foci which sometimes have an even more damaging effect on the organism as a whole than dental foci,” noting that the tonsils are “excretion organs by which the lymphocytes, microbes, toxin-laden lymph, and other matter are discharged.”
Most significantly, Issels found that in every tonsillectomy performed, biopsy specimens revealed that “severe or very severe destructive tonsillar processes” were present along with chronic infection. This was in spite of the fact that the tonsils did not appear enlarged, inflamed, or infected on examination, which is the major reason they never get noticed or treated. Even though the chronic drainage of infected jawbone lymph results in the tonsils becoming chronically infected, it does not result in them becoming swollen, as is routinely seen with lymph nodes that are in the drainage pathway. This needs to be differentiated completely from acute or recurrent tonsillitis, with clear inflammation and often massive swelling, as often occurs in children.
The lymphatic flow into the tonsils is directly connected to the lymphatic drainage of the jawbone that anchors the infected teeth and gums discussed above. Issels noted that Indian ink injected into a sealed dental cavity results in the appearance of inky spots on the tonsillar surface in only 20 to 30 minutes, further establishing this connection.
The tonsils are designed to support the immune system in dealing with short-term and minimal pathogen challenges presented to the oral cavity. However, when the tonsil is continuously draining a chronic jawbone infection in the form of a root canal or other abscessed tooth, it is overwhelmed to the point that it goes from protecting against infection to becoming a major focal point of chronic infection itself.
In any patient who had infected teeth properly extracted, it must be assumed that the tonsils have already become major focal infections as well. This is especially the case when C-reactive protein (CRP) levels are elevated and remain so after the infected teeth have been properly removed. The complete elimination of oral cavity infections remains in question as long as the CRP remains elevated. [260]
Currently, there are several ways to resolve such chronic tonsillar infections, and they should all be used together if possible. Aside from tonsillectomy, the tonsils can be treated with:
- Direct ozone gas injections,
- Supported by periodic ozone ear insufflation treatments, and
- The application of a few drops of 1% pharmaceutical grade methylene blue directly on each tonsillar surface daily for several weeks.
This also works well for the large and inflamed tonsils of childhood tonsillitis. Furthermore, a normalization of a previously-elevated CRP level is good confirmation that they are no longer supporting body-wide inflammation. Many tonsillectomies could be completely avoided with these treatments.
Breast Cancer Treatment
Based on all the information and research data presented above, it is essential to have as complete a diagnosis of the oral cavity as possible. This requires having a cone beam computed tomography (CBCT or 3D X-ray) properly performed and expertly interpreted. [261] This is the best way to keep from missing a minimally abscessed tooth that it easily missed on regular dental X-rays. Leaving even one infected tooth unextracted can prevent much of the benefit of removing multiple other infected teeth and root canals. A comprehensive protocol for optimizing the benefits of the removal of infected teeth is addressed in detail elsewhere. This includes a recommended and detailed surgical protocol for the dentist performing the extractions. [260] Optimal healing is also strongly supported by a dentist experienced in the proper application of ozone to prevent infection and accelerate quality healing.
Uninformed Consent
While it is the purported standard of care to make sure the patient is completely aware of the nature of a proposed procedure and its potential complications, an informed consent does not currently exist for the root canal procedure. Root canal dentists are simply unwilling or unable to give the patient even a tiny fraction of the information cited in this article that documents that all root canal-treated teeth are chronically infected and remain that way until they are properly extracted.
The current root canal procedure should be limited to patients who are fully informed of the health risks but simply do not want an extraction for any reason at all. In that patient subset, having an expertly-performed root canal that debulks the amount of infection in the targeted tooth can offer benefits. Most patients will opt for protecting their health rather than keeping the tooth.
Also, no patient should be denied the option of infected tooth extraction at the outset, as recurrent abscess formation in root canals often occurs, and the patient then ends up receiving “redo” root canal procedures to debulk the new abscess, all the while spending more money, having their body subjected to a longer period of pathogen and toxin exposure, and experiencing more discomfort in the dental chair.
The devastating impact on the health of the body by keeping infected teeth in the mouth cannot be overstated. Breast cancer is one of many chronic diseases caused and supported by oral cavity infections. Heart attacks are almost entirely due to oral pathogens metastasizing into and colonizing the coronary artery walls. [262]
Recap
Breast cancer starts when infected lymph from infected teeth, gums, and tonsils drains into the breast to a degree that the lymph nodes and the immune system can no longer compensate against the chronic pathogen/toxin exposure. Pathogens are present in breast cancer cells and their surrounding extracellular environment. This is a cause-and-effect between the pathogen presence and the development of the cancer. It must never be dismissed as an unclear association, relationship, correlation, connection, link, or any other term that attempts to avoid concluding the fact that infected teeth cause cancer and chronic disease, both in the breasts and elsewhere in the body.
Breast cancer needs a comprehensive treatment protocol to achieve the best results, which often results in the disappearance of the cancer without surgery, radiation, or chemotherapy. As Dr. Issels asserted many years ago:
“Cancer is a general disease of the whole body from the outset. The tumour is a symptom of that illness.”
A healthy body does not “catch” cancer. Cancer only appears when a particular tissue area served by a chronically inflamed circulation receives the greatest and most unrelenting toxin exposure, which always comes from pathogen colonizations.
(Thomas E. Levy, MD, JD is a former Assistant Professor of Medicine at Tulane Medical School and a past Fellow of the American College of Cardiology. He is also a bar-certified attorney. He can be reached at televymd@yahoo.com. All his articles for the Orthomolecular Medicine News Service can be accessed at https://www.tomlevymd.com/health_ebytes.php.)
Note: To access any of the references below, type in the PMID number following the citation in the search box at this link: https://pubmed.ncbi.nlm.nih.gov/.
References
1. Pant K, Dutta U (2008) Understanding and management of male breast cancer: a critical review. Medical Oncology 25:294-298. PMID: 18074245
2. Katsura C, Ogunmwonyi I, Kankam H, Saha S (2022) Breast cancer: presentation, investigation and management. British Journal of Hospital Medicine 83:1-7. PMID: 35243878
3. Halliwell B (2006) Reactive species and antioxidants. Redox biology is a fundamental theme of aerobic life. Plant Physiology 141:312-322. PMID: 16760481
