PPI
now browsing by category
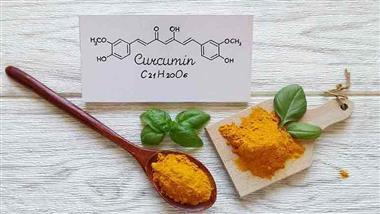
Have You Tried Curcumin for Indigestion?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2024/04/08/curcumin-indigestion.aspx
Analysis by Dr. Joseph Mercola April 08, 2024
STORY AT-A-GLANCE
- If you experience chronic heartburn, a new study indicates that taking curcumin, the biologically active polyphenolic compound found in turmeric, may offer the same protection and relief as the popularly used proton pump inhibitor (PPI) Prilosec (omeprazole)
- Despite knowing the serious side effects associated with PPIs, data show people are prescribed and are taking them at doses higher than recommended and for longer than is recommended by clinical guidelines
- PPIs may increase your risk of a gut infection, vitamin B12 deficiency, heart disease, heart attack, bone fractures and events of cutaneous and systemic lupus erythematosus. In just one week of use, PPIs are associated with significant impairment in attention, executive function, visual memory and working and planning functions
- Steps you can take to naturally reduce symptoms are to identify your trigger foods and eliminate them, don’t eat within four hours of going to bed, consider elevating the head of the bed if you experience nighttime symptoms and don’t wear clothing that is tight around the waist
Curcumin is the major biologically active polyphenolic compound of turmeric and the compound that gives the spice its yellow color. A 2023 study1 published in the BMJ Journal finds that curcumin has yet another health benefit — it helps improve outcomes in people with functional dyspepsia.
In the past decade, researchers have discovered several health benefits from including turmeric and curcumin in your diet. As I reported in 2021, curcumin was among the top five substances researchers had found that could help improve COVID outcomes. However, on their own, turmeric and curcumin have poor bioavailability when taken orally.
Researchers have attributed this to the body’s limited ability to absorb the compound and the body’s ability to rapidly metabolize and eliminate it.2 However, research has also demonstrated that when taken with different compounds, the bioavailability can improve and therefore may help enhance the multiple health benefits that are attributed to the compound.
For example, when taken with piperine, an alkaloid found in black pepper, the bioavailability of curcumin rises by 2,000%.3 Combining curcumin with bromelain, a protease from the pineapple stem, also “substantially increases the absorption of curcumin after oral administration.”4
Curcumin Is Potentially Effective for Functional Dysplasia
In the featured paper,5 151 people completed the study. The group was broken into four groups. They either received two 250 mg capsules of curcumin four times daily, one placebo capsule, 20 mg of Prilosec (omeprazole) and two placebo pills four times daily, or turmeric plus Prilosec.
Prilosec is a proton pump inhibitor (PPI) that is commonly used to treat functional dyspepsia. Functional dyspepsia6 is a type of chronic indigestion in which you experience symptoms of feeling full or bloated during and after meals, heartburn and excessive burping.
The researchers were interested in how curcumin could affect the gastrointestinal tract, so no additional compounds were included to increase bioavailability. The study was a randomized, double-blind controlled trial that engaged participants with functional dyspepsia from university hospitals in Thailand.
The main outcome measure used was the Severity of Dyspepsia Assessment (SODA) score that was measured on Days 28 and 56 to evaluate pain, non-pain and satisfaction with treatment. Secondary outcomes measured included adverse events and severe adverse events.
At the start of the study, patients in all the groups had similar clinical characteristics and scores on the SODA. When evaluating the results, the researchers found that on Days 28 and 56, the SODA scores indicated a significant reduction in symptoms for all but the placebo group.
The improvements were greater by Day 56. The researchers reported no serious adverse events occurred during the study, but acknowledged that individuals who were overweight experienced some liver function deterioration while taking curcumin.7
The researchers acknowledged several limiting factors, including the size of the study, the short intervention and the lack of long-term data. Despite these limitations, the researchers found that “The strength of the study lies in its relevance to daily clinical practice, providing additional drug options in addition to PPIs alone, without added side effects.” and “… the new findings from our study may justify considering curcumin in clinical practice.”8
What You Eat Matters to Your Heartburn
While it might seem counterintuitive, one of the most common causes of heartburn is insufficient amounts of stomach acid. Your body uses stomach acid to properly digest food, breaking it down to absorb nutrients. Without enough stomach acid, undigested food can lead to indigestion and heartburn. Undigested food can also cause bacterial overgrowth.
Yet, if you use PPIs,9 they reduce your stomach acid even further, and over time may cause the glands in the stomach that secrete acid to stop working altogether. A 2017 study10 suggested that a Mediterranean diet that focuses on fruits, healthy fats, lean meat and vegetables could be as effective as PPIs in treating acid reflux symptoms.
The study involved 184 participants and found that after six weeks those who had changed their diet had a slightly greater reduction in reflux symptoms than those who used PPI medication. The study measured symptoms of laryngopharyngeal reflux during which stomach acid affects the tissue at the back of your throat.
Each of your dietary choices can play a role in heartburn symptoms, including beverages. For occasional symptom relief, alkaline water, also tested in the study, may help neutralize the acid and offer relief. You can add 1 teaspoon of baking soda to 4 ounces of orange juice and stir.
Because the reaction causes foaming, make sure the glass is only half full to avoid overflow. Another option is to add a squeeze of lemon or lime juice, or one-half to 1 teaspoon of baking soda in a glass of filtered water.
However, I would underscore the importance of using alkaline water only as a temporary solution and only if reflux is caused by excess stomach acid. The bottom line is that daily consumption of water that’s either too acidic or too alkaline can upset the pH balance in your gastrointestinal tract and trigger heartburn.

Save This Article for Later – Get the PDF Now
PPIs Have Serious Side Effects
PPIs are associated with several significant side effects. For example, individuals who regularly use them can develop a vitamin B12 deficiency as they reduce your body’s ability to absorb vitamin B12 from food.11 Vitamin B12 is a water-soluble vitamin that’s required for red blood cell formation, DNA synthesis, and for the development of the central nervous system.12
A 2017 study13 indicates PPIs may increase your risk for a gut infection. The study engaged a total of 564,969 PPI users and controls (188,323 PPI users and 376,646 controls) and found that those who took certain heartburn drugs had an increased risk of developing C. difficile and campylobacter bacterial infections related to the suppression of stomach acid production.
Research has also found that even short-term use of PPIs can contribute to cognitive changes and long-term use is linked to dementia. One 2015 study14 suggested PPIs were associated with clinically and statistically significant impairment in attention, executive function, visual memory and working and planning functions after just one week of use.
Finally, long-term use has also been linked to chronic kidney disease, heart disease and heart attacks and increased risk of bone fractures and events of cutaneous and systemic lupus erythematosus.15
Despite this evidence, a 2018 Iceland nationwide drug utilization study16 demonstrated a continued increase in overall use in the previous 13 years, particularly in older adults.
The researchers noted that “Patients were increasingly treated for longer durations than recommended by clinical guidelines and mainly with higher doses.”17 A 2022 study from Spain found similar results in which the researchers observed an increase in PPI use especially in a population older than 65 years, “despite the risk of cognitive decline and falls.”18
A 2023 literature review19 identified observational studies on PPI use in individuals older than 18 across several databases from 23 countries. The data indicated that of the people using PPIs, 63%, were younger than 65 years, 56% were female and roughly two-thirds were on high doses of PPIs, 25% of which for more than a year and 28% for more than three years.
After reviewing the global data, the researchers concluded, “Given the widespread use of PPIs and increasing concern regarding long-term use, this review provides a catalyst to support more rational use, particularly with unnecessary prolonged continuation.”20
Steps to Help Naturally Reduce Symptoms
As I have written before, PPIs have serious effects on your health, so it is wise to first consider non-drug alternatives to reduce your symptoms. Since the foods you eat affect your reflux and heartburn symptoms, you can begin by identifying the foods that trigger your symptoms and eliminating them from your diet.
If you are on a PPI, it is vitally important that you seek to wean from them as soon as possible with your physician. The best H2 blocker to use would be Pepcid (famotidine) which you will gradually wean from as well.
Foods that commonly increase heartburn21 include fried and processed foods, such as fast food, pizza, and potato chips or similar fried snack foods. Other foods that commonly make the list are tomato-based sauces, citrus fruits and carbonated beverages.
After you have eliminated the foods that trigger your symptoms, there are several more steps you can take. Steer clear of clothes that are tight around your waist or middle22 since it can increase the symptoms of heartburn.
When you sit down, tight clothes squeeze your abdominal area, increasing the risk your stomach contents will push through the sphincter at the top of the stomach and you’ll experience reflux.
It’s important to remember that for many people, heartburn gets worse at night after you are lying down to go to sleep.23 It’s easier for food to back up the esophagus without the push of gravity as you’re standing.
Don’t eat in the three to four hours before going to sleep at night and if you’re still having trouble, try elevating the head of your bed approximately 6 inches. Don’t simply sleep on extra pillows as that adds an extra strain to your neck and shoulders.
The angle of the pillows can also increase pressure on the abdomen, depending on the position. Instead, consider blocks sold specifically for elevating the bed, which stabilizes it, so it doesn’t move at night.
Ginger has long been known to have a gastroprotective effect. Add two to three quarter-size slices of fresh ginger root to 2 cups of hot water and let it steep for several minutes. Drink it approximately 20 minutes before eating your meal. If heartburn seems to plague you at night, try a cup of chamomile tea about an hour before going to sleep.24
- 1, 5 BMJ, 2023; doi: 10.1136/bmjebm-2022-112231
- 2, 3 Foods, 2017;6(10)
- 4 Metabolism Open, 2020; 100066
- 6 Cleveland Clinic, Functional Dyspepsia
- 7 MedicalXpress, September 12th, 2023
- 8 BMJ, 2023; doi: 10.1136/bmjebm-2022-112231 75% DTP
- 9 Cleveland Clinic, Hypochlorhydria, What Causes bullet 3 30% DTP
- 10 Journal of the American Medical Association Otolaryngology – Head & Neck Surgery, 2017;143(10)
- 11, 12 National Institutes of Health, Vitamin B12
- 13 British Journal of Clinical Pharmacology, 2017; doi: 10.1111/bcp.13205
- 14 Alzheimer’s Research and Therapy, 2015; 7
- 15 US Pharmacist, 2017; 42 (7)
- 16, 17 Therapeutic Advances in Gastroenterology, 2018; 11
- 18 BMC Public Health, 2022; 22(818)
- 19, 20 European Journal of Pharmacology, 2023;79(9)
- 21 Johns Hopkins Medicine, GERD Diet: Foods That Help With Acid Reflux
- 22 Everyday Roots, 15 Natural Remedies for Heartburn and Severe Acid Reflux #10
- 23 Everyday Roots, 15 Natural Remedies for Heartburn and Severe Acid Reflux #4
- 24 Everyday Roots, 15 Natural Remedies for Heartburn and Severe Acid Reflux #15
The Microbiome Solution — Healing Your Body From the Inside Out
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/12/24/microbiome-solution.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola December 24, 2023
STORY AT-A-GLANCE
- One of the worst things you can do during pregnancy is to take an antibiotic. Young children also need to be shielded from antibiotics, as they devastate the microbiome
- Other medications best avoided, due to their devastating impact on your microbiome include hormone treatments, including birth control pills, antibacterial products containing triclosan and proton pump inhibitors
- Fiber-rich vegetables are massively important. Not only do they provide valuable nutrients your body needs, they also provide nutrition to the microbes in your gut, which feed on fiber
By now, you’re probably aware of how important a balanced gut microbiome is to your overall health, but how do you go about optimizing your gut flora? And what steps can you take to protect and nourish your baby’s microbiome, even before and during birth?
In this interview, Dr. Robynne Chutkan, a gastroenterologist (a doctor who specializes in the gut) and author of the book, “The Microbiome Solution: A Radical New Way to Heal Your Body From the Inside Out,” will guide you through the details.
Chutkan finished medical school in 1991. Like most conventionally trained doctors, she whole-heartedly endorsed pharmaceutical intervention “whenever possible, as frequently as possible.” Over the course of several years, however, she began to investigate alternative routes to health.
“My area of expertise is inflammatory bowel disease,” she says. “I trained in New York, at Columbia for medical school and residency, and then at Mount Sinai Hospital … Never once during my training did the idea that you could treat this set of diseases with food as opposed to pharmaceutical intervention, ever come up …
But when I arrived at Georgetown to join the faculty in 1997 … I started seeing a lot of patients, a lot of them women. Many wanted to know, ‘What can I do? What can I eat? How can I change what I’m doing to feel better?’ Of course, I had no answers at all for these questions.
I just had a lot of fancy drugs that I knew a lot about. Over the course of time, I started to experiment a little bit, mostly on myself, playing around with different ways of eating …”
Approaching Food as Medicine
She also conducted a study, in which she asked patients about their use of alternative and complementary practices to treat their Crohn’s and ulcerative colitis. She was surprised to discover that 70% of them were using some kind of complementary or alternative technique, sometimes in addition to conventional medicine.
“It was a sort of don’t-ask-don’t-tell policy,” she says. “I started to get interested and I wanted to know what people were doing and if it was helping …
This was the time when the specific-carbohydrate diet, which is very similar to the Paleo diet, had been popularized … I clearly remember the first patient I sat down with who … had had severe Crohn’s disease. She came back and was feeling great …
She was eating lean protein, lots of vegetables and some nuts and seeds … I remember doing her colonoscopy and seeing her very severe Crohn’s healed. I could not believe it. I said ‘I’ve got to find out more about this.’
I think it really was the patients who caused me to question what we were doing. I started looking at the drugs we were using and the side effects. Don’t get me wrong, I’m all for judicious use of conventional drugs when you don’t have lots of other options.
But to be strongly recommending drugs that we know can cause cancer and severe infection and other problems, and not having any conversation about this concept of foodist medicine, which is so well-proven, particularly in the gastroenterology world, I think that’s medical negligence.”
How C-Section Can Set a Child on the Path Toward Autoimmune Disease
Another incentive driving Chutkan’s growing interest in alternative treatments was her daughter. She was delivered via C-section, and because Chutkan had contracted influenza right before the delivery, her newborn daughter was given antibiotics as a precaution.
This was the beginning of a long series of illnesses, where she’d get sick, receive another round of antibiotics, only to get sick again and receive more medication. By the age of 2, her daughter had received 16 rounds of antibiotics.
According to Chutkan, this pattern is very common among patients who are subsequently diagnosed with Crohn’s disease and ulcerative colitis. Many are C-section babies who were then bottle-fed and received multiple rounds of antibiotics.
“I saw her heading down that road and I said ‘I really have to do something. If we don’t stop this cycle, this is what’s going to happen.’ I’m proud to be a doctor, but it’s sometimes hard to hold your head up these days because in my office, most of what I spend my time doing is trying to undo medical mischief.