4. Sies H (2015) Oxidative stress: a concept in redox biology and medicine. Redox Biology 4:180-183. PMID: 25588755
5. Hu D, Li L, Li S et al. (2019) Lymphatic system identification, pathophysiology and therapy in the cardiovascular diseases. Journal of Molecular and Cellular Cardiology 133:99-111. PMID: 31181226
6. Breslin J, Yang Y, Scallan J et al. (2018) Lymphatic vessel network structure and physiology. Comprehensive Physiology 9:207-299
7. Willard-Mack C (2006) Normal structure, function, and histology of lymph nodes. Toxicologic Pathology 34:409-424. PMID: 17067937
8. Leong S, Pissas A, Scarato M et al. (2022) The lymphatic system and sentinel lymph nodes: conduit for cancer metastasis. Clinical & Experimental Metastasis 39:139-157. PMID: 34651243
9. Russell P, Hong J, Trevaskis N et al. (2022) Lymphatic contractile function: a comprehensive review of drug effects and potential clinical application. Cardiovascular Research 118:2437-2457. PMID: 34415332
10. Akita S, Nakamura R, Yamamoto N et al. (2016) Early detection of lymphatic disorder and treatment for lymphedema following breast cancer. Plastic and Reconstructive Surgery 138:192e-202e. PMID: 27465179
11. Horvath A, Redling M (2022) [Breast cancer-related lymphedema and treatment]. Article in Hungarian. Orvosi Hetilap 163:902-910. PMID: 35895575
12. DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphedema after breast cancer: a systemic review and meta-analysis. The Lancet: Oncology 14:500-515. PMID: 23540561
13. Brunelle C, Ag A (2022) The important role of nighttime compression in breast cancer-related lymphedema treatment. Cancer 128:458-460. PMID: 34614203
14. Blumgart E, Uren R, Nielsen P et al. (2011a) Lymphatic drainage and tumour prevalence in the breast: a statistical analysis of symmetry, gender and node field independence. Journal of Anatomy 218:652-659. PMID: 21453408
15. Tanis P, Nieweg O, Olmos R, Kroon B (2001) Anatomy and physiology of lymphatic drainage of the breast from the perspective of sentinel node biopsy. Journal of the American College of Surgeons 192:399-409. PMID: 11245383
16. Wisniewska K, Rybak Z, Szymonowicz M et al. (2021) Review on the lymphatic vessels in the dental pulp. Biology 10:1257. PMID: 34943171
17. Zhang Y, Ren X, Hu T et al. (2023) The relationship between periodontal disease and breast cancer: from basic mechanism to clinical management and prevention. Oral Health & Preventive Dentistry 21:49-60. PMID: 36794777
18. Mattila K, Pussinen P, Paju S (2005) Dental infections and cardiovascular diseases: a review. Journal of Periodontology 76:2085-2088. PMID: 16277580
19. Romandini M, Baima G, Antonoglou G et al. (2021) Periodontitis, edentulism, and risk of mortality: a systematic review with meta-analyses. Journal of Dental Research 100:37-49. PMID: 32866427
20. Larvin H, Kang J, Aggarwal V et al. (2021) Risk of incident cardiovascular disease in people with periodontal disease: a systematic review and meta-analysis. Clinical and Experimental Dental Research 7:109-122. PMID: 33124761
21. Franek E, Napora M, Blach A et al. (2010) Blood pressure and left ventricular mass in subjects with type 2 diabetes and gingivitis or chronic periodontitis. Journal of Clinical Periodontology 37:875-880. PMID: 20796107
22. Foratori-Junior G, Mascoli L, Marchese C et al. (2021) Association between arterial hypertension and periodontal status in morbidly obese patients who are candidates for bariatric surgery. International Dental Journal 71:242-249. PMID: 34024333
23. Pietropaoli D, Monaco A, D’Aiuto F et al. (2020) Active gingival inflammation is linked to hypertension. Journal of Hypertension 38:2018-2027. PMID: 32890278
24. Beck J, Philips K, Moss K et al. (2020) Periodontal disease classifications and incident coronary heart disease in the Atherosclerosis Risk in Communities study. Journal of Periodontology 91:1409-1418. PMID: 32449797
25. Byon M, Kim S, Kim J et al. (2020) Association of periodontitis with atherosclerotic cardiovascular diseases: a nationwide population-based retrospective matched cohort study. International Journal of Environmental Research and Public Health 17:7261. PMID: 33020434
26. Nikolaeva E, Tsarev V, Tsareva T et al. (2019) Interrelation of cardiovascular diseases with anaerobic bacteria of subgingival biofilm. Contemporary Clinical Dentistry 10:637-642. PMID: 32792823
27. Aoyama N, Kure K, Minabe M, Izumi Y (2019) Increased heart failure prevalence in patients with a high antibody level against periodontal pathogen. International Heart Journal 60:1142-1146. PMID: 31447467
28. Sandi R, Pol K, Basavaraj P et al. (2014) Association of serum cholesterol, triglyceride, high and low density lipoprotein (HDL and LDL) levels in chronic periodontitis subjects with risk for cardiovascular disease (CVD): a cross sectional study. Journal of Clinical and Diagnostic Research 8:214-216. PMID: 24596778
29. Gomes-Filho I, Balinha I, da Cruz S et al. (2021) Moderate and severe periodontitis are positively associated with metabolic syndrome. Clinical Oral Investigations 25:3719-3727. PMID: 33226499
30. Dewake N, Ishioka Y, Uchida K et al. (2020) Association between carotid artery calcification and periodontal disease progression in Japanese men and women: a cross-sectional study. Journal of Clinical Medicine 9:3365. PMID: 33092208
31. Heji E, Bukhari A, Bahammam M et al. (2021) Periodontal disease as a predictor of undiagnosed diabetes or prediabetes in dental patients. European Journal of Dentistry 15:216-221. PMID: 33285572
32. Quadri M, Fageeh H, Ibraheem W, Jessani A (2020) A case-control study of type 2 diabetes mellitus and periodontitis in Saudi Arabian adults. Journal of Multidisciplinary Healthcare 13:1741-1748. PMID: 33273822
33. Jimenez M, Krall E, Garcia R et al. (2009) Periodontitis and incidence of cerebrovascular disease in men. Annals of Neurology 66:505-512. PMID: 19847898
34. Slowik J, Wnuk M, Grzech K et al. (2010) Periodontitis affects neurological deficit in acute stroke. Journal of the Neurological Sciences 297:82-84. PMID: 20723913
35. Lafon A, Pereira B, Dufour T et al. (2014) Periodontal disease and stroke: a meta-analysis of cohort studies. European Journal of Neurology 21:1155-1161. PMID: 24712659
36. Palm F, Lahdentausta L, Sorsa T et al. (2014) Biomarkers of periodontitis and inflammation in ischemic stroke: a case-control study. Innate Immunity 20:511-518. PMID: 24045341
37. Lin H, Chen C, Yeh Y et al. (2019) Dental treatment procedures for periodontal disease and the subsequent risk of ischaemic stroke: a retrospective population-based cohort study. Journal of Clinical Periodontology 46:642-649. PMID: 30989681
38. Sen S, Mascari R (2020) Exploring the periodontal disease-ischemic stroke link. Journal of Periodontology 91:S35-S39. PMID: 32592499
39. Patel U, Malik P, Kodumuri N et al. (2020) Chronic periodontitis is associated with cerebral atherosclerosis-a nationwide study. Cureus 12:e11373. PMID: 33304705
40. Pyysalo M, Pyysalo L, Hiltunen J et al. (2018) The dental infections in patients undergoing preoperative dental examination before surgical treatment of saccular intracranial aneurysm. BMC Research Notes 11:600. PMID: 30126459
41. Hallikainen J, Keranen S, Savolainen J et al. (2021) Role of oral pathogens in the pathogenesis of intracranial aneurysm: review of existing evidence and potential mechanisms. Neurosurgical Review 44:239-247. PMID: 32034564
42. Takahashi M, Nakanishi Y, Hamada Y et al. (2020) A case of brain abscess caused by Actinomyces cardiffensis and Parvimonas micra. The Tokai Journal of Clinical and Experimental Medicine 45:189-194. PMID: 33300589