Well-meaning physicians who either are not well-informed or just have tunnel vision; dermatologists putting young people on years of potent antibiotics, when you consider the fact that five days of a broad-spectrum antibiotic … can remove a third of your gut bacteria … We are creating disease.”

Download this Article Before it Disappears
Avoid Antibiotics Unless Your Life Hangs in the Balance
Indeed, one of the worst things you can do during pregnancy is to take an antibiotic. Young children also need to be shielded from antibiotics, as they devastate the microbiome. Perhaps the single most important take-home point is to avoid antibiotics unless your life hangs in the balance.
Don’t take them frivolously, and certainly not as a precautionary measure. Other medications best avoided, due to their devastating impact on your microbiome include:
• Hormone treatments, including birth control pills
• Antibacterial products containing triclosan
• Proton pump inhibitors (PPIs). According to Chutkan, research shows 20% of the bacteria in the microbiome are changed from long-term use of acid suppressing drugs.
In fact, the authors concluded that PPI use was just as dangerous as antibiotic use in the long term. Despite that, gastroenterologists routinely put patients on long-term acid suppression without giving it a second thought
Should you have an infection, there are a number of alternatives to antibiotics you can try. For example, D-mannose is very effective against urinary tract infections. “We use a topical form of probiotics mixed with coconut oil for bacterial vaginosis for women. It works great,” Chutkan says.
Beware of Hidden Antibiotics
Chutkan also addresses the issue of hidden antibiotics. Eighty percent of all the antibiotics sold in the U.S. are actually used in the food industry. Animals raised in concentrated animal feeding operations (CAFOs) are routinely given low-dose antibiotics to prevent disease associated with factory farming. So while you may be really judicious about medical antibiotics, you may still ingest antibiotics through factory-farmed food, especially animal products.
“I think this is an area where it’s really important to buy organic and to know not just what you’re eating, but what the food you’re eating has eaten, tracing it all the way back, because 80%, that’s an astounding number; we already have the highest per capita consumption of antibiotics in the world …
From infancy, the average American child will take somewhere around 18 to 20 courses of antibiotics by their 18th birthday. Then you add to that, how many courses of antibiotics they’re probably ingesting with food. It’s really astounding. It’s almost like the myth of Sisyphus.
We’re on this treadmill. From the minute we’re born — one could argue even before birth with the in-utero exposure — we are in this incredible downward spiral to destroy our microbiome. You have to be so vigilant about all of these things.”
Fecal Microbiota Transplant — A Potentially Life-Saving Procedure
Chutkan’s book, “The Microbiome Solution,” provides an excellent chapter on fecal microbiota transplants (FMTs). It even includes instructions on how to do it yourself, were you to choose that route. While most people are not candidates for a stool transplant, it can be a life-saving measure in extreme cases. That said, it’s important to understand that the stool transplant is only as good as a donor’s stool.
“I love my husband very much, but he grew up playing football and eating Burger King every day after practice. I don’t want his stool, because it’s probably not robust enough, growing up eating a standard American diet and taking the usual arsenal of medications.
I’ve always said, if I ever develop a severe autoimmune disease … and I am failing the typical options, I’m heading to Tanzania to get some stool from the Hadza tribe, or down to the Amazon. I want some high-octane stool,” Chutkan says. “When you contemplate donor stool, it’s not just a matter of excluding serious infectious diseases like HIV, syphilis or hepatitis. It’s really about evaluating how robust the microbiome of your donor is …”
Your Microbiome Is Constantly Changing and, With That, Your Health
While an FMT can be highly beneficial in extreme cases, the vast majority of people simply need to optimize their own microbiome through dietary and lifestyle changes. The good news is our microbiomes are constantly changing, based on diet and environmental exposures, so you have a great deal of personal control.
If you have a long history of antibiotic use, it may be more difficult for you to shift your gut flora and repair the cellular-microbial damage that has already occurred. But you can still improve a great deal.
“For most people who have eaten poorly [and] taken some drugs, there is incredible opportunity for recovery, but it really has to be meaningful change,” Chutkan says.
“The idea that you can continue to eat potato chips and soda and not eat vegetables and just take a fancy probiotic and get better, is really magical thinking. I really try to stress in my practice that it’s not the microbes that you put in your body; it’s what you feed those microbes.”
Fiber-rich vegetables are massively important. Not only do they provide valuable nutrients your body needs, they also provide nutrition to the microbes in your gut, which feed on fiber. Another part of the equation is eating foods grown in healthy soils. Factory-farmed vegetables grown in nutrient-poor soils are not going to give you the same bang for your buck.
As noted by Chutkan and many other health experts, nutrition and human health really starts in the soil. To learn more, check out Dr. Maya Shetreat-Klein’s book “The Dirt Cure: Growing Healthy Kids With Food Straight from Soil.”
How to Optimize Your Baby’s Health if a C-Section Is Unavoidable
Since you’re bypassing the birth canal, children born via C-section are not “inoculated” with their mother’s bacteria. Sometimes a C-section is necessary. It can be lifesaving for the baby or the mother. But evidence suggests C-sections are vastly overused in the U.S., and most are not medically necessary.
In her book, Chutkan includes a complete birthing plan to optimize your and your baby’s microbiome, and it begins with the recommendation to avoid C-section at all cost, unless medically necessary.
“You really have to push because, again, your physician is very well-meaning, but they have been trained and indoctrinated to think that a C-section is fine. You might find yourself in the unusual position of having to educate your physician about the risks of C-section. There’s plenty of good information out there to do that. The first thing is to try and avoid it,” she says.
“If you have to have a C-section, I love the information Maria Gloria Dominguez-Bello [Ph.D.,] provides [on] vaginal seeding … [M]ake sure your doctor and their team know about this. Because if you start doing this and people don’t know what you’re doing, they’re going to call security and take the baby away.
The idea is to take a gauze pad and soak it in the perineal juices … Then when the baby is born via C-section, instead of essentially disinfecting them with antibacterial products like they do in the hospital, take this vaginal pad that’s soaked in all this wonderful flora from the mother and wipe the baby down, especially the head, the eyes, the mouth, all of that. Wipe them down so you’re sort of approximating a vaginal birth.”
According to Chutkan, studies show babies born vaginally are colonized with Bifidobacteria, lactobacillus and many other healthy bacteria from the mother’s microbiome. C-section babies are colonized mostly with hospital-acquired staph, and this microbial difference can follow the child for years to come.
Not surprisingly then, C-section babies tend to have higher rates of allergy, asthma, obesity and autoimmune diseases — all of which have been linked to poor microbial diversity and makeup. Being able to intervene with this vaginal seeding technique is quite brilliant, and could go a long way toward normalizing your baby’s microbiome if you have to have a C-section.
Other Dos and Don’ts for New Parents
Next comes breastfeeding. Not only is breast milk nutritionally superior to formula, it also has a direct impact on your baby’s microbiome. The third most common ingredient in breast milk is human milk oligosaccharides (HMOs), a type of sugar that is completely indigestible.
It provides no nutrition per se, rather it nourishes the beneficial bacteria in your baby’s digestive tract, which in turn helps repel staph and other potentially harmful microbes, including microbes that may linger on your nipples.
“It’s a great example of this synergy between what’s happening on the mother’s side and what’s going on in the baby’s side, and how it’s all supposed to work together. That’s another critical thing for people to know,” Chutkan says, adding:
“It’s amazing how much stuff gets done to you in the hospital that you don’t know about. Most women don’t know they get antibiotics for a C-section … I didn’t know that my daughter got not one but two potent antibiotics intravenously in the neonatal intensive care unit. You sign a general consent for treatment …
You know that doctors are well-meaning. You know they’re vested in a good outcome for the health of your child, but you make the crucial mistake of thinking they know and completely understand the ramifications of what they’re doing. It’s clear that they don’t, and so you have to be very aware of that …
Your doctors, for the most part … are lovely, well-meaning people, but they are not well-informed. They are getting their medical information from sources that compel them to keep practicing [a certain] way.”
Vitamin D and Inflammatory Bowel Disease
As previously noted, Chutkan’s specialty is inflammatory bowel disease (IBD), a serious autoimmune disease that can be lethal. IBD is not to be confused with irritable bowel syndrome (IBS), which is a functional disease — it can be painful and disabling, but it’s not going to kill you. IBD patients are frequently prescribed very toxic drugs and may even require surgery to remove a part of their colon.
If you have IBD, optimizing your vitamin D to a level between 40 and 60 nanograms per milliliter (ng/ml) is an important consideration. Crohn’s patients also need to pay attention to vitamin B12, because when your ileum — the end part of your small intestine — is inflamed or has been surgically removed, you cannot absorb B12 as efficiently. Malabsorption of fat-soluble vitamins A, D, E and K, magnesium, iron and more, can also occur.
“Vitamin D has definitely been shown in many studies to be important for inflammation in general, certainly in patients with IBD,” Chutkan says.
“It’s one of the first things we check and make sure that people are adequately supplemented … We have people we put on high-dose supplementation … if they’re down in the single digits … I recommend getting 20 minutes of sun exposure [on] upper body, arms and shoulders, without sunscreen, each day.”
On Treating IBD
When it comes to treating IBD, Chutkan focuses on using food as medicine, and in 77% of cases, her patients will no longer need immune modifying agents once they’ve properly adjusted their diet. She typically begins by assessing the level of inflammation. The most challenging situation is when you have “fibrostenotic disease,” where Crohn’s disease has caused severe scarring and narrowing of the gastrointestinal (GI) tract. In some cases, it can be severe enough to be irreversible.
People with colitis who have a lot of ulceration in the colon, and people who have Crohn’s who don’t have a lot of scarring but have active ulceration, are generally able to successfully treat their condition through diet. Next, she screens for nutrient deficiencies, such as vitamin D, B12, ferritin and fat-soluble vitamins, and begins assessing the diet. Chutkan uses a combination diet that is part specific-carbohydrate diet, part paleo and part vegan.
Increasing Vegetable Intake Is Crucial
Three years ago, Chutkan and colleagues published a small pilot study consisting of 12 patients, nine with Crohn’s and three with ulcerative colitis.
“We looked retrospectively at the diet. We found some interesting things. We found that the average time for the diet to work was about 90 days. When I say to work, to really kick in to the point where people felt like they were in remission. But some people notice results in as quickly as two to three days. Other people take several months. Ninety days was kind of the sweet spot.
Two-thirds of patients were able to get off their medication or significantly reduce their medication. Again, the majority of people, when we looked endoscopically, had healing of the inflammation.
But this is the most important part of the study: everybody took out the processed carbohydrates. Everybody was off gluten, off refined sugar. Essentially grain-free for the most part. As people get better, we do add in some brown rice, some legumes and so on.
For the most part, it was looking like a modified paleo diet. But there were two distinct groups: the group who got better and the group who didn’t, despite excluding all the not-so-great stuff. What was the difference?
The difference was the amount of vegetables people were consuming. The people who took out the gluten and the processed sugars … without increasing their vegetable intake, did not tend to do a lot better. The people who really ramped up their consumption of green leafy vegetables, and particularly the stringy vegetables like celery, asparagus and artichokes, which are high in inulin that really feed gut bacteria, did significantly better.”
So, a key take-home point here is that it’s not enough to simply remove certain foods, such as sugar and refined grains. You must also replace them with a significant amount of vegetables.
In fact, there appears to be a critical threshold when it comes to vegetables, which you must meet in order to see meaningful changes in your health. Dr. Terry Wahls has noted that multiple sclerosis (MS) patients typically need six to nine servings of leafy greens each day in order to affect positive change.
Chutkan says the same applies to autoimmune patients with Crohn’s and ulcerative colitis. Each morning, she makes herself a green smoothie with spinach, kale, celery, parsley, green apple, a peeled lemon, some fresh ginger and water. Each day, she’ll drink two to four glasses.
On Breaking the Mold
Chutkan is a perfect example of a conventional physician who, by listening to her patients and keeping an open mind, broke through the brainwashing — the carefully orchestrated propaganda created by the drug and medical industries. And she shares a great deal of priceless information in her book, “The Microbiome Solution.”
“[W]hen I saw the results of a meta-analysis out of Mount Sinai hospital … looking at over 7,000 patients with inflammatory bowel disease and identifying frequent antibiotic use, particularly in childhood, as one of the main risk factors for developing IBD, I said, ‘People have to know this.’
… [A]s an author, it is an incredible privilege to be able to put your nickel down and say ‘This is what I think. This is what I believe in. I feel an obligation to share it with you.’ But it’s also scary. People come after you …
I had a lot of conversations with Penguin about what I could or couldn’t say, or should or shouldn’t say. It’s scary because you know there’s an incredible amount of money being made by some of these companies. When you say something that’s critical, their goal is to crush you. They’ve done it very effectively to a lot of people we know.
It’s scary but you get to the point where you feel like you cannot legitimately not share this information with people. As you know, books are not a way to get rich, right? Typically, books are probably, at best, a break-even proposition, or you lose money writing a book when you think about the amount of time it takes.
But it is an incredible way to take this information out of the office … and get it into the hands of millions of people. That’s a wonderful privilege … I do have to say that I am emboldened by practitioners like you who have been doing this for a very long time and play such an important role in this education of the public.
You’ve been criticized by conventional medicine and by pharmaceutical companies. It really emboldens those of us who have our eyes open to say ‘You know what? I’m going to speak the truth. I’m going to educate patients. I’m going to try to bring a few colleagues along. I’m going to be okay.'”
How Patients Can Help Their Doctors
As noted by Chutkan, many doctors still do not realize the wool has been pulled over their eyes. They don’t realize they are being used to market drugs for pharmaceutical companies — some of which are effective, others not so much, and virtually all of which have side effects.
However, all is not lost. Just like Chutkan came to see the light after being repeatedly prompted by her patients to provide answers other than drugs, you too can affect positive change by talking to and informing your doctor about strategies that are important to you.
“I think … it’s so important for patients to not just abandon their doctors,” she says. “If you have a doctor and you have a decent relationship with them, but they’re still hell bent on prescribing an antibiotic you don’t need, I think it’s so important to say to them ‘This is why I don’t want to take the antibiotic. Here is a book you should read.’
Because that’s what people did with me. People trusted me. They felt that I had their best interest at heart. They took the time to educate me and I’m so glad they did. I think we have to bring a colleague along. We have to bring our physicians along and not just abandon them entirely.”
One of the books you can bring your physician if he or she wants to prescribe antibiotics is “The Microbiome Solution.” It should really open their eyes. Chutkan is incredibly articulate, and her book is chockfull of valuable information that can have a tremendously beneficial impact on your health.