43. Leira Y, Ameijeira P, Dominguez C et al. (2020) Severe periodontitis is linked with increased peripheral levels of sTWEAK and PTX3 in chronic migraineurs. Clinical Oral Investigations 24:597-606. PMID: 31111284
44. Stein P, Steffen M, Smith C et al. (2012) Serum antibodies to periodontal pathogens are a risk factor for Alzheimer’s disease. Alzheimer’s & Dementia 8:196-203. PMID: 22546352
45. Sochocka M, Zwolinska K, Leszek J (2017) The infectious etiology of Alzheimer’s disease. Current Neuropharmacology 15:996-1009. PMID: 28294067
46. Botelho J, Mascarenhas P, Mendes J, Machado V (2020) Network protein interaction in Parkinson’s disease and periodontitis interplay: a preliminary bioinformatic analysis. Genes 11:1385. PMID: 33238395
47. Costa A, Yasuda C, Shibasaki W et al. (2014) The association between periodontal disease and seizure severity in refractory epilepsy patients. Seizure 23:227-230. PMID: 24456623
48. Aldosari M, Helmi M, Kennedy E et al. (2020) Depression, periodontitis, caries and missing teeth in the USA, NHANES 2009-2014. Family Medicine and Community Health 8:e000583. PMID: 33303491
49. Chang K, Hsu Y, Chiu I et al. (2020) Association between periodontitis and bipolar disorder: a nationwide cohort study. Medicine 99:e21423. PMID: 32756145
50. Tzeng N, Chung C, Yeh C et al. (2016) Are chronic periodontitis and gingivitis associated with dementia? A nationwide, retrospective, matched-cohort study in Taiwan. Neuroepidemiology 47:82-93. PMID: 27618156
51. Demmer R, Norby F, Lakshminarayan K et al. (2020) Periodontal disease and incident dementia: the Atherosclerosis Risk in Communities study (ARIC). Neurology 95:e1660-e1671. PMID: 32727837
52. Ding Y, Ren J, Yu H et al. (2018) Porphyromonas gingivalis, a periodontitis causing bacterium, induces memory impairment and age-dependent neuroinflammation in mice. Immunity & Ageing 15:6. PMID: 29422938
53. Manchery N, Henry J, Nangle M (2020) A systematic review of oral health in people with multiple sclerosis. Community Dentistry and Oral Epidemiology 48:89-100. PMID: 31815299
54. Dev Y, Goyal O (2013) Recurrent lung infection due to chronic periodontitis. Journal of the Indian Medical Association 111:127, 129. PMID: 24003573
55. Gomes-Filho I, de Oliveira T, da Cruz S et al. (2014) Influence of periodontitis in the development of nosocomial pneumonia: a case-control study. Journal of Periodontology 85:e82-e90. PMID: 24171504
56. Gomes-Filho I, Soledade-Marques K, da Cruz S et al. (2014) Does periodontal infection have an effect on severe asthma in adults? Journal of Periodontology 85:e179-e187. PMID: 24224961
57. Zhou X, Han J, Liu Z et al. (2014) Effects of periodontal treatment on lung function and exacerbation frequency in patients with chronic obstructive pulmonary disease and chronic periodontitis: a 2-year pilot randomized controlled trial. Journal of Clinical Periodontology 41:564-572. PMID: 24593836
58. Brasil-Oliveira R, Cruz A, Souza-Machado A et al. (2020) Oral health-related quality of life in individuals with severe asthma. Jornal Brasiliero de Pneumologia 47:e20200117. PMID: 33174972
59. Wee J, Yoo D, Byun S et al. (2020) Subjective oral health status in an adult Korean population with asthma or allergic rhinitis. Medicine 99:e22967. PMID: 33120860
60. Kim E, Choi Y (2018) Allergic rhinitis and periodontitis among Korean adults: results from a nationwide population-based study (2013-2015). BMC Ear, Nose, and Throat Disorders 18:12. PMID: 30116157
61. da Silva R, Caugant D, Eribe E et al. (2006) Bacterial diversity in aortic aneurysms determined by 16S ribosomal RNA gene analysis. Journal of Vascular Surgery 44:1055-1060. PMID: 17098542
62. Iwai T (2009) Periodontal bacteremia and various vascular diseases. Journal of Periodontal Research 44:689-694. PMID: 19874452
63. Gulati N, Masamatti S, Chopra P (2020) Association between obesity and its determinants with chronic periodontitis: a cross-sectional study. Journal of Indian Society of Periodontology 24:167-172. PMID: 32189846
64. Khan M, Alasqah M, Alammar L, Alkhaibari Y (2020) Obesity and periodontal disease: a review. Journal of Family Medicine and Primary Care 9:2650-2653. PMID: 32984101
65. She Y, Kong X, Ge Y et al. (2020) Periodontitis and inflammatory bowel disease: a meta-analysis. BMC Oral Health 20:67. PMID: 32164696
66. Tan C, Brand H, Kalender B et al. (2021) Dental and periodontal disease in patients with inflammatory bowel disease. Clinical Oral Investigations 25:5273-5280. PMID: 33619633
67. Zhang Y, Qiao D, Chen R et al. (2021) The association between periodontitis and inflammatory bowel disease: a systematic review and meta-analysis. BioMed Research International 2021:6692420. PMID: 33778080
68. Ogrendik M (2013) Rheumatoid arthritis is an autoimmune disease caused by periodontal pathogens. International Journal of General Medicine 6:383-386. PMID: 23737674
69. Gomez-Banuelos E, Mukherjee A, Darrah E, Andrade F (2019) Rheumatoid arthritis-associated mechanisms of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. Journal of Clinical Medicine 8:1309. PMID: 31454946
70. Pandey A, Rajak R, Pandey M (2021) Periodontal disease and its association with disease activity in ankylosing spondylitis/SpA: a systematic review. European Journal of Rheumatology 8:168-179. PMID: 33284102
71. Skeie M, Gil E, Cetrelli L et al. (2019) Oral health in children and adolescents with juvenile idiopathic arthritis-a systematic review and meta-analysis. BMC Oral Health 19:285. PMID: 31856793
72. Disale P, Zope S, Suragimath G et al. (2020) Prevalence and severity of periodontitis in patients with established rheumatoid arthritis and osteoarthritis. Journal of Family Medicine and Primary Care 9:2919-2925. PMID: 32984149
73. Xu S, Zhang G, Guo J, Tan Y (2021) Associations between osteoporosis and risk of periodontitis: a pooled analysis of observational studies. Oral Diseases 27:357-369. PMID: 32615008
74. Hickey N, Shalamanova L, Whitehead K et al. (2020) Exploring the putative interactions between chronic kidney disease and chronic periodontitis. Critical Reviews in Microbiology 46:61-77. PMID: 32046541
75. Schutz J, de Azambuja C, Cunha G et al. (2020) Association between severe periodontitis and chronic kidney disease severity in predialytic patients: a cross-sectional study. Oral Diseases 26:447-456. PMID: 31742816
76. Yue H, Xu X Liu Q et al. (2020) Effects of non-surgical periodontal therapy on systemic inflammation and metabolic markers in patients undergoing haemodialysis and/or peritoneal dialysis: a systematic review and meta-analysis. BMC Oral Health 20:18. PMID: 31969148
77. Mohammed H, Varoni E, Cochis A et al. (2018) Oral dysbiosis in pancreatic cancer and liver cirrhosis: a review of the literature. Biomedicines 6:115. PMID: 30544974
78. Gerlovin H, Michaud D, Cozier Y, Palmer J (2019) Oral health in relation to pancreatic cancer risk in African American women. Cancer Epidemiology, Biomarkers, & Prevention 28:675-679. PMID: 30923045
79. Wang J, Yang X, Zou X et al. (2020) Relationship between periodontal disease and lung cancer: a systematic review and meta-analysis. Journal of Periodontal Research 55:581-593. PMID: 32583879
80. Chen Y, Yang Y, Zhu B et al. (2020) Association between periodontal disease, tooth loss and liver diseases risk. Journal of Clinical Periodontology 47:1053-1063. PMID: 32621350
81. Di Spirito R, Toti P, Pilone V et al. (2020) The association between periodontitis and human colorectal cancer: genetic and pathogenic linkage. Life 10:211. PMID: 32962181
82. Xuan K, Jha A, Zhao T et al. (2021) Is periodontal disease associated with increased risk of colorectal cancer? A meta-analysis. International Journal of Dental Hygiene 19:50-61. PMID: 33269543