Popular Heartburn Meds Linked to Osteoporosis
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/12/19/ppi-osteoporosis.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola December 19, 2023
STORY AT-A-GLANCE
- An estimated 12.3 million Americans over 50 are affected by osteoporosis (“porous bone” or low bone density), and an additional 47 million younger Americans are in the early stages. Worldwide, the prevalence is 18.3%
- Rates of hip fractures vary from tenfold to a hundredfold between countries, showing that low bone density is not a consequence of aging per se, but is dependent on lifestyle factors, including the use of certain drugs such as proton pump inhibitors (PPIs), the most popular heartburn medications on the market
- PPIs are only recommended for short-term use, yet 60% of users report staying on the drug for more than one year; 31% are still on them after three years. More than 60% are also taking them to treat conditions for which these drugs are not indicated, such as indigestion
- Dozens of studies show rates of hip fractures are elevated among both long- and short-term users of PPIs, and at all dose levels
- More recent research suggests one of the primary ways by which PPIs damage bone may be by way of collagen, as these drugs have been shown to inhibit collagen production through several mechanisms of action
Americans spend a whopping $13 billion a year on over-the-counter (OTC) antacids (acid neutralizers) and OTC and prescription proton pump inhibitors (PPIs), which are the most popular heartburn medications on the market.1 It’s estimated that more than 15% of the population are on PPIs.2,3
Prescription PPIs like Nexium, Dexilant, Prilosec, Zegerid, Prevacid, Protonix, Aciphex and Vimovo inhibit acid production in your stomach and are routinely used to treat gastroesophageal reflux disease (GERD), a condition affecting about 20% of the U.S. population.4 OTC versions like Prilosec OTC, Zegerid OTC and Prevacid 24HR are also available.
Once prescribed, your doctor may keep you on a PPI drug for years, despite label warnings suggesting they be used only for short periods. One of the potential ramifications of long-term use of heartburn medication is osteoporosis. In the Nutrition Facts video above,5 Dr. Michael Greger reviews the evidence for this.
Your Osteoporosis Risk Is Highly Modifiable
As of 2020, an estimated 12.3 million Americans over 50 were affected by osteoporosis (“porous bone” or low bone density), and an additional 47 million younger Americans were in the early stages.6 Worldwide, the prevalence is 18.3%, according to data cited by Greger.
If your bones are getting compromised in your 40s or even 30s, your life expectancy, not to mention quality of life, will be seriously lowered. As noted by Greger, the good news is, osteoporosis is not an inevitable outcome even in advanced age, as lifestyle has been shown to play the greatest role in its development.
Rates of hip fractures vary from tenfold to a hundredfold between countries,7 showing that low bone density is not a consequence of aging per se, but is dependent on things like diet, exercise, alcohol use — and the use of certain drugs, including:8
- PPIs and H2 blockers
- Antidepressants, anti-anxiety and antipsychotic drugs
- Antiparkinsonian drugs
- Benzodiazepines and other sedatives
- Systemic corticosteroids
PPIs Linked to Bone Fractures
The link between PPIs and brittle bone is strong enough that the U.S. Food and Drug Administration issued a safety alert on it in 2010, warning that the use of these drugs increases the risk of wrist, hip and spine fractures. As noted in that safety announcement:9
“The new safety information is based on FDA’s review of several epidemiological studies that reported an increased risk of fractures of the hip, wrist, and spine with proton pump inhibitor use.
Some studies found that those at greatest risk for these fractures received high doses of proton pump inhibitors or used them for one year or more. The majority of the studies evaluated individuals 50 years of age or older and the increased risk of fracture primarily was observed in this age group.
While the greatest increased risk for fractures in these studies involved people who had been taking prescription proton pump inhibitors for at least one year or who had been taking high doses of the prescription medications (not available over-the-counter), as a precaution, the ‘Drug Facts’ label on the OTC proton pump inhibitors (indicated for 14 days of continuous use) also is being revised to include information about this risk.
Healthcare professionals and users of proton pump inhibitors should be aware of the possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors, and weigh the known benefits against the potential risks when deciding to use them.”

Download this Article Before it Disappears
FDA Safety Alert Is Out of Date
However, in March 2011, the FDA removed the warning for PPIs sold over the counter, claiming they had “concluded that fracture risk with short-term low dose PPI use is unlikely.” The caveat, of course, is that users of OTC PPIs must then strictly follow usage recommendations to avoid the risk of bone fractures.
OTC PPIs are not to be used for more than 14 days in a row, up to three times in a single year. Chances are, many users do not stick to these parameters, and since there’s no warning label, they might not think anything of it.
According to one survey, 60% of PPI users stayed on the drug for more than one year, and 31% were still on them after three years. More than 60% were also taking them to treat conditions for which these drugs are not indicated, such as indigestion.10 So, overuse is clearly a problem.
What’s more, as noted by Greger, as of 2023 there are dozens of studies showing rates of hip fractures are elevated among both long- and short-term users, and at all dose levels. So, the FDA’s safety alert is seriously outdated.
PPIs and the Risk of Bone Fractures
Studies showing a clear link between PPI usage and bone fractures include a prospective study11 published in 2009, which found that use of the PPI omeprazole was “a significant and independent predictor of vertebral fractures,” with a 3.50 relative risk compared to nonusers.
Relative risk ratio refers to the probability of an event occurring in the exposed group versus the probability of the same event occurring in a nonexposed group.12 So, in this case, PPI users were 3.5 times, or 350%, more likely to fracture their spines during the six-year follow-up compared to those who did not use the drug.
A meta-analysis13 published in 2016, which looked at 18 studies involving a total of 244,109 fracture cases, concluded PPI use was associated with a “modestly” increased risk of all fractures, including hip and spine fractures.
Here, pooled analysis showed PPI use raised the relative risk of hip fracture by 1.26 times, and this was true both for short-term (less than one year) and long-term (more than one year) use. The relative risk of spine fracture was also 1.58 times higher, and any-site fractures 1.33 times higher among PPI users.
How PPIs Cause Osteoporosis
As for how PPIs cause osteoporosis, studies suggest they can affect bone density by:
| Inducing hypochlorhydria (a state where production of hydrochloric acid production is absent or very low), which inhibits calcium absorption14 |
| Dysregulating bone resorption, which is essential for healthy bone15 |
| Secondary hyperparathyroidism caused by a negative calcium balance16 |
| PPI-induced hypergastrinemia resulting in parathyroid hypertrophy or hyperplasia17 |
| Gut microbiome alterations18 |
| Hypomagnesemia (low magnesium)19 |
Interestingly, more recent research suggests one of the primary ways by which PPIs damage bone may actually be by way of collagen, as these drugs have been shown to:20
- Inhibit Type 1 collagen found in bone by increasing the release of calcium and deoxypyridinoline (the latter of which provides structural stiffness to Type 1 collagen)
- Inhibit the gene expression of several collagen types
- Reduce total collagen levels by inhibiting expression of dimethylarginine dimethylaminohydrolase (DDAH)
- Impair vitamin B12 absorption, which can lead to elevated homocysteine. High homocysteine increases the risk of fractures by altering the quality of collagen21
As noted in a 2020 paper in the Frontiers in Endocrinology:22
“PPIs may actually target the ECM [extracellular matrix] in general and members of the collagen family in particular to influence bone pathophysiology including increasing the risk of osteoporosis and osteoporotic fractures …”
Other Risks Associated With PPIs
Dependency is also a real risk. Research cited by Greger found that just two months of PPI therapy in healthy volunteers induced “acid-related symptoms” when the drug was withdrawn.23 Besides bone fractures, other health risks associated with PPIs include:24
| Kidney disease25 |
| Intestinal infections, including Clostridioides difficile infection — In one study, those taking PPIs had a 1.7 to 3.7 times increased risk of developing C. difficile or Campylobacter infection compared to nonusers26 |
| Stomach cancer |
| Gastrointestinal polyps |
| Pneumonia |
| Heart disease27 and heart attacks, even if you have no prior history of cardiovascular disease28 |
| Erectile dysfunction |
| Premature death |
| Higher risk of knee replacement29 |
| Dementia30 and Alzheimer’s disease31,32 — In one study, PPIs were found to cause statistically and clinically significant impairments in the participants’ executive functions, visual memory and planning function after just one week of use33 |
Natural Remedies for Treating Occasional Reflux Problems
As explained in “Keys to Optimal Digestion” and “Why You Should Never Take Antacids for Digestive Reflux,” stomach acid serves several important functions, such as breaking down proteins, killing ingested pathogens, ensuring optimal nutrient absorption, and regulating the rest of the digestion process.