83. Kawasaki M, Ikeda Y, Ikeda E et al. (2021) Oral infectious bacteria in dental plaque and saliva as risk factors in patients with esophageal cancer. Cancer 127:512-519. PMID: 33156979
84. Velly A, Franco E, Schlecht N et al. (1998) Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncology 34:284-291. PMID: 9813724
85. Kageyama S, Takeshita T, Takeuchi K et al. (2019) Characteristics of the salivary microbiota in patients with various digestive tract cancers. Frontiers in Microbiology 10:1780. PMID: 31428073
86. Mathur R, Singhavi H, Malik A et al. (2019) Role of poor oral hygiene in causation of oral cancer-a review of literature. Indian Journal of Surgical Oncology 10:184-195. PMID: 30948897
87. Gopinath D, Menon R, Veettil S et al. (2020) Periodontal diseases as putative risk factors for head and neck cancer: systematic review and meta-analysis. Cancers 12:1893. PMID: 32674369
88. Payao S, Rasmussen L (2016) Helicobacter pylori and its reservoirs: a correlation with the gastric infection. World Journal of Gastrointestinal Pharmacology and Therapeutics 7:126-132. PMID: 26855818
89. Ma H, Zheng J, Li X (2020) Potential risk of certain cancers among patients with periodontitis: a supplementary meta-analysis of a large-scale population. International Journal of Medical Sciences 17:2531-2543. PMID: 33029095
90. Sun J, Tang Q, Yu S et al. (2020) Role of the oral microbiota in cancer evolution and progression. Cancer Medicine 9:6306-6321. PMID: 32638533
91. Malinowski B, Wesierska A, Zalewska K et al. (2019) The role of Tannerella forsythia and Porphyromonas gingivalis in pathogenesis of esophageal cancer. Infectious Agents and Cancer 14:3. PMID: 30728854
92. Marwaha A, Morris J, Rigby R (2020) Hypothesis: Bacterial induced inflammation disrupts the orderly progression of the stem cell hierarchy and has a role in the pathogenesis of breast cancer. Medical Hypotheses 136:109530. PMID: 31862686
93. Figuero E, Han Y, Furuichi Y (2000) Periodontal diseases and adverse pregnancy outcomes: mechanisms. Periodontology 83:175-188. PMID: 32385886
94. Heo J, Ahn K, Park J (2020) Radiological screening of maternal periodontitis for predicting adverse pregnancy and neonatal outcomes. Scientific Reports 10:21266. PMID: 33277556
95. Machado V, Lopes J, Patrao M et al. (2020) Validity of the association between periodontitis and female infertility conditions: a concise review. Reproduction 160:R41-R54. PMID: 32716008
96. Aldulaijan H, Cohen R, Stellrecht E et al. (2020) Relationship between hypothyroidism and periodontitis: a scoping review. Clinical and Experimental Dental Research 6:147-157. PMID: 32067402
97. Kothiwale S, Desai B, Kothiwale V et al. (2014) Periodontal disease as a potential risk factor for low birth weight and reduced maternal haemoglobin levels. Oral Health & Preventive Dentistry 12:83-90. PMID: 24619787
98. Wu D, Lin Z, Zhang S et al. (2020) Decreased hemoglobin concentration and iron metabolism disorder in periodontitis: systematic review and meta-analysis. Frontiers in Physiology 10:1620. PMID: 32082180
99. Chau S, Lee C, Huang J et al. (2020) The existence of periodontal disease and subsequent ocular diseases: a population-based cohort study. Medicina 56:621. PMID: 33218003
100. Sun K, Shen T, Chen S et al. (2020) Periodontitis and the subsequent risk of glaucoma: results from the real-world practice. Scientific Reports 10:17568. PMID: 33067540
101. Antal M, Braunitzer G, Mattheos N et al. (2014) Smoking as a permissive factor of periodontal disease in psoriasis. PLoS One 9:e92333. PMID: 24651659
102. Zhang X, Gu H, Xie S, Su Y (2022) Periodontitis in patients with psoriasis: a systematic review and meta-analysis. Oral Diseases 28:33-43. PMID: 32852860
103. Nijakowski K, Gruszczynski D, Kolasinska J et al. (2022) Periodontal disease in patients with psoriasis: a systematic review. International Journal of Environmental Research and Public Health 19:11302. PMID: 36141573
104. Costa A, Cota L, Mendes V et al. (2021) Periodontitis and the impact of oral health on the quality of life of psoriatic individuals: a case-control study. Clinical Oral Investigations 25:2827-2836. PMID: 32955692
105. Bhadauria U, Purohit B, Agarwal D et al. (2023) Oral hygiene status in individuals with hearing difficulties: a systematic review and meta-analysis. Special Care in Dentistry Mar 6. Online ahead of print. PMID: 36880182
106. Wu C, Yang T, Lin H et al. (2013) Sudden sensorineural hearing loss associated with chronic periodontitis: a population-based study. Otology & Neurotology 34:1380-1384. PMID: 24026022
107. Huang F, Luo C, Lee S et al. (2023) Relationship between periodontal disease and dizziness in Taiwanese adults: a nationwide population-based cohort study. Medicine 102:e32961. PMID: 36827024
108. Young H, Ward W (2021) The relationship between polycystic ovarian syndrome, periodontal disease, and osteoporosis. Reproductive Sciences 28:950-962. PMID: 32914348
109. Degasperi G, Ossick M, Pinheiro S, Etchegaray A (2020) Autoimmunity and periodontal disease: arguing a possible correlation. Indian Journal of Dental Research 31:615-620. PMID: 33107465
110. Benli M, Batool F, Stutz C et al. (2021) Orofacial manifestations and dental management of systemic lupus erythematosus: a review. Oral Diseases 27:151-167. PMID: 31886584
111. Pessoa L, Aleti G, Choudhury S et al. (2019) Host-microbial interactions in systemic lupus erythematosus and periodontitis. Frontiers in Immunology 10:2602. PMID: 31781106
112. Lee J, Jeong S (2020) A population-based study on the association between periodontal disease and major lifestyle-related comorbidities in South Korea: an elderly cohort study from 2002-2015. Medicina 56:575. PMID: 33138320
113. Gupta S, Suri P, Patil P et al. (2020) Comparative evaluation of role of hs C-reactive protein as a diagnostic marker in chronic periodontitis patients. Journal of Family Medicine and Primary Care 9:1340-1347. PMID: 32509613
114. Esteves-Lima R, Reis C, Santirocchi-Junior F et al. (2020) Association between periodontitis and serum C-reactive protein levels. Journal of Clinical and Experimental Dentistry 12:e838-e843. PMID: 32994872
115. Costa F, Lima R, Cortelli S et al. (2021) Effect of compliance during periodontal maintenance therapy on C-reactive protein levels: a 6-year follow-up. Journal of Clinical Periodontology 48:400-409. PMID: 33259118
116. Isola G, Polizzi A, Muraglie S et al. (2019) Assessment of vitamin C and antioxidant profiles in saliva and serum in patients with periodontitis and ischemic heart disease. Nutrients 11:2956. PMID: 31817129
117. Olszewska-Czyz I, Firkova E (2022) Vitamin D3 serum levels in periodontitis patients: a case-control study. Medicina 58:585. PMID: 35630002
118. Isola G. Alibrandi A, Rapisarda E et al. (2020) Association of vitamin D in patients with periodontitis: a cross-sectional study. Journal of Periodontal Research 55:602-612. PMID: 32173876
119. Munday M, Rodricks R, Fitzpatrick M et al. (2020) A pilot study examining vitamin C levels in periodontal patients. Nutrients 12:2255. PMID: 32731485
120. Gupta V, Mishra S, Gazala M et al. (2022) Serum vitamin D level and its association with red blood cell indices in patients with periodontitis. Journal of Indian Society of Periodontology 26:446-450. PMID: 36339383
121. Botelho J, Machado V, Proenca L et al. (2020) Vitamin D deficiency and oral health: a comprehensive review. Nutrients 12:1471. PMID: 32438644
122. Tada A, Miura H (2019) The relationship between vitamin C and periodontal diseases: a systematic review. International Journal of Environmental Research and Public Health 16:2472. PMID: 31336735