If you use acid-blockers, you’re compromising your entire digestive system. You may also be compromising your bone health and significantly raising your risk of osteoporosis and serious bone fractures that take a long time to heal.
So, if you suffer from occasional heartburn, indigestion and other minor reflux symptoms, forgo the PPIs and try one or more of the following nondrug alternatives instead:34,35,36,37,38
| Aloe juice — The juice of the aloe plant naturally helps reduce inflammation, which may ease symptoms of acid reflux. Drink about one-half cup of aloe juice before meals. To avoid its laxative effect, look for a brand in which the laxative component has been removed. |
| Apple cider vinegar (raw, unfiltered) — Take 1 tablespoon of raw unfiltered apple cider vinegar in a large glass of water before or directly after meals. |
| Astaxanthin — When compared to a placebo, this potent antioxidant was found to reduce symptoms of acid reflux, especially for individuals with pronounced H. pylori infection.39 The researchers concluded a daily dose of 40 mg of astaxanthin was effective for reflux reduction. |
| Baking soda — One-half to 1 teaspoon of baking soda (sodium bicarbonate) in an 8-ounce glass of water, or orange juice, will help neutralize your stomach acid and ease the burn of acid reflux. While I do not advise this as an ongoing remedy, it is effective on an “emergency” basis when you are in excruciating pain. |
| Ginger root — Ginger has a gastroprotective effect by suppressing H. pylori. It also accelerates gastric emptying which, when impaired, contributes to heartburn. Add two or three slices of fresh ginger root to 2 cups of hot water and let it steep for several minutes. Drink it about 20 minutes prior to your meal. |
| Sauerkraut — Consuming sauerkraut or cabbage juice will stimulate your body to produce stomach acid. |
| Glutamine — The amino acid glutamine has been shown to address gastrointestinal damage caused by H. pylori. Glutamine is found in many foods, including beef, chicken, dairy products, eggs, fish and selected fruits and vegetables. L-glutamine is widely available as a supplement. |
| Ripe papaya or a papain supplement — Papaya contains papain, an enzyme useful for breaking down both protein and carbohydrates. |
| Fresh pineapple or bromelain supplement — Bromelain is a proteolytic enzyme found in pineapple that helps digest proteins. |
| Pepsin supplement — Like bromelain, pepsin is a proteolytic enzyme involved in protein digestion.40 |
| Betaine HCI supplement — Betaine HCl is the hydrochloride salt of betaine, not to be confused with betaine or trimethylglycine (TMG). As noted in a 2020 review paper:41 “… the most common recommendation for the use of betaine HCl supplements is usually implemented using an empirical test for low stomach acid whereby increasing doses of betaine HCl are given during sequential meals until such time as an uncomfortable sensation is noticed by the patient.
Along with improvements in symptoms of dyspepsia (or laboratory analysis of improved protein digestion), the lack of side effects acts is an empirical confirmation that low gastric acid production was contributing to poor digestion and/or dyspeptic symptoms.” |
| Bitters — Bitters have a long history of use in herbal medicinal traditions to promote digestion and/or to relieve digestive complaints.42 |
| Slippery elm — Slippery elm coats and soothes your mouth, throat, stomach and intestines, and contains antioxidants that may help address inflammatory bowel conditions. Because it stimulates nerve endings in your gastrointestinal tract, it is useful for increasing mucus secretion, which has a protective effect against ulcers and excess acidity. |
| Vitamin D — Vitamin D is important for your gut health. Once your vitamin D levels are optimized, you will benefit from your body’s production of about 200 antimicrobial peptides that will help eradicate gut infections. |
| Zinc — Your stomach needs zinc to produce stomach acid, so make sure your body has the necessary raw ingredients. The recommended daily amount for adults is 8 to 11 mg. Zinc-rich foods include oysters, lobster, beef, cashew nuts, beans and raw yogurt. A zinc supplement can be used if you rarely eat these foods.43 |
Talk to Your Doctor About Getting Off PPIs
If you’re currently on a PPI, I strongly recommend working with your doctor to wean off it, as inhibiting stomach acid can raise your risk of other, far more serious health conditions, including:44
| Osteoporosis | Asthma |
| Depression | Gallbladder disease |
| Migraines | Macular degeneration |
| Autoimmune conditions, including but not limited to Celiac disease, Type 1 juvenile diabetes, Grave’s disease (hyperthyroid), lupus, multiple sclerosis (MS), rheumatoid arthritis and ulcerative colitis |
The best and safest way to do that is to work with your doctor to lower the dose you’re taking while simultaneously implementing the following lifestyle modifications:
- Avoid reflux triggers and/or any food that irritates your stomach
- Avoid processed foods and sugar
- Eat a Mediterranean diet, focused on fruits, healthy fats, lean meats, nuts and vegetables. Research published in the Journal of the American Medical Association Otolaryngology — Head & Neck Surgery found a Mediterranean diet was as effective as PPIs in treating acid reflux symptoms45
- Reseed your gut with beneficial bacteria from traditionally fermented foods or a high-quality probiotic supplement
- Thoroughly chew each bite of food
Once you get down to the lowest dose of the PPI, you can start substituting with an over-the-counter H2 blocker like Pepcid (famotidine) which appears to be the safest of all the OTC H2 blocker options out there. Then, gradually wean off the H2 blocker over the next several weeks.
- 1 Time September 7, 2017
- 2, 44 Midwestern Doctor Substack September 16, 2023
- 3 Therapeutic Advances in Gastroenterology 2018; 11: 1756284818777943
- 4 The Surgical Clinic. What Is GERD?