123. Debelian G, Olsen I, Tronstad L (1995) Bacteremia in conjunction with endodontic therapy. Endodontics & Dental Traumatology 11:142-149. PMID: 7641631
124. Savarrio L, Mackenzie D, Riggio M et al. (2005) Detection of bacteraemias during non-surgical root canal treatment. Journal of Dentistry 33:293-303. PMID: 15781137
125. Caplan D (2014) Chronic apical periodontitis is more common in subjects with coronary artery disease. The Journal of Evidence-Based Dental Practice 14:149-150. PMID: 25234220
126. Costa T, Neto J, de Oliveira A et al. (2014) Association between chronic apical periodontitis and coronary artery disease. Journal of Endodontics 40:164-167. PMID: 24461397
127. Petersen J, Glabl E, Nasseri P et al. (2014) The association of chronic apical periodontitis and endodontic therapy with atherosclerosis. Clinical Oral Investigations 18:1813-1823. PMID: 24338091
128. Liljestrand J, Mantyla P, Paju S et al. (2016) Association of endodontic lesions with coronary artery disease. Journal of Dental Research 95:1358-1365. PMID: 27466397
129. Garrido M, Cardenas A, Astorga J et al. (2019) Elevated systemic inflammatory burden and cardiovascular risk in young adults with endodontic apical lesions. Journal of Endodontics 45:111-115. PMID: 30711165
130. Sobieszczanski J, Mertowski S, Sarna-Bos K et al. (2023) Root canal infection and its impact on the oral cavity microenvironment in the context of immune system disorders in selected diseases: a narrative review. Journal of Clinical Medicine 12:4102. PMID: 37373794
131. Takahashi M, Segoe H, Kikuiri T et al. (2022) A rare case of multiple brain abscesses caused by apical periodontitis of deciduous teeth in congenital heart disease: a case report. BMC Oral Health 22:261. PMID: 35765049
132. Leao T, Tomasi G, Conzatti L et al. (2022) Oral inflammatory burden and carotid atherosclerosis among stroke patients. Journal of Endodontics 48:597-605. PMID: 35143813
133. Grau A, Buggle F, Ziegler C et al. (1997) Association between acute cerebrovascular ischemia and chronic and recurrent infection. Stroke 28:1724-1729. PMID: 9303015
134. Villalobos V, Garrido M, Reyes A et al. (2022) Aging envisage imbalance of the periodontium: a keystone in oral disease and systemic health. Frontiers in Immunology 13:1044334. PMID: 36341447
135. Reyes A, Ramcharan K Maharaj R (2019) Chronic migraine headache and multiple dental pathologies causing cranial pain for 35 years: the neurodental nexus. BMJ Case Reports 12:e230248. PMID: 31540922
136. Gomes C, Martinho F, Barbosa D et al. (2018) Increased root canal endotoxin levels are associated with chronic apical periodontitis, increased oxidative and nitrosative stress, major depression, severity of depression, and a lowered quality of life. Molecular Neurobiology 55:2814-2827. PMID: 28455694
137. Rotstein I, Katz J (2022) Periapical disease in post-stroke patients. American Journal of Dentistry 35:197-199. PMID: 35986935
138. Xiang W, Wei H, Xu L, Liang Z (2022) Orbital apex syndrome secondary to apical periodontitis of a tooth: a case report. BMC Neurology 22:354. PMID: 36123630
139. Piras V, Usai P, Mezzena S et al. (2017) Prevalence of apical periodontitis in patients with inflammatory bowel diseases: a retrospective clinical study. Journal of Endodontics 43:389-394. PMID: 28231978
140. Poyato-Borrego M, Segura-Sampedro J, Martin-Gonzalez et al. (2020) High prevalence of apical periodontitis in patients with inflammatory bowel disease: an age- and gender-matched case-control study. Inflammatory Bowel Disease 26:273-279. PMID: 31247107
141. Segura-Sampedro J, Jimenez-Gimenez C, Jane-Salas E et al. (2022) Periapical and endodontic status of patients with inflammatory bowel disease: age- and sex-matched case-control study. International Endodontic Journal 55:748-757. PMID: 35403728
142. Poyato-Borrego M, Segura-Egea J, Martin-Gonzalez J et al. (2021) Prevalence of endodontic infection in patients with Crohn’s disease and ulcerative colitis. Medicina Oral, Patologia Oral y Cirugia Bucal 26:e208-e215. PMID: 32851982
143. Budreikaite K, Varoneckaite M, Oleinikaite D, Zilinskas J (2022) Association between apical periodontitis and root canal treatment in patients with type II diabetes. A systematic review. Stomotologija 24:100-103. PMID: 37154421
144. Castellanos-Cosano L, Machuca-Portillo G, Segura-Sampedro J et al. (2013) Prevalence of apical periodontitis and frequency of root canal treatments in liver transplant candidates. Medicina Oral, Patologia Oral y Cirugia Bucal 18:e773-e779. PMID: 23722148
145. Gronkjaer L, Holmstrup P, Schou S et al. (2016) Presence and consequence of tooth periapical radiolucency in patients with cirrhosis. Hepatic Medicine: Evidence and Research 8:97-103. PMID: 27695370
146. Khalighinejad N, Aminoshariae A, Kulild J et al. (2017) Association of end-stage renal disease with radiographically and clinically diagnosed apical periodontitis: a hospital-based study. Journal of Endodontics 43:1438-1441. PMID: 28712633
147. Buhlin K, Barany P, Heimburger O et al. (2007) Oral health and pro-inflammatory status in end-stage renal disease patients. Oral Health & Preventive Dentistry 5:235-244. PMID: 17977296
148. Karatas E, Kul A, Camilleri J, Yonel Z (2023) Association between rheumatoid arthritis and pulpal-periapical pathology: a systematic review. Clinical Oral Investigations Oct 12. Online ahead of print. PMID: 37828236
149. Karatas E, Kul A, Tepecik E (2020) Association of ankylosing spondylitis with radiographically and clinically diagnosed apical periodontitis: a cross-sectional study. Dental and Medical Problems 57:171-175. PMID: 32104993
150. Karatas E, Kul A, Tepecik E (2020) Association between rheumatoid arthritis and apical periodontitis: a cross-sectional study. European Endodontic Journal 5:155-158. PMID: 32766528
151. Lopez-Lopez J, Castellanos-Cosano L, Estrugo-Devesa A et al. (2015) Radiolucent periapical lesions and bone mineral density in post-menopausal women. Gerodontology 32:195-201. PMID: 24164489
152. Katz J, Rotstein I (2021) Prevalence of periapical lesions in patients with osteoporosis. Journal of Endodontics 47:234-238. PMID: 33130060
153. Allihaibi M, Niazi S, Farzadi S et al. (2023) Prevalence of apical periodontitis in patients with autoimmune diseases: a case-control study. International Endodontic Journal 56:573-583. PMID: 36747086
154. Dolan S, Rae E (2023) Apical periodontitis and autoimmune diseases-should we be screening patients prior to therapy? Evidence-Based Dentistry 24:64-65. PMID: 37173517
155. Harjunmaa L, Jarnstedt J, Alho L et al. (2015) Association between maternal dental periapical infections and pregnancy outcomes: results from a cross-sectional study in Malawi. Tropical Medicine & International Health 20:1549-1558. PMID: 26224026
156. Leal A, de Oliveira A, Brito L et al. (2015) Association between chronic apical periodontitis and low-birth-weight preterm births. Journal of Endodontics 41:353-357. PMID: 25576210
157. Bakhsh A, Moyes D, Proctor G et al. (2022) The impact of apical periodontitis, non-surgical root canal retreatment and periapical surgery on serum inflammatory biomarkers. International Endodontic Journal 55:923-937. PMID: 35707939
158. Sathyanarayanan K, Ranjana N, Bhavana M et al. (2023) Asymptomatic apical periodontitis lesions and their association with systemic inflammatory burden: a preliminary prospective clinical study. Cureus 15:e46357. PMID: 37920638
159. Sirin D, Ozcelik F (2021) The relationship between COVID-19 and the dental damage stage determined by radiological examination. Oral Radiology 37:600-609. PMID: 33389600
160. Braz-Silva P, Bergamini M, Mardegan A et al. (2019) Inflammatory profile of chronic apical periodontitis: a literature review. Acta Odontologia Scandinavica 77:173-180. PMID: 30585523
161. Gomes B, Herrera D (2018) Etiologic role of root canal infection in apical periodontitis and its relationship with clinical symptomatology. Brazilian Oral Research 32:e69. PMID: 30365610
162. Yazdi K, Sabeti M, Jabalameli F et al. (2008) Relationship between human cytomegalovirus transcription and symptomatic apical periodontitis in Iran. Oral Microbiology and Immunology 23:510-514. PMID: 18954359
163. Hernadi K, Szalmas A, Mogyorosi R et al. (2012) [The prevalence of herpesviruses in human apical periodontitis samples]. Article in Hungarian. Fogorvosi Szemle 105:135-140. PMID: 23387127
164. Ozbek S, Ozbek A, Yavuz M (2013) Detection of human cytomegalovirus and Epstein-Barr virus in symptomatic and asymptomatic apical periodontitis lesions by real-time PCR. Medicina Oral, Patologia Oral y Cirugia Bucal 18:e811-e816. PMID: 23722135
165. Waltimo T, Siren E, Torkko H et al. (1997) Fungi in therapy-resistant apical periodontitis. International Endodontic Journal 30:96-101. PMID: 10332243
166. Peciuliene V, Reynaud A, Balciuniene I, Haapasalo M (2001) Isolation of yeasts and enteric bacteria in root-filled teeth with chronic apical periodontitis. International Endodontic Journal 34:429-434. PMID: 11556508
167. Sirin D, Ozcelik F, Uzun C et al. (2019) Association between C-reactive protein, neutrophil to lymphocyte ratio and the burden of apical periodontitis: a case-controlled study. Acta Odontologica Scandinavica 77:142-149. PMID: 30394169
168. Hoppe C, Oliveira J, Grecca F et al. (2017) Association between chronic oral inflammatory burden and physical fitness in males: a cross-sectional observational study. International Endodontic Journal 50:740-749. PMID: 27578486
169. Ye L, Cao L, Song W et al. (2023) Interaction between apical periodontitis and systemic disease (review). International Journal of Molecular Medicine 52:60. PMID: 37264964
170. Blumgart E, Uren R. Nielsen P et al. (2011) Predicting lymphatic drainage patterns and primary tumour location in patients with breast cancer. Breast Cancer Research and Treatment 130:699-705. PMID: 21850393
171. Desouki M (2015) Reduction mammoplasty is beneficial in women with and without history of breast cancer. Women’s Health 11:419-422. PMID: 26245153
172. Ingram D, Huang H, Catchpole B, Roberts A (1989) Do big breasts disadvantage women with breast cancer? The Australian and New Zealand Journal of Surgery 59:115-117. PMID: 2919995
173. Leon-Lopez M, Cabanillas-Balsera D, Martin-Gonzalez J et al. (2022) Prevalence of root canal treatment worldwide: a systematic review and meta-analysis. International Endodontic Journal 55:1105-1127. PMID: 36016509
174. Tiburcio-Machado C, Michelon C, Zanatta F et al. (2021) The global prevalence of apical periodontitis: a systematic review and meta-analysis. International Endodontic Journal 54:712-735. PMID: 33378579
175. Ahmed I, Ali R, Mudawi A (2017) Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Sudanese population. Clinical and Experimental Dental Research 3:142-147. PMID: 29744192
176. Van der Veken D, Curvers F, Fieuws S, Lambrechts P (2017) Prevalence of apical periodontitis and root filled teeth in a Belgian subpopulation found on CBCT images. International Endodontic Journal 50:317-329. PMID: 26992464
177. Mashyakhy M, Alkahtany M (2021) Prevalence of apical periodontitis between root canal-treated and non-treated teeth and between genders: a cross-sectional CBCT study. Nigerian Journal of Clinical Practice 24:1656-1661. PMID: 34782505
178. Chala S, Abouqal R, Abdallaoui F (2011) Prevalence of apical periodontitis and factors associated with the periradicular status. Acta Odontologica Scandinavica 69:355-359. PMID: 21426267
179. Jimenez-Pinzon A, Segura-Egea J, Poyato-Ferrera M, et al. (2004) Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. International Endodontic Journal 37:167-173. PMID: 15009405
180. Jakovljevic A, Aminoshariae A (2022) Limited evidence shows a high global burden of apical periodontitis among adults worldwide. The Journal of Evidence-Based Dental Practice 22:101667. PMID: 35219461
181. Segura-Egea J, Martin-Gonzalez J, Castellanos-Cosano L (2015) Endodontic medicine: connections between apical periodontitis and systemic diseases. International Endodontic Journal 48:933-951. PMID: 26174809
182. Al-Qudah A, Jawad D, Jaradat M (2023) Periapical status of non-root-filled teeth with amalgam, composite, or crown restorations: a cross-sectional study. International Dental Journal 73:645-650. PMID: 36543731
183. Siqueira Jr J, Rocas I (2009) Diversity of endodontic microbiota revisited. Journal of Dental Research 88:969-981. PMID: 19828883
184. Suprewicz L, Tokajuk G, Ciesluk M et al. (2020) Bacteria residing at root canals can induce cell proliferation and alter the mechanical properties of gingival and cancer cells. International Journal of Molecular Sciences 21:7914. PMID: 33114460
185. Kulacz R, Levy T (2014) The Toxic Tooth: How a root canal could be making you sick. Henderson, NV: MedFox Publishing
186. Lechner J, Schick F (2021) Chronic fatigue syndrome and bone marrow defects of the jaw-a case report on additional dental X-ray diagnostics with ultrasound. International Medical Case Reports Journal 14:241-249. PMID: 33907473
187. Lechner J, Schmidt M, von Baehr V, Schick F (2021) Undetected jawbone marrow defects as inflammatory and degenerative signaling pathways: chemokine RANTES/CCL5 as a possible link between the jawbone and systemic interactions? Journal of Inflammation Research 14:1603-1612. PMID: 33911892
188. Lechner J, Schulz T, Lejeune B, von Baehr V (2021) Jawbone cavitation expressed RANTES/CCL5: case studies linking silent inflammation in the jawbone with epistemology of breast cancer. Breast Cancer 13:225-240. PMID: 33859496
189. Lechner J, von Baehr V, Schick F (2021) RANTES/CCL5 signaling from jawbone cavitations to epistemology of multiple sclerosis-research and case studies. Degenerative Neurological and Neuromuscular Disease 11:41-50. PMID: 34262389
190. Zhang Y, Liu X, Yang R (2023) Diagnosis and treatment of apical cyst of deciduous teeth with infection: a case report. West China Journal of Stomatology 41:356-360. PMID: 37277803
191. Parhi L, Alon-Maimon T, Sol A et al. (2020) Breast cancer colonization by Fusobacterium nucleatum accelerates tumor growth and metastatic progression. Nature Communities 11:3259. PMID: 32591509
192. Van der Merwe M, Niekerk G, Botha A, Engelbrecht A (2021) The onco-immunological implications of Fusobacterium nucleatum in breast cancer. Immunology Letters 232:60-66. PMID: 33647328
193. Fu A, Yao B, Dong T et al. (2022) Tumor-resident intracellular microbiota promotes metastatic colonization in breast cancer. Cell 185:1356-1372. PMID: 35395179
194. Zheng H, Du C, Yu C et al. (2022) The relationship of tumor microbiome and oral bacteria and intestinal dysbiosis in canine mammary tumor. International Journal of Molecular Sciences 23:10928. PMID: 36142841
195. Lawson J, Glenn W, Whitaker N (2010) Breast cancer as an infectious disease. Women’s Health 6:5-8. PMID: 20088725
196. Thompson K, Ingle J, Tang X et al. (2017) A comprehensive analysis of breast cancer microbiota and host gene expression. PLoS One 12:e0188873. PMID: 29190829
197. Khodabandehlou N, Mostafaei S, Etermadi A et al. (2019) Human papilloma virus and breast cancer: the role of inflammation and viral expressed proteins. BMC Cancer 19:61. PMID: 30642295
198. Lehrer S, Rheinstein P (2019) The virology of breast cancer: viruses as the potential causative agents of breast tumorigenesis. Discovery Medicine 27:163-166. PMID: 31095925