- 5 Nutrition Facts December 11, 2023
- 6 The Washington Post October 17, 2023 (Archived)
- 7 YouTube NutritionFacts December 11, 2023 1:38 minutes
- 8 YouTube NutritionFacts December 11, 2023 5:53 minutes
- 9 FDA Safety Alert May 25, 2010
- 10 YouTube NutritionFacts December 11, 2023 3:37 minutes
- 11 Calcif Tissue Int January 2009; 84(1): 13-19
- 12 StatPearls Relative Risk
- 13 Osteoporosis International January 2016; 27(1): 339-347
- 14 JAMA December 27, 2006; 296(24): 2947-2953
- 15, 20, 22 Front. Endocrinol. July 22, 2020
- 16, 17, 18, 19, 21 International Journal of Molecular Sciences September 2022; 23(18): 10733, Section 3
- 23 YouTube NutritionFacts December 11, 2023 4:21 minutes
- 24 YouTube NutritionFacts December 11, 2023 4:33 through 5:03 minutes
- 25 The Journal of the American Medical Association 2016;176(2):238
- 26 British Journal of Clinical Pharmacology, January 5, 2017, DOI: 10.1111/bcp.13205
- 27 PLOS ONE December 27, 2013, DOI: 10.1371/journal.pone.0084890
- 28 PLOS One June 10, 2015 DOI: 10.1371/journal.pone.0124653
- 29 Osteoarthritis Cartilage April 2022; 30(4): 559-569
- 30 JAMA Neurology February 15, 2016, doi: 10.1001/jamaneurol.2015.4791
- 31 Annals of Translational Medicine 2016;4(12):240
- 32 Journal of the American Medical Association 2016;73(4):410-416
- 33 Alzheimer’s Research & Therapy 2015;7:79
- 34 Health January 25, 2016
- 35 Everyday Roots, 15 Natural Remedies for Heartburn & Severe Acid Reflux
- 36, 40, 43 Medical News Today 6 Ways to Increase Stomach Acid
- 37, 41, 42 Integr Med February 2020; 19(1): 32-36
- 38 Drugwatch PI Alternatives
- 39 Phytomedicine June 2008; 15(6-7): 391-9
- 45 Journal of the American Medical Association Otolaryngology – Head & Neck Surgery September 7, 2017; doi: 10.1001/jamaoto.2017.1454
How to Put an End to Heartburn, Without Pills?
Reproduced from original article:
https://articles.mercola.com/sites/articles/archive/2023/08/30/natural-remedies-for-heartburn-relief.aspx
The original Mercola article may not remain on the original site, but I will endeavor to keep it on this site as long as I deem it to be appropriate.
Analysis by Dr. Joseph Mercola Fact Checked August 30, 2023

STORY AT-A-GLANCE
- Heartburn pills like omeprazole (Prilosec) are improperly prescribed in up to 70% of cases; they’re also linked to osteoporosis, infections and nutrient deficiencies
- Pepcid (famotidine) is an H2 blocker that can be used to wean off Prilosec and other proton pump inhibitors. It also has very powerful anti-serotonin effects and can be purchased OTC
- One of the most common causes of heartburn is insufficient amounts of stomach acid; consuming sauerkraut or cabbage juice is one way to stimulate your body to produce stomach acid
- While processed foods should be avoided, consuming a Mediterranean diet, which focuses on fruits, healthy fats, lean meats and vegetables, may be as effective as medications in treating acid reflux symptoms
- Ginger tea is beneficial, as ginger accelerates gastric emptying, which, when impaired, contributes to heartburn
- Astaxanthin, deglycyrrhizinated licorice, slippery elm and vitamin D can also help relieve heartburn
Omeprazole (Prilosec), a proton-pump inhibitor (PPI) used to treat heartburn, stomach ulcers and gastroesophageal reflux disease (GERD), is the sixth most common drug prescribed in the U.S.1 Other PPIs include lansoprazole (Prevacid), pantoprazole (Protonix), rabeprazole (AcipHex) and esomeprazole (Nexium) — and they’re often prescribed to reduce stomach acid,2 in a misguided attempt to relieve heartburn.
An estimated 113 million PPI prescriptions are filled worldwide each year,3 but it’s estimated that up to 70% of people taking them shouldn’t be.4 Fortunately, there are many natural methods for heartburn that provide relief without exposing you to the many side effects linked to these popular heartburn pills.
PPIs Are Intrinsically Taken and Should Not Be Used
Initially intended only for treatment of several serious conditions, including bleeding ulcers, severe acid reflux involving damage to the esophagus and Zollinger-Ellison syndrome,5 a rare condition that causes your stomach to produce excess acid, proton pump inhibitors (PPIs) were not meant to be used for everyday heartburn.
Further, they’re only supposed to be taken for a short period of time. Using them long-term can be habit-forming and dangerous, yet they’re commonly prescribed to hospital patients, who often continue taking them after being discharged, with no planned stopping point.6 In fact, up to 80% of patients are inappropriately prescribed a PPI at discharge.7 The consequences can be dire, as PPIs are associated with a number of adverse effects, including:8
- Osteoporosis and related fractures
- Community-acquired pneumonia
- Clostridium difficile colitis
- Cardiovascular morbidity
- Hypomagnesemia, or low magnesium levels
Research shows taking PPIs for more than two years increases your risk of vitamin B12 deficiency,9 while the drugs are also linked to dementia, to the extent that researchers concluded, “The avoidance of PPI medication may prevent the development of dementia.”10
Why PPIs Cause More Harm Than Good
PPIs inhibit the proton pump in your body that produces hydrochloric acid. But excess stomach acid is rarely the primary trigger of heartburn and indigestion. On the contrary, heartburn is typically an indicator you have too little hydrochloric acid, which means if you add a PPI medication, you are only going to exacerbate the problem by decreasing your acid level even more.
Because hydrochloric acid (and pepsin) is necessary to break down protein in your intestinal tract, reduced acid levels affect your body’s ability to absorb nutrients. Without adequate protein breakdown, you also increase your risk of dysbiosis, an imbalance in gut microbiome between harmful and friendly bacteria.
As these undigested protein molecules ferment in your intestines, they become food for pathogens such as Candida, C. difficile and Helicobacter pylori (H. pylori). If you’re currently taking PPIs, be aware that you can develop both tolerance to and dependance on them. As explained in Gastroenterology & Hepatology:11
“The treatment itself may also predispose patients to a need for ongoing therapy. In suppressing acid, PPIs stimulate the body’s feedback loop that tries to reactivate acid secretion.
If the drug is removed, there is a potential risk of rebound hypersecretion, creating a sort of dependency on the drug because the body is acclimated to having acid suppressed. In addition, ongoing feedback stimulation creates a need for ongoing therapy to control symptoms.”
For this reason, it’s important to wean yourself off them gradually to avoid severe rebound symptoms. Do not stop taking PPIs cold turkey. Instead, work with your health care provider to gradually lower the dose you’re taking while simultaneously implementing the natural strategies that follow.
Once you get down to the lowest dose of the PPI, you can start substituting an over-the-counter (OTC) H2 blocker. There are many like Tagamet, Cimetidine or Ranitidine, but Zantac (famotidine) is by far the best and the safest. Then, gradually wean off the H2 blocker over a period of several weeks.
Famotidine is a potent serotonin antagonist and can help those who are taking SSRIs to come off them as they will help lower serotonin levels. Unlike most drugs, it is a relatively safe drug if used long term.

Download this Article Before it Disappears
What Causes Heartburn?
One of the most common causes of heartburn is insufficient amounts of stomach acid. Your body needs stomach acid to properly digest food and absorb nutrients. If you don’t have enough, undigested food in your gastrointestinal tract can lead to indigestion and heartburn.
The leftover food in your gut can also cause bacterial overgrowth, including H. pylori, which is linked to gastritis, peptic ulcer disease and symptoms of acid reflux. As mentioned, if you use PPIs, they cause low stomach acid and, over time, may cause the glands that secrete acid in your stomach to stop working altogether.12
Hiatal hernia, in which the top of your stomach bulges through your diaphragm, is another potential cause of heartburn, as it allows food and acid to back up into your esophagus.13 Physical therapy and chiropractic care can sometimes be effective in resolving this condition.
Food allergies are another potential contributing factor, with caffeine, alcohol and nicotine among the top culprits. However, eating processed foods can also contribute, as it negatively alters your gut microbiome, encouraging the overgrowth of harmful microbes.