199. O’Connor H, MacSharry J, Bueso Y et al. (2018) Resident bacteria in breast cancer tissue: pathogenic agents or harmless commensals? Discovery Medicine 26:93-102. PMID: 30399327
200. Tzeng A, Sangwan N, Jia M et al. (2021) Human breast microbiome correlates with prognostic features and immunological signatures in breast cancer. Genome Medicine 13:60. PMID: 33863341
201. Urbaniak C, Gloor G, Brackstone M et al. (2016) The microbiota of breast tissue and its association with breast cancer. Applied and Environmental Microbiology 82:5039-5048. PMID: 27342554
202. Douglas P (2021) Overdiagnosis and overtreatment of nipple and breast candidiasis: a review of the relationship between diagnoses of mammary candidiasis and Candida albicans in breastfeeding women. Women’s Health 17:17455065211031480. PMID: 34269140
203. Toumazi D, Daccache S, Constantinou C (2021) An unexpected link: the role of mammary and gut microbiota on breast cancer development and management (review). Oncology Reports 45:80. PMID: 33786630
204. Chen J, Douglass J, Prasath V et al. (2019) The microbiome and breast cancer: a review. Breast Cancer Research and Treatment 178:493-496. PMID: 31456069
205. Bartsich S, Ascherman J, Whittier S et al. (2011) The breast: a clean-contaminated surgical site. Aesthetic Surgery Journal 31:802-806. PMID: 21908811
206. Chattopadhyay I, Verma M, Panda M (2019) Role of oral microbiome signatures in diagnosis and prognosis of oral cancer. Technology in Cancer Research & Treatment 18:1533033819867354. PMID: 31370775
207. Hussein A, Salih N, Saadoon I (2021) Effect of microbiota in the development of breast cancer. Archives of Razi Institute 76:761-768. PMID: 35096312
208. Xuan C, Shamonki J, Chung A et al. (2014) Microbial dysbiosis is associated with human breast cancer. PLoS One 9:e83744. PMID: 24421902
209. Thu M, Chotirosniramit K, Nopsopon T et al. (2023) Human gut, breast, and oral microbiome in breast cancer: a systematic review and meta-analysis. Frontiers in Oncology 13:1144021. PMID: 37007104
210. Levy T (2021) Rapid Virus Recovery: No need to live in fear! Henderson, NV: MedFox Publishing. [Free eBook download available at https://rvr.medfoxpub.com/]
211. Dominy S, Lynch C, Ermini F et al. (2019) Porphyomonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Science Advances 5:eaau3333. PMID: 30746447
212. Dioguardi M, Crincoli V, Laino L et al. (2020) The role of periodontitis and periodontal bacteria in the onset and progression of Alzheimer’s disease: a systematic review. Journal of Clinical Medicine 9:495. PMID: 32054121
213. Laugisch O, Johnen A, Maldonado A et al. (2018) Periodontal pathogens and associated intrathecal antibodies in early stages of Alzheimer’s disease. Journal of Alzheimer’s Disease 66:105-114. PMID: 30223397
214. Balin B, Gerard H, Arking E et al. (1998) Identification and localization of Chlamydia pneumoniae in the Alzheimer’s brain. Medical Microbiology and Immunology 187:23-42. PMID: 9749980
215. Miklossy J, Khalili K, Gern L et al. (2004) Borrelia burgdorferi persists in the brain in chronic Lyme neuroborreliosis and may be associated with Alzheimer’s disease. Journal of Alzheimer’s Disease 6:639-649. PMID: 15665404
216. Wozniak M, Mee A, Itzhaki R (2009) Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. The Journal of Pathology 217:131-138. PMID: 18973185
217. Wan J, Fan H (2023) Oral microbiome and Alzheimer’s disease. Microorganisms 11:2550. PMID: 37894208
218. Alonso R, Pisa D, Marina A et al. (2014) Fungal infection in patients with Alzheimer’s disease. Journal of Alzheimer’s Disease 41:301-311. PMID: 24614898
219. Adams B, Nunes J, Page M et al. (2019) Parkinson’s disease: a systemic inflammatory disease accompanied by bacterial inflammagens. Frontiers in Aging Neuroscience 11:210. PMID: 31507404
220. Alonso R, Fernandez-Fernandez A, Pisa D, Carrasco (2018) Multiple sclerosis and mixed microbial infections. Direct identification of fungi and bacteria in nervous tissue. Neurobiology of Disease 117:42-61. PMID: 29859870
221. Pisa D, Alonso R, Jimenez-Jimenez F, Carrasco L (2013) Fungal infection in cerebrospinal fluid from some patients with multiple sclerosis. European Journal of Clinical Microbiology & Infectious Diseases 32:795-801. PMID: 23322279
222. Alonso R, Pisa D, Marina A et al. (2015) Evidence for fungal infection in cerebrospinal fluid and brain tissue from patients with amyotrophic lateral sclerosis. International Journal of Biological Sciences 11:546-558. PMID: 25892962
223. Ott S, El Mokhtari N, Musfeldt M et al. (2006) Detection of diverse bacterial signatures in atherosclerotic lesions of patients with coronary heart disease. Circulation 113:929-937. PMID: 16490835
224. Zaremba M, Gorska R, Suwalski P, Kowalski J (2007) Evaluation of the incidence of periodontitis-associated bacteria in the atherosclerotic plaque of coronary blood vessels. Journal of Periodontology 78:322-327. PMID: 17274722
225. Mahendra J, Mahendra L, Kurian V et al. (2010) 16S rRNA-based detection of oral pathogens in coronary atherosclerotic plaque. Indian Journal of Dental Research 21:248-252. PMID: 20657096
226. Haraszthy V, Zambon J, Trevisan M et al. (2000) Identification of periodontal pathogens in atheromatous plaques. Journal of Periodontology 71:1554-1560. PMID: 11063387
227. Pyysalo M, Pyysalo L, Pessi T et al. (2016) Bacterial DNA findings in ruptured and unruptured intracranial aneurysms. Acta Odontologica Scandinavica 74:315-320. PMID: 26777430
228. Kurihara N, Inoue Y, Iwai T et al. (2004) Detection and localization of periodontopathic bacteria in abdominal aortic aneurysms. European Journal of Vascular and Endovascular Surgery 28:553-558. PMID: 15465379
229. Pessi T, Karhunen V, Karjalainen P et al. (2013) Bacterial signatures in thrombus aspirates of patients with myocardial infarction. Circulation 127:1219-1228. PMID: 23418311
230. Pinon-Esteban P, Nunez L, Moure R et al. (2020) Presence of bacterial DNA in thrombotic material of patients with myocardial infarction. Scientific Reports 10:16299. PMID: 33004892
231. Vakhitov D, Tuomisto S, Martiskainen M et al. (2018) Bacterial signatures in thrombus aspirates of patients with lower limb arterial and venous thrombosis. Journal of Vascular Surgery 67:1902-1907. PMID: 28847664
232. Louhelainen A, Aho J, Tuomisto S et al. (2014) Oral bacterial DNA findings in pericardial fluid. Journal of Oral Microbiology 6:25835. PMID: 25412607
233. Reichert S, Haffner M, Keyber G et al. (2013) Detection of oral bacterial DNA in synovial fluid. Journal of Clinical Periodontology 40:591-598. PMID: 23534379
234. Totaro M, Cattani P, Ria F et al. (2013) Porphyromonas gingivalis and the pathogenesis of rheumatoid arthritis: analysis of various compartments including the synovial tissue. Arthritis Research & Therapy 15:R66. PMID: 23777892
235. Du Q, Ma X (2020) [Research progress of correlation between periodontal pathogens and systemic diseases]. Article in Chinese. Journal of Southern Medical University 40:759-764. PMID: 32897213
236. Ye C, Katagiri S, Miyasaka N et al. (2020) The periodontopathic bacteria in placenta, saliva and subgingival plaque of threatened preterm labor and preterm low birth weight cases: a longitudinal study in Japanese pregnant women. Clinical Oral Investigations 24:4261-4270. PMID: 32333174
237. Fisher L, Demerath E, Bittner-Eddy P, Costalonga M (2019) Placental colonization with periodontal pathogens: the potential missing link. American Journal of Obstetrics and Gynecology 221:383-392. PMID: 31051120
238. Figueredo C, Sete M, Carlos J et al. (2018) Presence of anti-Porphyromonas gingivalis-peptidylarginine deiminase antibodies in serum from juvenile systemic lupus erythematosus patients. Acta Reumatologica Portuguesa 43:239-240. PMID: 30414375