Increase Stomach Acid to Resolve Heartburn Naturally
A key strategy to resolving heartburn is to increase the acid content of your stomach. Taking a betaine hydrochloride (also known as trimethyl glycine) supplement, which is available without a prescription, is one way to do so. Take as many as you need to get the slightest burning sensation and then decrease by one capsule. You can also consume 1 tablespoon of raw unfiltered apple cider vinegar in a large glass of water to increase stomach acid.
I also recommend swapping out processed table salt for an unprocessed version like Celtic salt. By consuming enough of the raw material, you will encourage your body to make sufficient amounts of hydrochloric acid (stomach acid) naturally. Fermented vegetables are another dietary addition to focus on if you have heartburn.
Sauerkraut or cabbage juice is among the strongest stimulants for your body to produce stomach acid. It will also provide you with valuable bacteria to help balance and nourish your gut. Having a few teaspoons of fermented cabbage juice from sauerkraut before your meal will do wonders to improve your digestion. Fresh raw cabbage juice can also be very useful to heal resistant ulcers.
What You Eat and Drink Matters
Your diet, including beverages, also plays a role in heartburn symptoms. While processed foods should be avoided, consuming a Mediterranean diet, which focuses on fruits, healthy fats, lean meats and vegetables, may be as effective as PPIs in treating acid reflux symptoms.14
For occasional relief from burning reflux symptoms, alkaline water,15 due to its higher pH level than regular drinking water, may deliver soothing relief by neutralizing the acid in your body. One of the best ways to do this is to use 1 teaspoon of baking soda in 4 ounces of orange juice and stir.
Just make sure that the glass is only half-full as the reaction causes foaming that can cause the glass to overflow. This will help neutralize your stomach acid and ease the burn of acid reflux Another simple strategy is taking frequent sips of water, which can help in the management of GERD symptoms.16
Ginger tea is also useful, as it decreases pressure on the lower esophageal sphincter, helping to prevent heartburn and other gastrointestinal symptoms. Ginger also accelerates gastric emptying which, when impaired, contributes to heartburn,17 and helps suppress H. pylori. Add two or three slices of fresh ginger root to 2 cups of hot water and let it steep for several minutes. Drink it about 20 minutes prior to eating a meal.
The juice of the aloe plant is another natural remedy to help reduce inflammation, which may ease symptoms of acid reflux. Drink about one-half cup of aloe juice before meals. To avoid its laxative effect, look for a brand in which the laxative component has been removed.
Natural Remedies for Heartburn Relief
Getting regular sun exposure to optimize your vitamin D levels is critically important for gut health, as it plays a role in the production of 200 antimicrobial peptides that will help eradicate gut infections. Other remedies that may help you manage occasional bouts of heartburn and other minor reflux symptoms include:
• Astaxanthin — When compared to a placebo, this potent antioxidant was found to reduce symptoms of acid reflux, especially for individuals with pronounced H. pylori infection.18 “Significantly greater reduction of reflux symptoms were detected in patients treated with the highest dose of the natural antioxidant astaxanthin” compared to placebo, the study found.
Researchers concluded a daily dose of 40 milligrams of astaxanthin was effective for reflux reduction.
• Deglycyrrhizinated licorice root — Deglycyrrhizinated licorice (DGL) may also be helpful because it helps block inflammatory prostaglandins. One study found DGL protected gastric mucosa and relieved GERD symptoms better than acid-suppressive drugs.19
Licorice must be approached cautiously, however, because it contains the active metabolite glycyrrhiza, which at high doses can affect your adrenal glands, cause muscle weakness or numbness and raise your blood pressure.
Licorice is contraindicated if you’re on diuretics or stimulant laxatives. Women on hormone therapy, who have estrogen-dependent cancers or reproductive conditions like endometriosis, should also avoid it.
• Glutamine — The amino acid glutamine has been shown to address gastrointestinal damage caused by H. pylori. According to Susan Hagen, associate professor of surgery at Harvard Medical School, who’s studied the issue:20
“Gastric damage develops when the bacteria weakens the stomach’s protective mucous coating, damages cells and elicits a robust immune response that is ineffective at ridding the infection … Our findings suggest that extra glutamine in the diet could protect against gastric damage caused by H. pylori.”
Glutamine is found in many foods, including beef, chicken, dairy products, eggs, fish and selected fruits and vegetables. L-glutamine is widely available as a supplement.
• Papaya (papain supplement) or Pineapple (bromelain supplement) — Papaya contains papain, an enzyme useful for breaking down both protein and carbohydrates. Bromelain is a proteolytic enzyme found in pineapple, and like papain, helps digest proteins. Bromelain also promotes anti-inflammatory activity and helps you maintain regular bowel movements.
• Slippery elm — Slippery elm coats and soothes your mouth, throat, stomach and intestines, and contains antioxidants that may help address inflammatory bowel conditions.
Because it stimulates nerve endings in your gastrointestinal tract, it is useful for increasing mucus secretion, which has a protective effect against ulcers and excess acidity. Try mixing 1 to 2 tablespoons of slippery elm powder with water, consumed after meals and before bedtime.21
Other natural compounds, including curcumin, pectin and peppermint oil, have also been found to improve gastrointestinal symptoms and gut microbes while reducing the need for reflux medications.22 A dietary supplement containing melatonin, l-tryptophan, vitamin B6, folic acid, vitamin B12, methionine and betaine was also superior to omeprazole in the treatment of GERD.23
So, when it comes to finding relief from symptoms and support to address the underlying causes of most heartburn cases, there are numerous natural options at your disposal. These, combined with a whole food diet and limited processed foods, will help heal your gut and put an end to heartburn naturally.
- 1 Pharmacy (Basel). 2018 Jun; 6(2): 43., Figure 1
- 2 Harvard Health Publishing September 30, 2021
- 3 US Pharm. 2019:44(12):25-31
- 4, 6 Fed Pract. 2017 Feb; 34(2): 19–23
- 5 Arch Intern Med. 2010 May 10;170(9):747-8. doi: 10.1001/archinternmed.2010.64
- 7 BMC Geriatr. 2022; 22: 306
- 8 BMJ Open. 2020; 10(11): e040473
- 9 JAMA 2013;310(22):2435-2442
- 10 JAMA Neurol. 2016;73(4):410-416. doi: 10.1001/jamaneurol.2015.4791
- 11 Gastroenterol Hepatol (N Y). 2008 May; 4(5): 322–325
- 12 Cleveland Clinic, Hypochlorhydria
- 13 Mayo Clinic, Hiatal Hernia
- 14, 15 Journal of the American Medical Association Otolaryngology – Head & Neck Surgery September 7, 2017; doi: 10.1001/jamaoto.2017.1454
- 16 Case Rep Gastrointest Med. 2019; 2019: 9205259
- 17 Food Sci Nutr. 2019 Jan; 7(1): 96–108., Gastric Emptying and Dyspepsia
- 18 Phytomedicine June 2008; 15(6-7): 391-9
- 19 Journal of the Australian Traditional-Medicine Society (Vol. 23, Issue 2)
- 20 The Harvard Gazette May 15, 2009
- 21 University of Wisconsin Integrative Medicine, An Integrative Approach to GERD
- 22 Nutr Res. 2020 Apr;76:37-51. doi: 10.1016/j.nutres.2020.02.008. Epub 2020 Feb 8
- 23 Journal of Pineal Research Oct 2006, 41(3):195-200