239. Bagavant H, Dunkleberger M, Wolska N et al. (2019) Antibodies to periodontogenic bacteria are associated with higher disease activity in lupus patients. Clinical and Experimental Rheumatology 37:106-111. PMID: 29998833
240. Aoki S, Hosomi N, Nishi H et al. (2020) Serum IgG titers to periodontal pathogens predict 3-month outcome in ischemic stroke patients. PLoS One 15:e0237185. PMID: 32760103
241. Pillai R, Iyer K, Spin-Neto R et al. (2018) Oral health and brain injury: causal or casual relation? Cerebrovascular Diseases Extra 8:1-15. PMID: 29402871
242. Heiken T, Chen J, Hoskin T et al. (2016) The microbiome of aseptically collected human breast tissue in benign and malignant disease. Scientific Reports 6:30751. PMID: 27485780
243. Gaba F, Gonzalez R, Martinez R (2022) The role of oral Fusobacterium nucleatum in female breast cancer: a systematic review and meta-analysis. International Journal of Dentistry 2022:1876275. PMID: 36466367
244. Desalegn Z, Smith A, Yohannes M et al. (2023) Human breast tissue microbiota reveals unique microbial signatures that correlate with prognostic features in adult Ethiopian women with breast cancer. Cancers 15:4893. PMID: 37835588
245. Park D, Woo B, Lee B et al. (2019) Serum levels of interleukin-6 and titers of antibodies against Porphyromonas gingivalis could be potential biomarkers for the diagnosis of oral squamous cell carcinoma. International Journal of Molecular Sciences 20:2749. PMID: 31167516
246. Zhou Y, Luo G (2019) Porphyromonas gingivalis and digestive system cancers. World Journal of Clinical Care 7:819-829. PMID: 31024953
247. He Z, Tian W, Wei Q, Xu J (2022) Involvement of Fusobacterium nucleatum in malignancies except for colorectal cancer: a literature review. Frontiers in Immunology 13:968649. PMID: 36059542
248. Yamamura K, Baba Y, Nakagawa S et al. (2016) Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clinical Cancer Research 22:5574-5581. PMID: 27769987
249. Kosumi K, Baba Y, Yamamura K et al. (2023) Intratumour Fusobacterium nucleatum and immune response to oesophageal cancer. British Journal of Cancer 128:1155-1165. PMID: 36599917
250. Nagasaki A, Sakamoto S, Arai T et al. (2021) Elimination of Porphyromonas gingivalis inhibits liver fibrosis and inflammation in NASH. Journal of Clinical Periodontology 48:1367-1378. PMID: 34250613
251. Chen Y, Wei J (2015) Identification of pathogen signatures in prostate cancer using RNA-seq. PLoS One 10:e0128955. PMID: 26053031
252. Udayasuryan B, Ahmad R, Nguyen T et al. (2022) Fusobacterium nucleatum induces proliferation and migration in pancreatic cancer cells through host autocrine and paracrine signaling. Science Signaling 15:eabn4948. PMID: 36256708
253. Tan Q, Ma X, Yang B et al. (2022) Periodontitis pathogen Porphyromonas gingivalis promotes pancreatic tumorigenesis via neutrophil elastase from tumor-associated neutrophils. Gut Microbes 14:2073785
254. Pignatelli P, Nuccio F, Piattelli A, Curia M (2023) The role of Fusobacterium nucleatum in oral and colorectal carcinogenesis. Microorganisms 11:2358. PMID: 37764202
255. Wang N, Fang J (2023) Fusobacterium nucleatum, a key pathogenic factor and microbial biomarker for colorectal cancer. Trends in Microbiology 31:159-172. PMID: 36058786
256. Fiorillo L, Cervino G, Laino L et al. (2019) Porphyromonas gingivalis, periodontal and systemic implications: a systematic review. Dentistry Journal 7:114. PMID: 31835888
257. Mei F, Xie M, Huang X et al. (2020) Porphyromonos gingivalis and its systemic impact: current status. Pathogens 9:944. PMID: 33202751
258. Fan Z, Tang P, Li C et al. (2022) Fusobacterium nucleatum and its associated systemic diseases: epidemiologic studies and possible mechanisms. Journal of Oral Microbiology 15:2145729. PMID: 36407281
259. Issels J (1999) Cancer, A Second Opinion: The classic book on integrative cancer treatment. Garden City Park, NY: Avery Publishing Group
260. Levy T (2017) Hidden Epidemic: Silent oral infections cause most heart attacks and breast cancers. Henderson, NV: MedFox Publishing [Free eBook download available at http://www.hep21.medfoxpub.com]
261. Kaasalainen T, Ekholm M, Siiskonen T, Kortesniemi M (2021) Dental cone beam CT: an updated review. Physica Medica 88:193-217. PMID: 34284332
262. Levy T, Hunninghake R (2023) http://orthomolecular.org/resources/omns/v18n24.shtml
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org
Find a Doctor
To locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource.
Editorial Review Board:
Albert G. B. Amoa, MB.Ch.B, Ph.D. (Ghana)
Seth Ayettey, M.B., Ch.B., Ph.D. (Ghana)
Ilyès Baghli, M.D. (Algeria)
Barry Breger, M.D. (Canada)
Ian Brighthope, MBBS, FACNEM (Australia)
Gilbert Henri Crussol, D.M.D. (Spain)
Carolyn Dean, M.D., N.D. (USA)
Ian Dettman, Ph.D. (Australia)
Susan R. Downs, M.D., M.P.H. (USA)
Ron Ehrlich, B.D.S. (Australia)
Hugo Galindo, M.D. (Colombia)
Gary S. Goldman, Ph.D. (USA)
William B. Grant, Ph.D. (USA)
Claus Hancke, MD, FACAM (Denmark)
Patrick Holford, BSc (United Kingdom)
Ron Hunninghake, M.D. (USA)
Bo H. Jonsson, M.D., Ph.D. (Sweden)
Dwight Kalita, Ph.D. (USA)
Felix I. D. Konotey-Ahulu, M.D., FRCP (Ghana)
Peter H. Lauda, M.D. (Austria)
Fabrice Leu, N.D., (Switzerland)
Alan Lien, Ph.D. (Taiwan)
Homer Lim, M.D. (Philippines)
Stuart Lindsey, Pharm.D. (USA)
Pedro Gonzalez Lombana, M.D., Ph.D. (Colombia)
Victor A. Marcial-Vega, M.D. (Puerto Rico)
Juan Manuel Martinez, M.D. (Colombia)
Mignonne Mary, M.D. (USA)
Joseph Mercola, D.O. (USA)
Jorge R. Miranda-Massari, Pharm.D. (Puerto Rico)
Karin Munsterhjelm-Ahumada, M.D. (Finland)
Sarah Myhill, MB, BS (United Kingdom)
Tahar Naili, M.D. (Algeria)
Zhiyong Peng, M.D. (China)
Isabella Akyinbah Quakyi, Ph.D. (Ghana)
Selvam Rengasamy, MBBS, FRCOG (Malaysia)
Jeffrey A. Ruterbusch, D.O. (USA)
Gert E. Schuitemaker, Ph.D. (Netherlands)
Thomas N. Seyfried, Ph.D. (USA)
Han Ping Shi, M.D., Ph.D. (China)
T.E. Gabriel Stewart, M.B.B.CH. (Ireland)
Jagan Nathan Vamanan, M.D. (India)
Andrew W. Saul, Ph.D. (USA), Editor-In-Chief
Associate Editor: Robert G. Smith, Ph.D. (USA)
Editor, Japanese Edition: Atsuo Yanagisawa, M.D., Ph.D. (Japan)
Editor, Chinese Edition: Richard Cheng, M.D., Ph.D. (USA)
Editor, Norwegian Edition: Dag Viljen Poleszynski, Ph.D. (Norway)
Editor, Arabic Edition: Moustafa Kamel, R.Ph, P.G.C.M (Egypt)
Editor, Korean Edition: Hyoungjoo Shin, M.D. (South Korea)
Editor, Spanish Edition: Sonia Rita Rial, PhD (Argentina)
Editor, German Edition: Bernhard Welker, M.D. (Germany)
Associate Editor, German Edition: Gerhard Dachtler, M.Eng. (Germany)
Assistant Editor: Michael Passwater (USA)
Contributing Editor: Thomas E. Levy, M.D., J.D. (USA)
Contributing Editor: Damien Downing, M.B.B.S., M.R.S.B. (United Kingdom)
Contributing Editor: W. Todd Penberthy, Ph.D. (USA)
Contributing Editor: Ken Walker, M.D. (Canada)
Contributing Editor: Michael J. Gonzalez, N.M.D., Ph.D. (Puerto Rico)
Technology Editor: Michael S. Stewart, B.Sc.C.S. (USA)
Associate Technology Editor: Robert C. Kennedy, M.S. (USA)
Legal Consultant: Jason M. Saul, JD (USA)
Comments and media contact: drsaul@doctoryourself.com OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication.
This article may be reprinted free of charge provided 1) that there is clear attribution to the Orthomolecular Medicine News Service, and 2) that both the OMNS free subscription link http://orthomolecular.org/subscribe.html and also the OMNS archive link http://orthomolecular.org/resources/omns/index.shtml are included.
Riordan Clinic | Orthomolecular.org
3100 N Hillside Ave
Wichita, Kansas 67219
United States

 (
(